Fecal Occult Blood (FOB) Testing:
Links: Info & Types | iFOBT | Guiac Based | Because of the possibility of bleeding from trauma, it is not known if a positive result from a digital rectal exam (DRE) differs from a positive test of spontaneously evacuated stool. FOB testing doesn’t pick up early lesions and benign polyps, for that, we would still need to do some sort of imaging. A single FOBT (Hemoccult II) obtained following a DRE will miss cancer 95% of the time (Ann Int Med 2005;142:81-5). DRE should still be the first test, as compliance is lacking with FOBT with spontaneously passed stool. If the digitally obtained stool is negative, still need FOBT X3 from spontaneously passed stools (6x = 2 samples from 3 stools), as this is the only route proven to reduce colorectal Ca mortality by 15-33% (JAMA 2003;289:10). Alternatively, guidelines from the Am Ca Soc & Am Col Gastro say a screening colonoscopy can be performed q10yrs with much better compliance. Colorectal cancer screening by biennial FOBT reduces colorectal cancer mortality (Gastroenterology 2004;126:1674-1680), the cumulative risk for a positive FOBT result was 4.1%. The positive predictive value was 11.5% for colorectal cancer, 16.8% for large adenoma, and 11.4% for small adenoma. Having FOBT screening at least once reduced the risk of colorectal mortality by one-third. A meta-analysis that included 245,217 persons were followed up for more than 3 million pt years with annual FOBT found that overall, there was a 13% relative reduction in colorectal cancer mortality, but no reduction in all-cause mortality in pt’s screened (Am J Gastroenterol 2006;101:380-4). The 5-year results of the UK Bowel Cancer Screening Pilot study show that biennial use of the FOBT decreases emergency presentations (by 15.8%) for colorectal cancer, emergency surgeries (by 47.4%) and dramatically reduces 30-day postoperative mortality (Gut 2008;57:218)….compliance with FOB testing were 56.8% in round 1 and 51.9% in round 2.
3 classes of FOBTs: heme-porphyrin tests, immunochemical tests and guaiac-based tests.
1. Heme-porphyrin: HemoQuant, measures hemoglobin-derived porphyrins, allowing quantitative measurement of hemoglobin in stool. Its use is limited because it has a higher rate of false-positive results, is expensive, and requires lab time. Unlike the guaiac-based tests, dietary peroxidases do not cause false-positive results with the heme-porphyrin test.
2. Immunochemical (iFOBT) = Fecal Immunochemical Testing (FIT): HemeSelect, IMSTOB, ClearView UTLRA and FECA-EIA, detect intact human Hb. Fecal immunochemical tests (FIT). Immunochemical fecal occult blood tests were developed to improve specificity and eliminate the need for bowel preparation or dietary restriction. They use 1 or more monoclonal Ab’s or polyclonal Ab’s to detect human hemoglobin. These tests are more specific for bleeding from the lower GI tract, and consumption of red meat or dietary peroxidases does not produce false-positive results. They do not detect digested Hb, so they are not able to detect bleeding from upper GI sources. Even though more expensive, these fecal occult blood tests are thought to have higher compliance rates and be more accurate than guaiac-based tests. A recent study findings indicate that this does not actually hold true in the general clinic setting.
• Out of 3,000 pt’s, 47% returned the guaiac cards and 48% of 3,000 returned the immunochemical-based tests (Am J Med 2003;115:111-114). ClearView UTLRA is sensitive to 50 ug Hb/g (vs 1,500 with Hemoccult SENSA) with no dietary restrictions.
• A study on 1000 ambulatory adults undergoing elective colonoscopy concluded that quantitative immunochemical FOBT appears to have reasonable sensitivity and specificity for a screening test and some people might use it to select pt’s for colonoscopy (Ann Intern Med 2007;146:244-55)…. sensitivity of 67% and specificity of 91% for advanced neoplasia….for cancer, sensitivity and specificity were 94% and 88%.
• Experts say that the fecal occult blood test, which is more convenient, less invasive, and relatively inexpensive, could be an important next step in expanding colorectal cancer screening as only 52% of adults >50 have had a sigmoidoscopy or colonoscopy as of 2004 (Ann Intern Med. 2007;146:244-255)… drawback, however it that it doesn’t pick up early lesions and benign polyps, for that, we would still need to do some sort of imaging.
• An immunochemistry test for fecal occult blood is significantly more accurate in detecting left-sided colorectal cancer than conventional testing according to a prospective study with 5,841 pt’s with an average risk for colorectal cancer (J Natl Cancer Inst. 2007;99:1-9)(had 82% sensitivity versus 64.3% with an enhanced-sensitivity guaiac test, the specificity approached 100%)….”annual testing might be competitive with a colonoscopy screening program”….for advanced colonic neoplasm, for the immunochemistry test was 29.9% vs 24% with the unrehydrated guaiac test.
• iFOBT’s better sensitivity but lower specificity for detecting cancer (2.3% less) and advanced adenomas (1.3% less)(compared with guaiac-based FOBT) led to similar positive predictive values for the two test types (Gastroenterology 2008;135:82)……these results support the Joint Colorectal Cancer Screening Guideline recommendations to abandon older guaiac-based cards in favor of immunochemical FOBT.
• Immunochemical FOBT’s better sensitivity but lower specificity for detecting cancer and advanced adenomas (compared with guaiac-based FOBT) led to similar positive predictive values for the two test types (Gastroenterology 2008;135:82)(2.3% less specific than was guaiac-based FOBT for detecting cancer and 1.3% less specific for detecting advanced adenomas)…..wider use of immunochemical FOBT would result in more colonoscopies, it would also lead to the detection of substantially more neoplasias, and the positive predictive value would be comparable to that seen with guaiac-based FOBT.
• Aspirin and NSAIDs do not appear to affect Immunochemical Fecal Occult Blood testing according to data on 212 patients taking them who subsequently undewnt colonoscopy (Am J Gastroenterol 2009;104:933)…..sensitivity and specificity of immunochemical FOBTs for colonoscopy-detected advanced neoplasias were 51% and 91%, respectively among the 912 non-users and 67% and 90% among the users……the authors conclude that these drugs need not be discontinued before immunochemical FOBT screening.
• For 2 iFOBTs, use of low-dose ASA compared to no ASA was not afftected (actually associated with markedly higher sensitivity 70.8% & 58.3 Vs 35.9 & 32%) for detecting advance colorectal neoplasms with only a slightly lower sensitivity (85.7% vs 89.2)(JAMA 2010;304:2513-20)…..Based on the colonoscopy findings, iFOBT sensitivity results for advanced neoplasms were as follows: Hemoglobin vs Hemoglobin-Haptoglobin: Aspirin users 70.8% vs 58.3%. Aspirin nonusers 35.9% vs 32.0%. ….Specificities were slightly lower for aspirin users than nonusers (e.g., 85.7% vs. 91.1% for the hemoglobin-haptoglobin test).
• A widely studied fecal immunochemical test again outperformed guaiac-based testing in screening patients for colorectal cancer (Hemoccult II guaiac-based vs OC-Sensa Micro FIT)(Am J Gastroenterol 2010;105:2017)….7.9% of patients tested positive with guaiac-based FOBT; 12.2% of patients tested positive with FIT when the hemoglobin cut point was 75 ng/mL, and 11.2% tested positive when the cut point was 100 ng/mL.
• FIT was much more sensitive than guaiac-based FOBT, particularly for detecting cancer, although specificity was slightly lower with FIT, at least at the 100-ng/mL cut point. An increase of 1°C in outdoor temperature was associated with a 0.7% reduction in the probability of a positive result immunochemical FOBT (Gut 2010;e-pub ahead of print).
• FIT is more accurate than guaiac-based fecal occult blood testing (gFOBT) in screening for colorectal cancer accoring to a Dutch study with 1256 average-risk patients submitted single specimens for FIT (OC-Sensor) just before undergoing screening colonoscopy (Am J Gastroenterol 2012;107:1570)…..Colonoscopy identified 8 patients (0.6%) with colorectal cancer and 113 (9%) with advanced adenomas. At a cutoff of 50 ng/mL, FIT was positive in 10% of patients. Sensitivity and specificity of FIT for detecting advanced adenomas were 38% and 93%, respectively. For colorectal carcinoma, sensitivity was 88% (i.e., FIT was positive in 7 of 8 patients with cancer), and specificity was 91%. This study suggests that FIT is equally effective in both the proximal and distal colon, whereas some previous evidence had suggested better performance in the distal colon.
• FIT can identify a significant percentage of patients with proximal or distal advanced neoplasia with a single test (Am J Gastroenterol 2012;online in the July 31st)…..At the 50 ng/mL cutoff, FIT had 38% sensitivity for advanced neoplasia at a specificity of 93%.
Colonoscopy vs. FIT: A RCT with 27,792 patients shows show higher adherence to FIT (q2yrs), similar detection and yield of cancer, but higher adenoma detection rates and complications with colonoscopy (N Engl J Med 2012;366:697)…..Advanced adenoma detection rates were 1.9% in the colonoscopy group and 0.9% in the FIT group……Patients who want a more effective test and who value cancer prevention as well as cancer detection will choose colonoscopy…..Patients who are concerned about the invasive nature of colonoscopy will choose another first-line test such as FIT……it is important that we offer them alternatives.
Immunochemical vs Guaiac Paper: Specificity to Human hemoglobin only vs Human and animal hemoglobin. No dietary restrictions. Sensitivity 50 ng/mL vs 1500 ug hHb/g.
iFOBT products: Hemoccult ICT, Hemosure One-Step, immoCARE, Instant-View FOBT, InSure, and MonoHaem.
Hemoccult ICT: supplied as a three card pt test kit. Each card has two specimen collection zones. Pt’s are instructed to place two different swabs of the collected stool on each collection zone. Three kits are provided so that the pt will collect a stool sample on three consecutive days. The test analytical sensitivity is ~ 300 mcg hemoglobin per gram of feces (mcg/Hb/g) compared with Hemoccult and Hemoccult II at ~ 750 mcg/Hb/g. $2.50. Each kit comes with a mailing envelope so that the specimens can be mailed or brought back to the health care professional’s office. The fecal immunochemical test is more effective for at-home colon cancer screening than is a sensitive FOBT (Cancer. 2006;107:2152-2159).
Hemosure One-Step: kit contains a collection pad for capturing the stool specimen, a collection tube with a poke spiral applicator for insertion into six sites of the stool specimen, and a mailing envelope. Analytical test sensitivity is ~ 50 mcg/Hb/g of stool. Only one stool specimen is used. Price for the kit $10.
The immoCARE: product provides a stool specimen collection stick and bottle of buffer solution. The pt places the stool-containing swab into the bottle of buffer solution. Once received by a health care professional, the specimen-bottle is shaken, the tip of the bottle is broken and two drops are applied to a test cassette. The results can be read in five minutes. A single stool sample is used. The approximate analytical test sensitivity is 30 mcg/Hb/g of feces. Cost $16. ImmoCARE is available under the name, ColonCARE, at some pharmacies for pt purchase.
Instant-View FOBT I: available with a specimen collection tube, used as a sample applicator, and a cassette. Using the applicator, the sample is placed on the cassette. It provides a visual result in five to ten minutes upon addition of a stool swab sample. Analytical test sensitivity is ~ 50 mcg/Hb/g of feces. Only one stool specimen is used. Price is $10 per test.
InSure: kit consists of a test card with a specimen sampling brush and a mailing envelope. With InSure, the stool sample is collected by brushing the surface of the stool in the toilet bowl. The sample is then applied with the brush to the test card. The process is repeated with a second sample. The pt mails the completed test to Quest Diagnostics lab for processing. The analytical test sensitivity is about 50 mcg/Hb/g of feces.
ForSure: FDA clearance in 5/07 for the detection of possible colorectal carcinoma, Crohn’s disease, ulcerative colitis, and colon polyps in humans. The clearance allows for both over-the-counter and professional applications of the test. The test is used to identify indicators of human hemoglobin in human stool. The test features a dual-purpose collection tube to serve as a sample applicator and a device to preserve the transportation of pt specimen collection. In addition, the test is stable without the use of dietary restrictions.
MonoHaem: uses a three card two specimen application per card process. The pt kit contains cards, applicators, and a storage bag for return to the healthcare professional office. Approximate test sensitivity is 1,000 mcg/Hb/g to 2,000 mcg/Hb/g of feces. Price is $2.10 per kit.
The FlexSure OBT test, is more sensitive than Hemoccult Sensa, a guaiac test, at detecting left-sided colorectal cancer (J Natl Cancer Inst 2007;99:1424-1425,1462-1470) (81.8% sensitive and 96.9% specific vs 64.3% and 90.1%).
Info: An evaluation of 6 fecal immunochemical testing (FIT)(BioNexia FOBplus, PreventID CC, immoCARE-C, FOB advanced, QuickVue iFOB and BioNexia Hb/Hp Complex) found that they displayed markedly different performances; only two had specificity for advanced adenomas >90% (Ann Intern Med 2009;150:162)(immoCARE-C had sensitivity of 25.4% for advanced adenomas and specificity of 96.7%, and FOB advanced had sensitivity of 26.9% for advanced adenomas and specificity of 92.9%).
• A quantitative immunochemical fecal occult blood test (FOBT) is superior to the standard guaiac-based FOBT for detecting advanced colorectal neoplasms and cancer (Am J Gastroenterol 2010;online May 25th)…For the guaiac-based test, the PPV were 13.1% for advanced adenomas, 19.7% for advanced colorectal neoplasia, and 6.7% for colorectal cancer. The PPV’s with qFIT (using the 100 ng/mL cut point and 3-sample qFIT results) were 23.3%, 36.0%, and 12.8%, respectively…..Negative predictive values for advanced adenomas, advanced colorectal neoplasia, and colorectal cancer were high, with overlapping confidence intervals for the two tests.
• An increase of 1°C in outdoor temperature was associated with a 0.7% reduction in the probability of a positive result on immunochemical FOBT (Gut 2010;Jul 5;e-pub ahead of print)….presumably because hemoglobin degrades more in warm than in cool temperatures. Seasonable adjustments might need to be made in such testing programs to account for this effect.
CPT codes have been approved by CMS for Medicare billing are G0328QW for testing as a cancer screen, the reimbursement is $23.
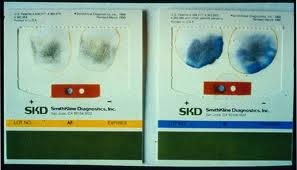 3. Guaiac-based: nonspecific and insensitive. Hem occult II and Hem occult II SENSA are the most commonly used, they are widely available and inexpensive. The limitations of include low sensitivity and a high false-positive rate. The test should be done annually, but many pt’s balk at handling stool. The pseudoperoxidase activity of Hb turns the guaiac compound blue in the presence of hydrogen peroxide. Eat foods high in fiber for one week before testing to cause more rapid stool transit, but avoid certain fruits and vegetables for 72 hours before testing. The USPSTF now recommends that FOBT be performed using immunochemical testing or the improved guaiac-based test, Hemoccult Sensa (Ann Intern Med 2008;Oct 6:e-pub ahead of print).
3. Guaiac-based: nonspecific and insensitive. Hem occult II and Hem occult II SENSA are the most commonly used, they are widely available and inexpensive. The limitations of include low sensitivity and a high false-positive rate. The test should be done annually, but many pt’s balk at handling stool. The pseudoperoxidase activity of Hb turns the guaiac compound blue in the presence of hydrogen peroxide. Eat foods high in fiber for one week before testing to cause more rapid stool transit, but avoid certain fruits and vegetables for 72 hours before testing. The USPSTF now recommends that FOBT be performed using immunochemical testing or the improved guaiac-based test, Hemoccult Sensa (Ann Intern Med 2008;Oct 6:e-pub ahead of print).
if + –> Need complete colonic evaluation (colo or flex sig + DCBE) within 2-3 mo’s. colo as 5-10% risk of CA. Two slides should be prepared from each of 3 consecutive bowel movements. They should be developed w/in 7days of collection. Avoid rehydration. + if any one of six slide windows is positive.
Developer is H2O2 & ETOH –> peroxidase reaction that turns the indicator blue. No False + with PO Fe. Guaiac based (Hem occult), will detect losses of ~20ml/day. Normal person loses 0.7-2ml/d blood in GI, early Ca loss is 1-2cc/d proportional to the tumor size. 50% of colon Ca sheds enough blood for + test. Warfarin use did not increase false-positive screening FOBT results according to data from 372 pt’s that were on warfarin and 9265 that were not (Am J Gastroenterol 2010;105:2030).
Avoid: False- : Stop Vit-C doses >250mg/d 2 days before testing (causes a false negative). Certain substances in the stool may give false positive. Storage >5 days (bacteria degrades Hb), non bleeding lesion, antacids, bile, dried specimen. Cancers and precancerous lesions bleed intermittently.
False +: (1-3% even with strict protocols) Any food containing pseudoperoxidase or associated with peroxidase activity (including rare red meat and uncooked fruits and vegetables, such as broccoli, turnips, cauliflower, radishes, and cantaloupe) can produce a false-positive result. –> Avoid large doses of NSAIDs, undercooked Red meat/ poultry/ fish, cantaloupe, broccoli, radish, cauliflower, collard greens, parsley, horseradish/ cocktail sauce, cucumber, zucchini, lemon rind (vegetable peroxidase). Not stopping iron therapy for 3 days, iodine, red fruits, bromide, chlorophyll. Long distance runners have up to 23% + guaiac.
• It is probably not necessary to restrict aspirin/NSAID use before FOBT to screen for colon cancer (Am J Med 2004;117:837-41) as ASA doses up to 1250 mg/day don’t seem to produce positive FOB tests. And even if an occult blood test comes back positive due to aspirin or NSAID usage, it’s good to know as GI bleeding from any source is important to detect. Tell pt’s to continue their normal activities and follow their normal diet during testing.
• Warfarin therapy does not lower the positive predictive value of FOBT (Am J Gastroenterol 2005;100:1586-1592)….a positive result in this setting should therefore not be ignored.
• A guaiac-based fecal occult blood test (FOBTs) program in England tested nearly 2.1 million people aged 60 to 69 found nearly 1800 colorectal cancers — most (77%) of them left-sided (Gut 2011;Dec 7;e-pub ahead of print)…
Individuals with positive tests (i.e., with 5 or 6 out of 6 windows testing positive) were offered colonoscopy, those with one to four positive windows were invited to repeat the tests; if any windows in as many as two additional tests were positive, individuals were referred for colonoscopy. Test-return rates were 40% in the London area and higher (55%–60%) in other regions of the country. The rate of positive tests was 2.5% in men and 1.5% in women; the uptake of colonoscopy or other investigational testing among these individuals was 83%. Cancer was identified in 11.6% of men and 7.8% of women who underwent such investigation, and high-risk adenomas were found in an additional 12.2% of men and 6.2% of women. Most of the cancers identified were early stage (10% polyps, 32% Dukes A, and 30% Dukes B).
On Coumadin: W/u: same as if INR is therapeutic then 67% chance of pathology.
!n Sure FOBT: detects the globulin portion of the Hb molecule. The globulin does not survive the passage through the upper GI tract, thus less false positives (does not react to non-human Hb, vitamins, drugs or peroxidases in foods). A long-handled brush is used to brush the surface of the stool while in the toilet bowl, thus trapping dislodged occult blood and water on the bristles. The brush is then dabbed onto the test card where the water dries into a special pad. Once dry, the Hb is considered stable and the card is sent to a lab for testing. The is a test line and a control line, if Hb is present, it binds to a colloidal gold-conjugated polyclonal Ab and turns red. A negative is one red line, a positive is two red lines.
OTHER: HemoQuant appears to be significantly better than Hem occult II which is better than HemeSelect in detecting occult upper GIB (Mayo Clin Proc 2002;77:23-28) A study has found that the first-generation stool DNA test (SDT-1) is not more effective than the widely used FOB tests Hemoccult and HemoccultSensa (Beckman Coulter) for detecting screen-relevant colorectal neoplasms (Ann Intern Med. 2008;149:441-450)……However, a second-generation stool DNA stool test (SDT-2), which uses a broader marker panel, was substantially more sensitive than FOB testing, and the higher sensitivity was particularly evident for adenomas. The sensitivities of SDT-1 and HemoccultSensa were very similar for screen-relevant neoplasms (20% vs 21%, respectively), whereas the sensitivity of SDT-2 was 40%…….although stool DNA analysis might be more effective in detecting colorectal neoplasia than fecal occult blood testing, the tests are still not comparable in efficacy to colonoscopy, as previously reported by Medscape Oncology.
Stool (Fecal) DNA Test: This method is 4 times more sensitive than FOBT; however, it is only half as sensitive as colonoscopy in average-risk pt’s. It’s high cost (US$400-$800) and fairly low positive predictive value indicate that it is not yet ready for widespread use as a screening test. Screens for DNA mutations. DNA is stable and shed continuously in the stool, PCR can detect it in minute amounts with a high sensitivity for both malignant and premalignant adenomatous polyps. 30g of stool is needed, the pt packs it on ice and ships it to the lab, where they homogenized it to separate bacterial and human DNA. Positive test needs colonoscopy.
• A digital protein truncation assay for abnormal polypeptides associated with adenomatous polyposis coli (APC) gene mutations, 50-60% sens/ 100% spec (NEJM 2002;346:311-20). May also detect other aerodigestive cancers (lung, esophageal, stomach, pancreas). Costs may be reduces as since only 6% of pop gets colorectal Ca and only 50% develop adenomatous polyps, this may decrease the need for colonoscopy. The kits are large and cost $400-700 each.
• Fecal DNA analysis detects a greater proportion of important colorectal neoplasia than fecal occult-blood testing (Hemoccult II) (51.6% Vs 12.9% of invasive cancers AND 18.2% Vs 10.85 of advanced neoplasia = tubular adenoma >1 cm or a polyp with high-grade dysplasia), but neither test detected the majority of lesions identified on colonoscopy (NEJM 2004;351:2704-2714).
• Stool DNA testing was not (yet) cost-effective, but as cost decrease of $300 or an adherence improvement of 50% is needed (Ann Intern Med 2010;153:368)…..The analysis assumed a cost for the stool DNA test of US$350, based on the costs of commercially available tests……to be cost-effective, stool DNA testing would need to cost $34 to $51 if performed at 5-year intervals and $40 to $60 if performed at 3-year intervals, based on two different simulation models……..editorialist notes that current reimbursement for fecal immunochemical testing (FIT) by Medicare is <$25 and that some FIT assays have sensitivity approaching that of current stool DNA tests but with better specificity……..serum hypermethylation assays, which have become available at costs similar to that of stool DNA testing, would seem to have greater potential to achieve substantial adherence gains.
**Ref: (NEJM 1993;328:1365) (Ann IM 1993;118:1294)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








