DIAPHRAGMATIC INJURY
CASE SCENARIO
A 22-year-old man was brought to the emergency department (ED) after a motor vehicle accident. The patient was entrapped and restrained in the passenger seat of a car that had been impacted on the passenger’s side by a truck.
On arrival to the emergency room his airway was patent, and he was immobilized with a rigid cervical collar and backboard. His respiratory rate was 20 breaths per minute with decreased breath sounds at the right base, and his oxygen saturation was 97% on 15 L oxygen through reservoir mask. His heart rate was 96 beats per minute and his blood pressure 139/91 mm Hg. He had a Glasgow Coma Scale (GCS) score of 15, and there was no loss of consciousness.
The remainder of his physical examination was significant for cervical spine tenderness, right-sided ecchymosis of the torso with ipsilateral pain, mild shortness of breath, and tenderness over the right 8th, 9th, and 10th ribs. He complained of diffuse abdominal discomfort and had mild tenderness to palpation of the right upper abdominal quadrant. He had a right arm deformity, but neurovascular examination was symmetrical to the contralateral limb. The remainder of the examination was unremarkable. His chest x-ray demonstrated right-side rib fractures, and a small right hemothorax with opacity in the right lower lung field. His focused assessment with sonography for trauma (FAST) scan was positive for perihepatic and perisplenic fluid. A right chest tube was placed that returned 300 cc of blood.
Following this, the patient underwent contrast-enhanced computed tomography (CT) scan evaluation remarkable for fractures of the right 8th, 9th, and 10th ribs; grade III liver laceration with hemoperitoneum; and rupture of the right hemidiaphragm. X-rays of the right upper arm revealed a midshaft humerus fracture.
A decision was made to take the patient to the operating room for exploratory laparotomy given the diaphragmatic injury. A 7-cm rupture of the right hemidiaphragm and the liver laceration were confirmed and repaired. Open reduction and internal fixation of the upper arm fracture took place under the same anesthesia.
Postoperative course was unremarkable and he was discharged in good condition.
EPIDEMIOLOGY
The incidence of diaphragmatic injury (DI) after trauma ranges from 0.8% to 8% after blunt trauma and 10% to 15% after penetrating trauma.1–5 Penetrating trauma is the leading cause (63%–73%) of all traumatic DI, with an incidence of 30% to 42% among patients with thoracoabdominal wounds.5,6 For blunt trauma, approximately 90% of diaphragmatic ruptures occur after motor vehicle accidents, with falls and crush injury constituting the remainder.7,8 Nearly two-thirds of DI following blunt trauma occurs in the left hemidiaphragm, although right diaphragmatic rupture may be underdiagnosed.9,10 Bilateral hemidiaphragm injuries are reported in 2% to 6% of patients.11,12 The decreased incidence of right-sided injuries could possibly be due to the liver dissipating force across the diaphragm.
PATHOPHYSIOLOGY
The diaphragm is the musculotendinous sheet that separates the positive-pressure abdominal cavity from the negative-pressure thoracic cavity. It plays a predominant role in ventilation, and injury to the diaphragm often impairs gas exchange and oxygen delivery. The muscular portion of the diaphragm attaches peripherally to the thoracic wall and lumbar vertebrae, and inserts centrally onto the central tendon. During exhalation, the diaphragm can rise to the level of the nipples, and it descends as low as the eighth thoracic dermatome with inhalation. This is important to recognize, as signs of injury to the thorax in this region should raise suspicion for DI.
The mechanics of respiration affect the presentation and natural history of diaphragmatic hernia. The pleuroperitoneal pressure can result in progressive herniation of abdominal contents through the diaphragmatic defect and into the chest with each respiration cycle.13 If the patient is intubated and receives positive-pressure ventilation, this gradient is reversed, which may delay visceral herniation and lead to false-negative findings on radiological imaging.9
As mentioned earlier, approximately one-third of patients suffer diaphragmatic injury from blunt trauma, in particular from motor vehicle accidents. DI is a marker for high-energy transfer. Injury is significantly more likely with compartment intrusion (≥15 cm) and high-velocity changes (≥35 km/h).14
Several mechanisms may cause DI in blunt trauma. The transmission of blunt force to the abdomen can increase pleuroperitoneal pressure gradients in excess of diaphragmatic strength, thus causing rupture.15 Other proposed mechanisms include lateral impact collisions, which deform the thoracic wall and shear the diaphragm, and rib fracture fragments penetrating the diaphragm.16,17 In a large series of 731 patients with traumatic diaphragmatic rupture, the most common site of injury was in the left posterolateral region.10 This area is a site of a congenital weakness, where the pleuroperitoneal membrane ultimately closes at embryogenesis.2
The severity of trauma and the intimate relationship of the diaphragm to adjacent thoracic and abdominal organs accounts for associated injuries in 52% to 100% of patients with DI.7,11 In fact, the mortality for diaphragmatic rupture is associated with the severity of associated injuries, and not with the acute DI itself. Williams et al. reported a higher mortality with blunt injury compared to penetrating injury due to significant thoracoabdominal injuries.10 Also, traumatic brain injury is present in 50% of DI cases and is predictive of mortality.3–5 Pneumohemothoraces and rib fractures are seen in 90% of patients, and aortic injury in 5%.1,17 Intra-abdominal injuries include lacerations to the spleen in 60% of cases, and the liver in 93% with right-sided DI and 24% with left.7,11 Pelvic fractures (40%–55%) and long-bone fractures (45%–85%) also occur with high frequency.1,17
Blunt diaphragmatic ruptures usually exhibit large radial tears (>10 cm), which predispose to herniation of abdominal viscera.2,17 Initially, the hernia is often asymptomatic or presents as vague upper abdominal discomfort. Difficulties with ventilation may be seen in the intubated patient. Delayed presentation, due to chronic defects that have a tendency to become larger, may exhibit signs of bowel obstruction and even life-threatening bowel strangulation.18
Practitioners should always suspect DI when evaluating patients with thoracoabdominal penetrating injuries. Furthermore, DI remains in the differential for any patient sustaining a truncal gunshot wound, as the missile can take an unpredictable course.19 Penetrating injuries produce small diaphragmatic holes, usually about 1 cm in diameter, with a left-side predominance that corresponds to the prevalence of right-handed assailants.5,20
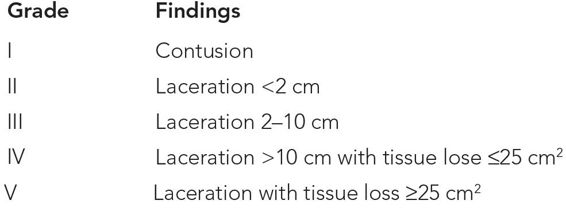
The American Association for the Surgery of Trauma (AAST) characterizes DI under a generally accepted injury scoring scale, as outlined in Table 28–1.
CLINICAL PRESENTATION
Diaphragmatic injury may be classified into three phases of presentation: (a) the initial or acute phase, which takes place during the original trauma presentation; (b) the latent phase; and (c) the obstructive phase.21 In the acute phase, coexisting trauma may divert attention to more obvious injuries and consequently prohibit DI detection.1,10 Diagnostic ambiguity is worsened by the nonspecific signs and symptoms of DI. Shoulder pain, epigastric pain, vomiting, dyspnea, absent breath sounds, or bowel sounds heard during chest auscultation can suggest DI; however, a high index of suspicion is required, especially as delayed treatment confers increased morbidity and mortality.18,22 Regarding penetrating DI, the characteristically small size of DIs presents a diagnostic challenge. The ability to detect these injuries noninvasively is highly important for the appropriate application of selective nonsurgical management.6
The latent phase of DI varies considerably in duration and severity of symptoms. During this phase, patients with missed DI might have no symptoms or might have nonspecific respiratory symptoms, such as shortness of breath and exercise intolerance. Also, upper gastrointestinal (GI) discomfort, reflux, early satiety, and changes to bowel movements can possibly be present.
The obstructive phase corresponds to acute symptoms of gastrointestinal obstruction due to visceral herniation. These symptoms may be intermittent or progressive, and range from nausea and vomiting, to acute onset of dyspnea, chest pain, and abdominal pain, and finally cardiovascular collapse and septic shock.5,19
DIFFERENTIAL DIAGNOSIS
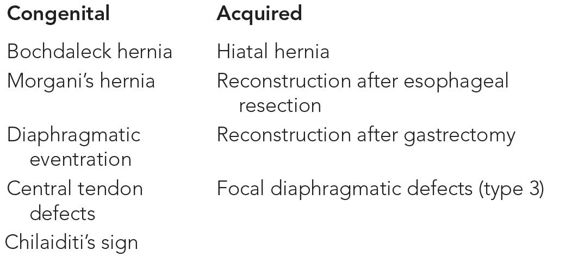
See Table 28–2.
WORKUP AND CHOICE OF IMAGING
DI remains a diagnostic challenge, since pathognomonic clinical and radiological signs may be subtle or absent. Chest x-ray is always the first imaging modality for trauma patients, and occasionally can reveal a large diaphragmatic rupture. According to Gelman et al., chest radiographs were diagnostic in 46% of patients with surgically proven left blunt DI, but only in 17% of right-sided injuries.15 The authors suggested that the liver blocks herniation of abdominal viscera into the right hemithorax, thus making radiographic diagnosis of right DI more difficult. A review of the literature reveals that 12% to 66% of diaphragmatic ruptures are missed on initial chest radiography, with the potential risk of late presentation following visceral herniation.2,18
CT is commonly performed in the initial evaluation of hemodynamically stable patients with blunt thoracoabdominal trauma to establish injury burden, and in these cases DI might be diagnosed incidentally. Early reports with conventional CT suggested a variable sensitivity of 14% to 61% and specificity of 76% to 99% for the diagnosis of diaphragmatic rupture.23,24 More recent studies, however, report sensitivity between 71% and 100%.25 The sensitivity and specificity of current CT technology (64+ detector) in diagnosing blunt diaphragmatic rupture has yet to be established.
Regarding penetrating trauma, diaphragmatic defects are typically between 1 and 2 cm in diameter, and as such are difficult to detect.26 Initial studies with CT suggested comparable specificity with blunt diaphragmatic trauma, with a much lower sensitivity, ranging from 0% to 40%. Again, the advent of 4-, 16-, and 64-section multidetector CT scans has improved detection rates, with the more recent reported overall sensitivity ranging from 73% to 100%.6,27,28
The focused assessment with sonography for trauma (FAST) examination during initial trauma evaluation has placed ultrasound at the forefront of trauma diagnosis. Ultrasound use in the diagnosis of DI is limited; however, a few case reports describe detection following blunt trauma.29,30 A negative study cannot exclude the diagnosis, and it is prudent to pursue further imaging—usually CT—if there is clinical suspicion of DI.
Magnetic resonance imaging (MRI) is time-consuming and poorly adapted to polytraumatized patients, and thus should be reserved for hemodynamically stable patients who cannot undergo CT scanning, or for whom a high index of suspicion persists despite equivocal or negative studies.
In equivocal cases or hemodynamically unstable patients, surgical exploration may be indicated to establish the diagnosis.
IMAGING FINDINGS
 Chest Radiography
Chest Radiography
Normal Diaphragm
Chest radiograph normally shows the upper surface of the dome-shaped diaphragm at its interface with the lung. The inferior surface of the diaphragm cannot be distinguished from the soft tissues of the abdomen. In normal adults, the cupola of the right hemidiaphragm spans from the fifth rib to the sixth rib, and rarely to as low as to the seventh rib. Also, the right diaphragmatic dome is usually half an interspace higher than the left; however, both may appear at the same level, or the left may be higher than the right31 (Figure 28–1).
Figure 28–1 Normal upright chest x-ray demonstrating the expected position and contours of the diaphragm.
Diaphragmatic Injury
Distinct radiographic findings of visceral herniation include visualization of abdominal organs in the thorax with or without focal constriction of the herniated mass at the site of the tear (collar sign).15 Identification of the classic radiological finding of the nasogastric tube above the left hemidiaphragm is also indicative of herniation in the setting of trauma.
Other findings that could suggest DI include hemidiaphragmatic elevation, contralateral mediastinal shift, pleural effusion, and distortion of the diaphragmatic contour. However, these signs are nonspecific and may reflect concurrent pulmonary pathology such as hemothorax, atelectasis, phrenic nerve palsy, or pulmonary contusion16 (Table 28–3 and Figures 28–2 and 28–3).