Key Clinical Questions
Introduction
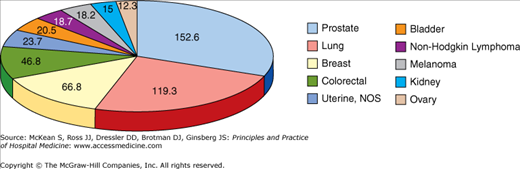
Cancer of unknown primary site (CUP) is described as histologically confirmed metastases with no identifiable primary site of origin. The majority of malignancies present with an obvious primary site, whereas CUP has a reported incidence of 2.3% to 7.8% in international databases. Prostate, lung, breast, and colorectal have remained the top four primary sites of cancer for most of this decade (Figure 184-1).
Of the over 1.5 million new cancer cases estimated to be diagnosed in the United States in 2010, 30,000 cases were reported without an identifiable source, similar to the number of new cases of pancreatic cancer diagnosed each year. After appropriate evaluation, less than 25% of these patients will have a primary site identified.
The median age of CUP patients is 60 years, with males being more affected than females. The prognosis is dismal, with median survivals ranging from 11 weeks to 11 months, a 1-year survival rate of less than 25%, and a 5-year overall survival rate of approximately 11%. However, with the advancement of diagnostic tools and techniques, the ability to identify a primary site has improved over time, allowing for treatment plans specific to the primary site.
Pathophysiology
While CUP may be a distinct biologic and clinical entity, a few theories attempt to explain the biology behind CUP. There are many debatable hypotheses as follows:
- The primary tumor remains microscopic and escapes detection.
- The primary tumor spontaneously regresses after seeding the metastatic site—the “burned out primary.” For example, testicular scarring is sometimes seen in metastatic germ cell tumors.
- The embryonic epithelial cells that fail to appropriately migrate may undergo malignant transformation and result in a cancer of unknown primary. Extragonadal germ cell tumors in the mediastinum and undescended testes illustrate this biologic theory.
- Aberrations in genetic and molecular profiles may also explain the origin of CUP.
Histology
Despite the lack of a known primary site, CUP can still be classified in histologic categories, allowing for better differentiation and treatment (Table 184-1).
These categories include adenocarcinoma, squamous cell carcinoma, neuroendocrine carcinoma, poorly differentiated carcinoma, and poorly differentiated neoplasm. The latter is a vague label, as the tissue does not have any defining characteristics and may include carcinoma, lymphoma, melanoma, or sarcoma. Within these histologic categories, subsets exist with favorable prognosis (Table 184-2).
|
Diagnostic Evaluation
The clinical presentation itself will often provide the necessary information to diagnose an occult primary. Hence, the evaluation begins with a thorough history and physical. It is important to identify any possible risk factors for malignancy and any signs or symptoms suggestive of a primary site. The history should include a detailed occupational, tobacco, gynecologic, and family history.
The physical exam must also be a comprehensive and systematic head-to-toe examination. This would include a breast and pelvic exam in females, testicular and prostate exam in males, and digital rectal exam in all patients.
|
Laboratory studies should begin with routine blood tests to assess hematologic and end-organ function, including a complete blood count, renal and liver function tests, and lactate dehydrogenase. When appropriate, urinalysis, urine cytology, and fecal occult blood testing should also be included.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree