Diseases of the Aorta
Robert J. Siegel
Kirsten Tolstrup
Most chronic disorders of the aorta are without symptoms. Approximately 40% of patients with ascending aortic aneurysm are asymptomatic, as are most patients with Marfan syndrome, pseudoaneurysm, and sinus of Valsalva aneurysms.
Aortic atheromatosis is also asymptomatic until acutely manifested with a transient ischemic attack, stroke, or peripheral embolism.
Acute aortic disorders (aortic dissection and rupture, intramural hematoma, and penetrating aortic ulcer) generally present with severe chest pain that usually radiates to the back, retrosternal or interscapular pain, dyspnea, dysphagia, or extremity pain:
Aortic dissection, rupture of aortic sinus of Valsalva, or trauma with flail aortic cusps may result in severe acute aortic regurgitation (AR) and acute severe heart failure.
The physical examination in chronic or acute disorders of the aorta is nonspecific, nonsensitive, and therefore of limited diagnostic value.
Class I Indications for Echocardiography in Aortic Diseases
Transthoracic echocardiography (TTE) and particularly transesophageal echocardiography (TEE) are of important diagnostic value in patients with aortic diseases (1,2,3,4,5) (Table 14.1). Recent guidelines were developed for specific genetic conditions associated with aortic aneurysms and dissections (6) (Table 14.2).
Imaging of the Aorta by M-Mode, Two-dimensional, and Doppler Echocardiography
Ascending Aorta: Best Imaging Planes
The ascending aorta begins at the aortic valve and extends 5 to 6 cm to the junction with the aortic arch.
Transthoracic Echocardiography
M-mode parasternal long- and short-axis view by two-dimensional (2D) guidance.
Two-dimensional left parasternal long- and short-axis views and suprasternal view.
Apical five-chamber view with anterior angulation of the transducer.
Right parasternal long-axis view.
Sometimes subcostal imaging.
Enhance imaging of the superior portion of the ascending aorta by moving the transducer to higher interspaces (origin of aorta beneath third left intercostal space [ICS] and courses toward second right ICS).
Enhance image quality with steeper left lateral decubitus position (brings aorta closer to chest wall).
Apical five-chamber view allows assessment of flow by pulsed Doppler.
Suprasternal view allows high-quality pulsed Doppler antegrade flow.
Transesophageal Echocardiography
Multiplane probe at an angle of 120 to 135 degrees generally allows assessment of the long axis of the aorta from the aortic valve to just below the innominate artery (may image up to 10 cm of the aorta).
Short-axis views at 0 to 30 degrees. The aortic segments just beneath the arch cannot be visualized due to the trachea being interposed between the ascending aorta and the esophagus.
A deep transgastric approach can visualize the ascending aorta. Multiplane imaging at 0, 90, and 120 degrees allows images of the proximal 3 to 5 cm of the ascending aorta.
Epiaortic Imaging (Intraoperative)
Imaging of the ascending aorta by direct application of the transducer on the aorta in a sterile sheath.
Table 14.1 Class I indications for echocardiography in thoracic aortic diseases
Aortic dissection, diagnosis, location, and extent.*
Aortic aneurysm.
Aortic intramural hematoma.*
Aortic rupture.*
Aortic root dilatation in Marfan syndrome or other connective tissue syndromes.
Degenerative or traumatic aortic disease with clinical atheroembolism.*
Follow-up of aortic dissection, especially when complication or progression is suspected.*
First-degree relative of a patient with Marfan syndrome or other connective tissue disorder.
The hemodynamically unstable multiple-injury patient without obvious chest trauma but with a mechanism of injury suggesting potential cardiac or aortic injury (deceleration or crush).*
Widening of the mediastinum and postinjury-suspected aortic injury.*
Follow-up study on victims of serious blunt or penetrating trauma.
Surgical repair of aortic dissection with possible aortic valve involvement and valve replacement requiring homografts or coronary reimplantation (intraoperative).
*Transesophageal echocardiography is the sonographic technique of choice for these conditions.
Primarily used to reduce intraoperative stroke risk by identifying sites of significant atherosclerosis or atheroma and to choose sites for aortic cannulation or cross-clamping.
More accurate than TEE for detection and assessment of ascending aortic atherosclerosis.
Sensitivity and specificity for ascending atherosclerosis are 100%, compared to TEE sensitivity and specificity of 100% and 60%, respectively.
Pitfalls
Needs to be done intraoperatively and under sterile conditions.
Potential for contamination of surgical field.
Logistics are more complex than intraoperative TEE.
Need to use stand-off for the epiaortic probe to visualize the aortic wall (e.g., sterile, saline-filled bag or glove).
Aortic Arch: Best Imaging Planes
The aortic arch begins beneath the upper edge of the second right ICS and joins the descending thoracic aorta posterior to the fourth ICS.
Table 14.2 Class I recommendations for echocardiographic imaging of the aorta in genetic syndromes (Marfan syndrome, Loeys-Dietz syndrome), familial thoracic aortic aneurysm and dissections, and bicuspid aortic valve and associated congenital variants in adults | ||
|---|---|---|
|
Transthoracic Echocardiography
TTE imaging is best from the suprasternal notch. By scanning with the transducer inferoposterolateral (left), the imaging plane aligns with the long axis of the aortic arch (left carotid to the right, innominate artery to the left). The right pulmonary artery is beneath the aortic arch.
Nearness of the suprasternal notch to the aortic arch makes imaging routinely feasible, and left carotid and subclavian arteries are detected in 90% and innominate in 60% of cases (5), with both longitudinal and transverse planes.
Right parasternal view may be useful.
Right or left supraclavicular imaging of the arch, or both, is also sometimes feasible.
Normal systolic flow away from transducer is followed by early diastolic reversal, mid-diastolic antegrade flow, and again reversal of flow at end diastole.
Low wall filters may be needed to detect a normal Doppler flow pattern due to low-velocity diastolic flow.
Transesophageal Echocardiography
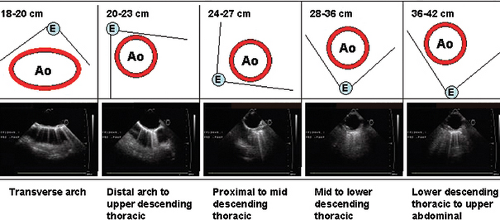
Esophagus posterior to the aorta at the level of arch and anterior to the aorta at the level of the mid- to distal thoracic aorta (Fig. 14.1).
High esophageal imaging at 0 and 130 degrees with posterior and medial flexion yields longitudinal views of arch.
Other multiplane views yield cross-sectional views at multiple levels.
Epiaortic Imaging (Intraoperative)
Intraoperative epiaortic imaging is as described in the Ascending Aorta discussion.
Descending Thoracic Aorta: Best Imaging Planes
The descending thoracic aorta begins at the lower edge of the fourth left ICS.
Transthoracic Echocardiography
Parasternal long axis allows short-axis view of the descending thoracic aorta seen beneath the heart at the site of the atrioventricular groove.
Longitudinal view of thoracic aorta is obtained by lateral angulation and rightward rotation of transducer (feasible in >65% of cases).
Apical two-chamber view with medial tilt of transducer.
Subcostal view allows imaging of distal descending aorta and proximal abdominal aorta.
With left pleural effusion, imaging thoracic aorta from right lateral decubitus position is feasible.
Doppler is best done from the suprasternal notch due to parallel flow.
Transesophageal Echocardiography
Aorta is posterolateral and posterior to the esophagus (Fig. 14.1).
Short-axis plane is seen at 0 degrees and long-axis plane at 90 degrees.
Comprehensive imaging from the abdominal aorta to the aortic arch is often best accomplished during continuous or preferably stepwise “pull-back” of the probe from the transgastric position, with the probe inserted to 45 to 50 cm from the bite-block to approximately 15 to 20 cm from the bite-block. Stepwise pull-back allows visualization of the entire aorta by performing short- and long-axis views or using an X-plane feature at intervals of ≤5 cm.
During pull-back, rotation is required to keep short-axis aortic images in the center of the screen due to aorta becoming more anterior and rightward as the probe is pulled in a cephalad direction.
Flow is perpendicular to ultrasound. Thus, it is not possible to obtain accurate maximal Doppler flow velocities of aorta.
In the descending aorta in transverse view (0 degrees), color flow Doppler reflects counterclockwise swishing direction of blood flow. In a longitudinal view (90 degrees), color flow Doppler reveals a red pattern toward the head and blue toward the diaphragm.
Intravascular Ultrasound
Intravascular ultrasound (IVUS) uses catheters with high-frequency (20–40 MHz) miniature transducers to image within blood vessels (3).
IVUS is used more commonly to image the descending thoracic aorta.
IVUS yields high-resolution images.
IVUS has documented utility in assessment of aortic dissection, trauma, aneurysm, and coarctation.
IVUS is used for assessment and deployment of endovascular grafts for aneurysm as well as dissection.
Pitfalls
IVUS has no Doppler capability, no steerability, and limited penetration due to high frequency.
It requires fluoroscopy in the catheterization laboratory or a specialized operating room.
TTE should be the first choice in clinically stable situations to assess the ascending aorta.
Three-dimensional Transesophageal Echocardiography
Real-time three-dimensional (RT3D) TEE can be acquired at each level of the aorta. Unlike for 2D TEE imaging, it is only necessary to locate one imaging plane, such as a long-axis view. Manipulation of the picture will provide the other views. The images may be obtained utilizing zoom function, live 3D, or by acquisition of a full-volume scan.
Diagnostic Value of Echocardiography in Aortic Diseases
Aortic Aneurysm
Definition
Aortic aneurysm is the dilatation of an aortic segment ≥1.5 times the normal diameter. The intimal, media, and adventitia all are present.
Normal Diameters
Aortic annulus: 2.6 ± 0.3 cm in males and 2.3 ± 0.2 cm in females.
Sinus of Valsalva: 3.4 ± 0.3 cm in males and 3.0 ± 0.3 cm in females.
Ascending aorta: <3.7 cm, 2.9 ± 0.3 cm in males, and 2.6 ± 0.3 cm in females.
Descending aorta: 1.0 to 1.6 cm/m.
Nomograms have been developed for the sinuses of Valsalva relating the dimension to age and body surface area (7) (Fig. 14.2). In addition, one may use the diameter related to the height of the patient. Studies have showed that if the maximal cross-sectional area in square centimeters of the ascending aorta or root divided by the patient’s height in meters exceeds a ratio of 10, surgical repair is reasonable (8).
Types
Fusiform: Uniform dilatation of entire aortic circumference (75% of aneurysms).
Saccular: Localized expansion resulting in a balloon-type (eccentric) dilatation of a segment of the wall with a narrow neck. Often contains clot within aortic lumen.
Etiology
Ascending Aorta
Etiology of an aortic aneurysm in the ascending aorta includes atherosclerosis (most common), hypertension, Marfan syndrome, Loeys-Dietz syndrome, Ehlers-Danlos syndrome, bicuspid aortic valve, aortic coarctation, infection (syphilis, tuberculosis, sal-monella), aortitis (Takayasu arteritis, giant cell arteritis, Behçet disease, ankylosing spondylitis), Turner and Noonan syndromes, familial aortic root dilatation, and annuloaortic ectasia.
Arch and Descending Aorta
The etiology of an aortic aneurysm in the arch and descending aorta are the same as for the ascending aorta.
Key Diagnostic Features
TTE is adequate to detect and characterize ascending aortic aneurysms located at the sinuses and sinotubular positions (2,4,5).
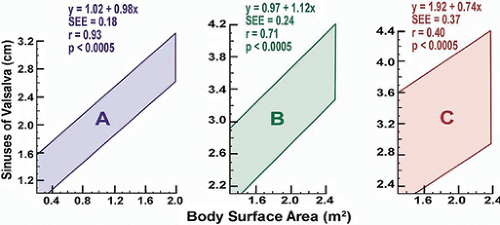
Figure 14.2: Nomogram relating the aortic diameter to body surface area for three age groups (A, <20 years, B, 20 to 40 years, C, >40 years).
TEE is more accurate than TTE in detecting distal ascending aortic aneurysm and aneurysm of the arch and descending aorta:
Accurate for assessment of size and defining underlying aortic wall pathology (sclerosis, calcification, atherosclerosis, dissection).
Dilatation of aorta.
Systolic expansion of aorta.
Left atrial compression.
Aortic valve midsystolic closure.
Assessment of the presence and severity of associated AR.
TEE transverse (0 degrees for descending aorta) and longitudinal planes (90 degrees) generally are best to define aneurysm shape, size, morphology, extent, and plaque size as well as thrombus. 3D TEE imaging may improve the spatial morphologic description of the aneurysm and atherosclerotic plaques.
Prognosis
Five-year survival is related to the diameter of the ascending aorta: ≤6 cm is 61%, and >6 cm is 38%. The 5-year survival for a descending thoracic aortic aneurysm with a diameter >6 cm is 39%.
In atherosclerotic aneurysm, the need for surgery has to be individualized due to comorbid diseases.
The operative mortality rate ranges from 2% to 21%, and there is a high risk of rupture with aneurysm >6 cm.
Pitfalls
Transthoracic Echocardiography
TTE has limited sensitivity and specificity for aortic dimension due to tangential imaging and for aortic wall pathology due to distance from the transducer, calcification in aorta, and limited windows (9).
Transesophageal Echocardiography
TEE does not usually allow visualization of aorta adjacent to the trachea or the innominate artery and much of the abdominal aorta.
Marfan Syndrome
Definition
Marfan syndrome includes abnormalities of the skeleton, eye, cardiovascular system, pulmonary system, skin, central nervous system, and family history.
Etiology
Marfan syndrome is an autosomal-dominant connective tissue disorder due to FBN1 mutations resulting in abnormal fibrillin.
Approximately 25% of cases have no family history.
Echocardiographic Key Diagnostic Features
Major Criteria
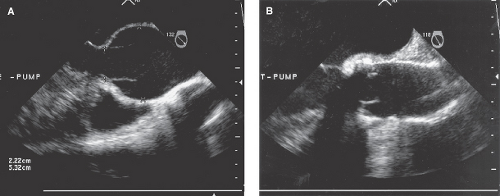
Dilatation of the ascending aorta with or without AR and involving at least the sinuses of Valsalva (Fig. 14.3):
Initially affects most proximal aorta.
In children and adults ≤45 years of age, aorta rarely dilates distal to root.
AR secondary to dilatation of aortic sinotubular ridge.
AR is rare when the ascending aorta is ≤4 cm.
AR is almost always present if the ascending aorta is >6 cm.
Dissection of the ascending aorta:
Dissection begins in root and often progresses to iliacs.
Retrograde dissection can involve coronaries and can rupture into pericardium.
Minor Criteria
Mitral valve prolapse with or without mitral valve regurgitation.
Dilatation of the main pulmonary artery in the absence of valvular or peripheral pulmonic stenosis or any other obvious cause in patients <40 years of age.
Calcification of the mitral annulus in patients <40 years of age
Dilatation or dissection of the descending thoracic or abdominal aorta in patients <50 years of age.
For the cardiovascular system to be involved, a major criterion or only one of the minor criteria must be present.
Pregnancy
Pregnancy is contraindicated if aorta measures >4 cm due to increased risk of aortic dissection (Table 14.3).
Prognosis
Life expectancy is primarily determined by cardiovascular involvement, especially the aorta.
Beta-blockade reduces the progression of aortic root dilatation in some patients.
Prophylactic aortic root replacement improves prognosis.
Low risk if aorta is <4 cm.
High risk if aorta is >5 cm.
Table 14.3 Aortic root dimension in marfan syndrome and risk
Low Risk (<4 cm)
Moderate Risk (≥4 cm)
High Risk* (>5 cm)
Pregnancy not contraindicated.
Pregnancy contraindicated due to risk of aortic dissection or rupture. 
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access