Chapter 10 Discontinuation of Mechanical Ventilation
2 When should patients receiving mechanical ventilation be assessed for ventilator discontinuation?
 Lung injury stable or resolving
Lung injury stable or resolving
 Adequate gas exchange with low positive end-expiratory pressure (PEEP) and fraction of inspired oxygen (FiO2) requirements (e.g., PEEP < 5-8 cm H2O, FiO2 < 0.4-0.5)
Adequate gas exchange with low positive end-expiratory pressure (PEEP) and fraction of inspired oxygen (FiO2) requirements (e.g., PEEP < 5-8 cm H2O, FiO2 < 0.4-0.5)
 Hemodynamic stability (e.g., not requiring pressors, no serious arrhythmias)
Hemodynamic stability (e.g., not requiring pressors, no serious arrhythmias)
3 How, exactly, should this assessment be done?
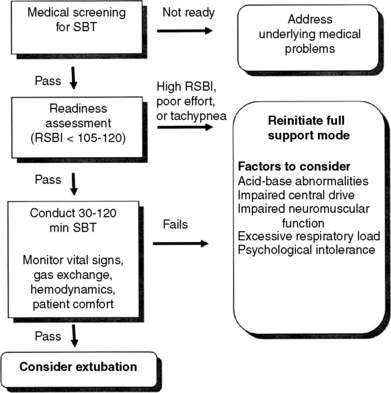
As of yet, no systematic weaning protocol has been agreed on. However, most protocols have a stepwise assessment that varies in the details. The above criteria should be assessed daily as a wean screen. For the patients who pass the daily wean screen, there is first an initial brief trial or readiness assessment during which patients are closely observed for 1 to 5 minutes while receiving minimal or no support (continuous positive airway pressure [CPAP] ≤ 5 cm H2O, T-piece trial, 5 to 7 cm H2O pressure support from the ventilator, or automatic tube compensation) to assess their ability to undergo a formal spontaneous breathing trial (SBT). If the patient does well during the readiness assessment, an SBT is performed for between 30 and 120 minutes. During this time patients are closely monitored for signs of respiratory insufficiency, hemodynamic deterioration, problems with gas exchange, or patient discomfort. Full ventilatory support is promptly reinitiated if problems develop. Successfully completing an SBT is highly predictive of successful ventilator discontinuation. These steps are illustrated in Figure 10-1.
4 What is the rapid shallow breathing index (RSBI)? What does it predict?
The RSBI is calculated by using the following formula:
5 To which mode should the ventilator be set during the SBT?
 T-piece circuit that provides a constant flow of oxygen past the endotracheal tube with an extension downstream to prevent entrainment of room air
T-piece circuit that provides a constant flow of oxygen past the endotracheal tube with an extension downstream to prevent entrainment of room air
 Low levels of pressure support ventilation of 5 to 8 cm H2O
Low levels of pressure support ventilation of 5 to 8 cm H2O
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree