Disorders of Cardiac Rate and Rhythm
Richard Sterba
An evaluation of abnormalities in the cardiac rate or rhythm may be initiated during a patient interview, auscultation of the heart, or palpation of the peripheral pulses. We rely on electrocardiogram (EKG) to make the definitive diagnosis of clinically suspected abnormalities. Electrocardiography, although simple and inexpensive to perform, provides a great deal of information about the components and function of the electrical system of the heart. Information regarding atrial conduction properties or atrial hypertrophy can be identified by studying the Pwave morphology. Cardiac conduction from the sinus node through the atrium, atrioventricular (AV) node, and His-Purkinje system occurs during the PR interval. Therefore, abnormalities in the conduction from the
atrium to the ventricle can be identified by abnormalities in the duration of the PR interval. Change in the shape or size of the P wave is present if atrial hypertrophy exists. The QRS complex represents ventricular depolarization, and therefore contains information regarding intraventricular conduction and ventricular hypertrophy. Both right and left ventricular hypertrophies have well-described changes in their QRS waveform and voltage. The QT interval records ventricular repolarization.
atrium to the ventricle can be identified by abnormalities in the duration of the PR interval. Change in the shape or size of the P wave is present if atrial hypertrophy exists. The QRS complex represents ventricular depolarization, and therefore contains information regarding intraventricular conduction and ventricular hypertrophy. Both right and left ventricular hypertrophies have well-described changes in their QRS waveform and voltage. The QT interval records ventricular repolarization.
VARIABILITY IN SINUS RHYTHM
The heart rate generated by the sinus node varies with age. Newborns typically have a faster heart rate, in the range of 100 to 180 beats/minute. By the age of 5 years, the heart rate generally decreases to approximately 60 to 120 beats/minute in a quiet and restful situation. Through adolescence and early adulthood, the sinus rate falls to the normal adult range, and typically varies between 50 and 100 beats/minute. The sinus node and heart rate follow signals from the body to generate an appropriate cardiac output. In stressful situations, the heart rate should increase. During sleep or rest it will decrease. To diagnose the abnormalities of the heart rate correctly, one must be aware of the outside influences and disease states that can affect the heart rate.
Sinus arrhythmia is the normal variation that occurs in the heart rate while a patient is breathing. Some parents who check their child’s heart rate while the child is asleep will notice this subtle variation in pulse rate and be concerned that extra heartbeats are present. Although called sinus arrhythmia, it is a normal phenomenon, and should not be interpreted as an abnormality in sinus node function.
Sinus bradycardia is the most common type of bradycardia seen in pediatrics. Sinus bradycardia can be seen in well-trained athletes. Sinus bradycardia is not uncommonly seen in patients with hypothyroidism, or those with eating disorders, such as anorexia. True sinus node dysfunction resulting in significant sinus bradycardia and its symptoms is unusual in pediatric patients. This is discussed further in the subsequent section on Bradycardia.
Normal heart rates above the expected normal ranges are labeled sinus tachycardia. Sinus tachycardia can be seen at rates over 200 beats/minute in expected situations. This extreme sinus tachycardia can be seen in patients who are very febrile, or during peak exercise. Patients with critical diseases who are receiving inotropic agents can also have an elevated sinus rate. There is generally a subtle variation in the R-R interval during sinus tachycardia, and this phenomenon is not commonly seen in patients with true supraventricular tachycardia (SVT).
TACHYCARDIAS
Tachycardias, typically paroxysmal tachycardias, are the most common significant arrhythmias seen in pediatric patients. In general, heart rates faster than 220 beats/minute should be considered abnormal. Sinus, supraventricular, and ventricular tachycardias cannot always be differentiated on the basis of their clinical presentation alone. Therefore, a 12-lead EKG is an important tool in defining the specific type of tachycardia in an individual patient.
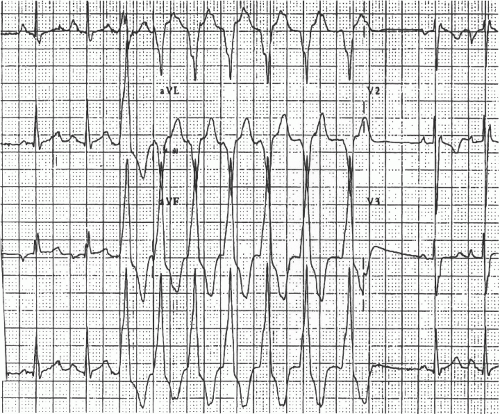
A rapid, regular, narrow QRS rhythm is called supraventricular tachycardia, and is the most common abnormal tachycardia seen in pediatrics (Fig. 27.1). SVT accounts for at least 90% of the cases of abnormal tachycardia. SVT is typically paroxysmal. This statement means that the tachycardia has a sudden onset and offset, and is not consistently present. Pediatric patients older than 5 years can often describe the sudden onset of tachycardia quite well. The electrophysiologic mechanisms responsible for SVT include AV re-entrant tachycardia (tachycardia secondary to an accessory AV connection) and AV nodal re-entry tachycardia. These two mechanisms account for approximately 90% of the cases of SVT seen in a pediatric electrophysiologic practice. Less commonly, ectopic atrial tachycardia, atrial flutter, or junctional tachycardia is seen. Patients with paroxysmal SVT may describe the sensation as a fast heart rate that starts suddenly and stops suddenly. In most cases, arrhythmia is not life threatening, and can be characterized as a nuisance. Should an episode of SVT last for a significant time, generally hours, hemodynamic
compromise can develop, and the patient may present critically ill. Some newborns who present with SVT and patients who have SVT in association with significant structural heart disease can present in a more compromised condition. Infants and newborns present with critical illness because the parents are not aware of the SVT and notice signs such as poor feeding and poor color that generally occur later in the episode of supraventricular tachycardia. The rate of SVT in newborns ranges from 240 to 300 beats/minute. The heart rate during SVT in children and adolescents ranges from 180 to 250 beats/minute. Because most patients with SVT have a structurally normal heart, they usually do not present with cardiac collapse or syncope, but rather with the sensation of a rapid heartbeat that is frequently associated with chest tightness. Tachycardia may be brought to the attention of a primary care physician only after a prolonged episode or frequent episodes. Patients with symptoms suggestive of SVT would benefit from a cardiac consultation.
compromise can develop, and the patient may present critically ill. Some newborns who present with SVT and patients who have SVT in association with significant structural heart disease can present in a more compromised condition. Infants and newborns present with critical illness because the parents are not aware of the SVT and notice signs such as poor feeding and poor color that generally occur later in the episode of supraventricular tachycardia. The rate of SVT in newborns ranges from 240 to 300 beats/minute. The heart rate during SVT in children and adolescents ranges from 180 to 250 beats/minute. Because most patients with SVT have a structurally normal heart, they usually do not present with cardiac collapse or syncope, but rather with the sensation of a rapid heartbeat that is frequently associated with chest tightness. Tachycardia may be brought to the attention of a primary care physician only after a prolonged episode or frequent episodes. Patients with symptoms suggestive of SVT would benefit from a cardiac consultation.
The acute treatment of SVT depends on the patient’s presentation. Critically ill patients should be treated appropriately, with placement of an intravenous line and infusion of adenosine. If intravenous access is not available, the patient can be returned to sinus rhythm with synchronized cardioversion. In more stable patients, the use of vagal maneuvers, such as the Valsalva maneuver, or diving reflex can terminate episodes of SVT. To induce a vagal stimulus, one can also place a washcloth in a basin of ice-cold water and then firmly press the chilled washcloth over the patient’s face. Vagal maneuvers terminate SVT by slowing the conduction through the AV node, which is a critical part of the re-entrant circuit. The preferred medical treatment of an acute episode of SVT is intravenous adenosine. The recommended dose is 0.1 mg/kg bolus preferably through a centrally placed intravenous line. This medication terminates SVT by blocking the conduction through the AV node. Again, the AV node is a critical portion of the re-entry tachycardia loop. Tachycardia will terminate abruptly, and it is not uncommon to see a significant pause in the heart rate, and then perhaps in the sinus tachycardia. If tachycardia recurs after an infusion of adenosine, other antiarrhythmic medications (e.g., digoxin, β-blockers, intravenous procainamide, or other antiarrhythmics) can be added to the antiarrhythmic regimen to help maintain sinus rhythm. Transesophageal atrial pacing can also be performed to terminate SVT. This method is an excellent alternative for patients who have a tachycardia such as atrial flutter or intra-atrial re-entry tachycardia.
The long-term treatment of SVT depends on its mechanisms. Three options can generally be offered to the family and patients who have SVT. Patients with hemodynamically uncompromising, infrequent, and short episodes of tachycardia can be managed with observation alone. They are instructed in the use of vagal maneuvers should episodes of tachycardia occur. The second option is antiarrhythmic medications. Medications commonly used in pediatrics include β-blockers, digoxin, calcium channel blockers, flecainide, and sotalol. The typical re-entrant SVTs seen outside
the newborn age will not disappear as the child grows older. For that reason, many families prefer a more invasive approach with the use of an electrophysiologic procedure and ablation of the offending cardiac tissue. During this type of procedure, a catheter is positioned in the heart near the accessory or abnormal electrical tissue that is the underlying substrate for the arrhythmia. Myocardial destruction by tissue modification or destruction with heating (radiofrequency [RF] ablation) or cryoblation can destroy the abnormal electrical tissue and render the tachycardia noninducible. Many patients are cured after this type of procedure. The risk is considered low, and major complications develop in <2% of the procedures. SVT in pediatric patients should be considered a nuisance that is typically not life threatening, and can be controlled well either with medication or with ablation procedures.
the newborn age will not disappear as the child grows older. For that reason, many families prefer a more invasive approach with the use of an electrophysiologic procedure and ablation of the offending cardiac tissue. During this type of procedure, a catheter is positioned in the heart near the accessory or abnormal electrical tissue that is the underlying substrate for the arrhythmia. Myocardial destruction by tissue modification or destruction with heating (radiofrequency [RF] ablation) or cryoblation can destroy the abnormal electrical tissue and render the tachycardia noninducible. Many patients are cured after this type of procedure. The risk is considered low, and major complications develop in <2% of the procedures. SVT in pediatric patients should be considered a nuisance that is typically not life threatening, and can be controlled well either with medication or with ablation procedures.
Other SVTs include atrial flutter, atrial fibrillation, ectopic atrial tachycardia, and junctional tachycardias. Adenosine is not effective in terminating these arrhythmias, because the AV node is not a critical part of the tachycardia circuit. In an acute situation, these types of SVTs can be terminated with intravenous medications such as procainamide or amiodarone. They respond nicely to cardioversion or atrial overdrive pacing. Many of these arrhythmia circuits can also be destroyed during an ablation procedure.
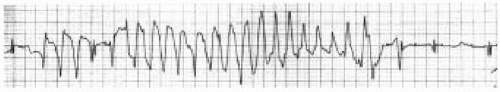
Ventricular tachycardia (Fig. 27.2) is a rapid, regular, wide QRS tachycardia that occurs infrequently in pediatric patients. Approximately 5% of patients who present with paroxysmal tachycardia have ventricular tachycardia as the underlying mechanism. Although SVT can be considered a nuisance in children, ventricular tachycardia should never be considered a nuisance, and should be considered a potentially life-threatening event. These patients require careful evaluation in an appropriate center where definitive studies can be performed to rule out structural heart defects, cardiomyopathic states, or a possible tumor in the heart. Patients presenting with ventricular tachycardia may respond to intravenous lidocaine, procainamide, or amiodarone. In critically ill patients, synchronized cardioversion should be performed. The long-term treatment of patients with ventricular tachycardia may include medications, RF ablation, or perhaps implantation of a defibrillator.
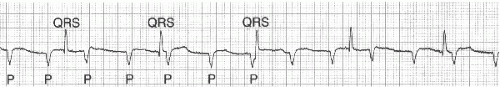
Ventricular fibrillation can certainly occur in pediatric patients. It is typically seen in patients with electrocardiographic abnormalities such as a long QT interval (Fig. 27.3) or a Brugada syndrome. Cardiomyopathies or structural heart abnormalities that cause significant ventricular dysfunction are also associated with ventricular fibrillation or ventricular tachycardia that degenerates into ventricular fibrillation. Patients with ventricular fibrillation require cardiopulmonary resuscitation (CPR), immediate defibrillation, and transfer to an appropriate center for further evaluation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree