Diagnostic Imaging of the Abdomen
Swapnil S. Bagade
Rebecca Hulett Bowling
KEY POINTS
 The plain abdominal radiograph is the most common imaging technique in the PICU but exposes the child to ionizing radiation.
The plain abdominal radiograph is the most common imaging technique in the PICU but exposes the child to ionizing radiation.
a. confirm proper position of catheters and tubes,
b. diagnose pneumoperitoneum with gas seen between the liver and the abdominal wall in the left lateral decubitus position, and
c. diagnose bowel obstruction with dilated proximal bowel loops and absent gas in the distal bowel.
 Ultrasound is an excellent imaging tool in children because of the absence of ionizing radiation. However, overlying bowel gas may limit visualization.
Ultrasound is an excellent imaging tool in children because of the absence of ionizing radiation. However, overlying bowel gas may limit visualization.
a. intussusception (“target sign”; sensitivity and specificity ˜100%),
b. guiding paracentesis in patients with ascites,
c. detection of hepatic vascular complications after liver transplantation by using Doppler ultrasound, and
d. focused abdominal sonography for trauma (FAST) to locate free fluid or hemoperitoneum in the upper quadrants and the pelvis.
 Computed tomography (CT) requires ionizing radiation and has been associated with increased cancer risk in children.
Computed tomography (CT) requires ionizing radiation and has been associated with increased cancer risk in children. CT is the imaging modality of choice for evaluation of abdominal injury after blunt trauma in a hemodynamically stable patient.
CT is the imaging modality of choice for evaluation of abdominal injury after blunt trauma in a hemodynamically stable patient. Plain radiographs are often the initial radiologic investigation used to evaluate a child with abdominal symptoms in the PICU. Other supplemental imaging techniques used include fluoroscopic gastrointestinal procedures with contrast media, ultrasound (US), and advanced cross-sectional imaging with computed tomography (CT) or magnetic resonance imaging (MRI). This chapter discusses these techniques of imaging the abdomen in children, highlighting the role of plain films, with brief discussions of fluoroscopy, US, and advanced imaging of CT and MRI.
Plain radiographs are often the initial radiologic investigation used to evaluate a child with abdominal symptoms in the PICU. Other supplemental imaging techniques used include fluoroscopic gastrointestinal procedures with contrast media, ultrasound (US), and advanced cross-sectional imaging with computed tomography (CT) or magnetic resonance imaging (MRI). This chapter discusses these techniques of imaging the abdomen in children, highlighting the role of plain films, with brief discussions of fluoroscopy, US, and advanced imaging of CT and MRI.PLAIN RADIOGRAPHS
The plain abdominal radiograph is an indispensable tool for both suspected abdominal pathology and the placement of tubes and catheters in children. Since children are more sensitive to radiation and have a longer life expectancy than adults, it is important to minimize radiation exposure. Dose reduction in diagnostic radiology must be achieved without compromising the diagnostic quality of the image. Low-dose techniques using increased tube potential (kVp) between 60 and 70 and a low milliampere-second (mAs) of 2-4 significantly decrease the dose (1).
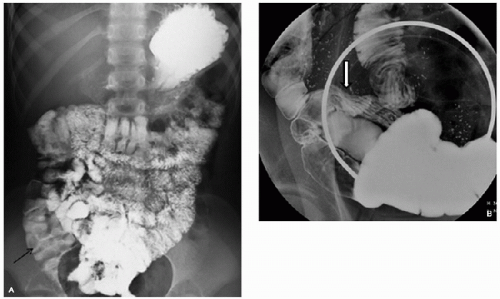
Various radiographic views for assessment of the abdomen include supine, decubitus, and cross-table (horizontal) lateral. The left lateral decubitus view is preferred over the right lateral decubitus view for detection of a pneumoperitoneum because it is more sensitive (gas is easily seen between liver and abdominal wall). The bowel gas pattern is part of the radiographic assessment. Gas is usually present in the stomach within 10-15 minutes of birth and fills the large bowel by 12-14 hours (2). The bowel loops should be symmetric and often have a polygonal pattern (“chicken wire”) on the supine image (Fig. 102.1). A decubitus film or, less commonly, a cross-table lateral view also shows the bowel gas pattern in another plane (Figs. 102.2 and 102.3). Both views are evaluated for abdominal masses and calcifications. Free intraperitoneal fluid may be seen on a plain film if the amount is sufficient; it will cause the bowel loops to move centrally, with increased opacity in the flanks (Fig. 102.4). The abdominal radiograph may also reveal a lower lobe pneumonia or pleural effusion as the cause of abdominal symptoms. In addition, abnormalities of the soft tissues and bones can be visualized.
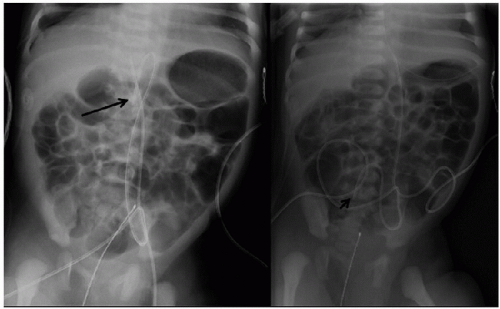
Tubes and catheters: An abdominal radiograph is often ordered to assess the position of tubes and catheters after placement. It is important to determine the position of the tubes and catheters to prevent untoward complications associated with their misplacement, kinking, or break in continuity. Common tubes and catheters seen on an abdominal radiograph include umbilical arterial catheter (UAC), umbilical venous catheter (UVC), peripheral and central venous catheters, enteric tube, gastrostomy tube, ventriculoperitoneal shunt tubing, drainage tubes, pH probes, and temperature probes (Figs. 102.5A-C, 102.6A,B, and 102.7).
Bowel obstruction (images can be seen in later sections according to etiology): The typical clinical presentation in a neonate includes poor feeding, vomiting, abdominal distension, and delayed passage of meconium. An increase in postgastric aspirates may also be present. Differentiation between large and small bowel on plain film in the neonate or very young
child can be difficult since mucosal landmarks such as valvuli, plicae, and haustra are poorly developed. The radiologic findings in obstruction differ dep ending on the level of pathology. High intestinal obstruction implies obstruction from the stomach to the level of proximal ileum. There may be air
only in the stomach in cases of gastric outlet obstruction such as in pyloric stenosis, antral dyskinesia, or antral web. Two dilated bowel loops (double bubble) are seen with duodenal atresia (DA), annular pancreas, or duodenal web. More dilated bowel loops are present with a jejunal obstruction as in jejunal atresia (3,4). A low bowel obstruction shows multiple loops of dilated bowel in the abdomen. Low intestinal obstruction is seen in conditions involving the ileum, such as meconium ileus and ileal atresia, and pathology of the colon including Hirschsprung disease (HD), meconium plug/small left colon,
colonic atresia, and imperforate anus. Contrast enemas are helpful in determining whether the colon or distal small bowel is the cause of low intestinal obstruction. In many cases of a high obstruction, the patient is taken to surgery after the plain film is obtained. If there is a concern for malrotation, an upper GI (UGI) study should be performed. In cases of low intestinal obstruction, plain film followed by enema is recommended (5).
child can be difficult since mucosal landmarks such as valvuli, plicae, and haustra are poorly developed. The radiologic findings in obstruction differ dep ending on the level of pathology. High intestinal obstruction implies obstruction from the stomach to the level of proximal ileum. There may be air
only in the stomach in cases of gastric outlet obstruction such as in pyloric stenosis, antral dyskinesia, or antral web. Two dilated bowel loops (double bubble) are seen with duodenal atresia (DA), annular pancreas, or duodenal web. More dilated bowel loops are present with a jejunal obstruction as in jejunal atresia (3,4). A low bowel obstruction shows multiple loops of dilated bowel in the abdomen. Low intestinal obstruction is seen in conditions involving the ileum, such as meconium ileus and ileal atresia, and pathology of the colon including Hirschsprung disease (HD), meconium plug/small left colon,
colonic atresia, and imperforate anus. Contrast enemas are helpful in determining whether the colon or distal small bowel is the cause of low intestinal obstruction. In many cases of a high obstruction, the patient is taken to surgery after the plain film is obtained. If there is a concern for malrotation, an upper GI (UGI) study should be performed. In cases of low intestinal obstruction, plain film followed by enema is recommended (5).
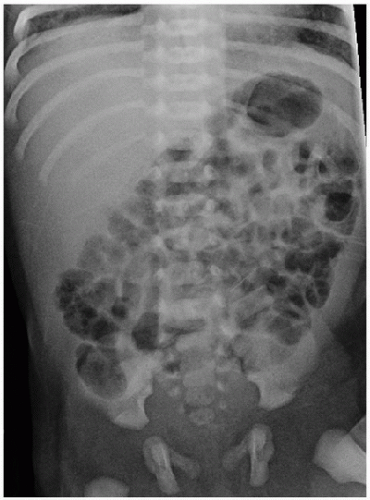 FIGURE 102.1. Normal abdominal bowel gas pattern. Supine AP radiograph of a neonate shows air-filled small-bowel loops in the center and air-filled colon in the periphery of the abdomen. However, in a neonate the differentiation between small and large bowel loops can be difficult. Air-filled stomach is seen in the left upper quadrant. Soft-tissue opacity of the liver occupies the right upper quadrant. |
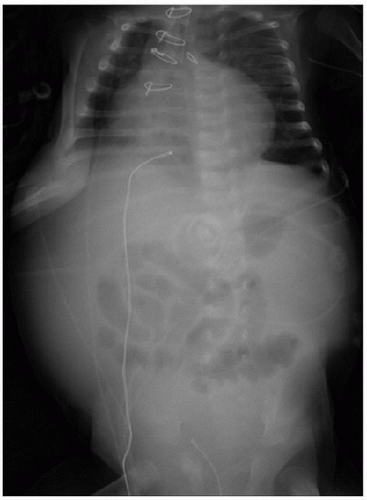 FIGURE 102.4. Ascites. On the abdominal radiograph, there is increased soft-tissue density in the periphery of the abdomen (from the ascitic fluid) with centrally located (floating) bowel loops. |
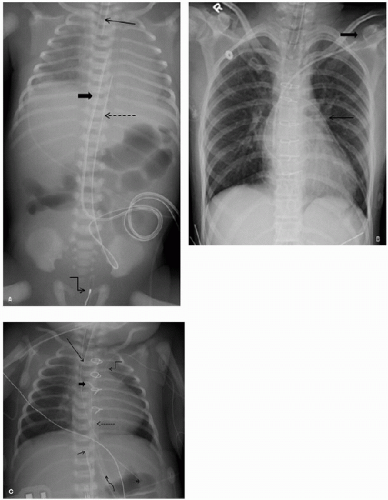 FIGURE 102.5. Positions of tubes and catheters. A: UVC terminating in the right atrium (bold arrow), while the UAC terminating at the level of T6 (dotted arrow). The UVC ideally should be at the level of the diaphragm. The UAC typically turns inferiorly from the umbilicus in the iliac artery and then extends superiorly in the aorta and is expected to terminate at the level varying from T6 to T10. Also seen are the endotracheal tube (thin arrow), which should lie at least 1 cm above the carina. A temperature probe is seen in the pelvis (angled arrow). B: A left-sided subclavian venous catheter (blocked arrow) is seen with its tip in the right atrium along with a mediastinal drainage catheter (thin arrow). C: Frontal view of the chest shows left PICC (peripherally inserted central catheter) line terminating in the left innominate vein region (angled arrow), UAC with its tip at the T7-8 level (dotted arrow), UVC ending over the left liver lobe (short arrow), likely in the ductus venosus. A well-positioned endotracheal tube about 3 cm above the carina (long arrow), and a drainage catheter extending in the mediastinum (curved arrow), Ductus ligation clip (blocked arrow), and the tip of nasogastric tube in the stomach (asterisk). |
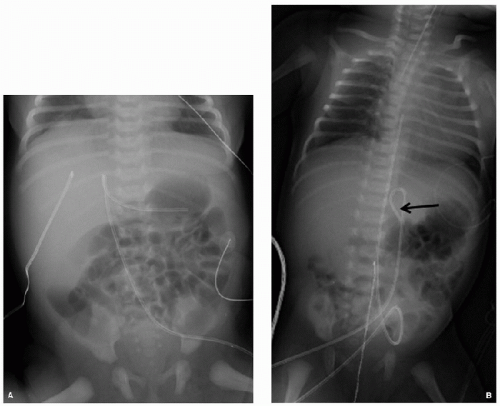 FIGURE 102.6. Malposition of catheter. A: The UVC bends to the left to overlie the mid-abdomen and probably extends into the splenic vein. B: In another case, the UVC loops near the hepatic hilum, and terminates overlying the left upper quadrant. Ideally, the tip of the UVC is positioned near the inferior cavoatrial junction. |
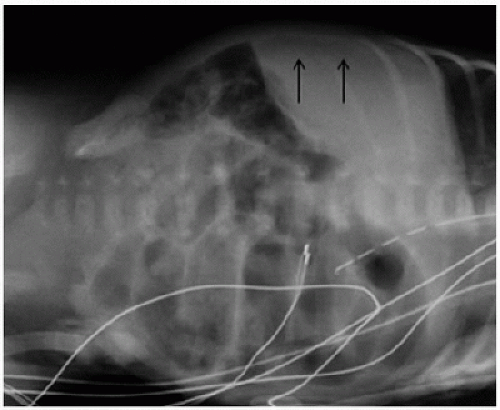
Pneumoperitoneum: Causes of pneumoperitoneum in the child include necrotizing enterocolitis (NEC), spontaneous perforation not associated with NEC, ruptured Meckel diverticulum, dissection from pneumomediastinum, gastric perforation (e.g., from a nasogastric tube, mechanical ventilation, indomethacin administration, or child abuse), colonic perforation (possibly secondary to an enema or a rectal thermometer), peritoneal dialysis, paracentesis, recent surgery, and abdominal trauma (6). In older children, perforation in appendicitis, Meckel diverticulitis or ischemic or infective enteritis, and penetrating and blunt abdominal trauma are common causes of pneumoperitoneum (7). Locations of gas in the abdomen include intraluminal, extraluminal, intramural, and intraparenchymal. Free intraperitoneal air (extraluminal) is seen in nondependent areas (subdiaphragmatic along the liver dome, or along the lateral margin of the liver in a left lateral decubitus view) (Fig. 102.8A,B). Portal venous gas can be seen as branching linear lucencies along the periphery of the liver (Fig. 102.9). Gas in the biliary tract is more central overlying the liver with a branching tree pattern (8).
Pneumatosis intestinalis: Pneumatosis intestinalis (PI) is when air accumulates within the bowel wall. It is a well-known radiographic finding in cases of NEC, where it portends bowel infarction. Pneumoperitoneum and portal venous gas may be accompanied with PI. PI can also appear in intestinal ischemia, bowel obstruction, graft-versus-host disease, short bowel syndrome, infection with rotavirus, decompensated cardiac disease, and nonischemic colitis (9,10). A more benign occurrence of pneumatosis can be seen in chronic steroid use, immunodeficiency, nutritional deficiencies, bronchopulmonary dysplasia (BPD), or pneumomediastinum. On radiographs, pneumatosis may appear as small linear or bubbly lucencies within the bowel wall (Fig. 102.10).
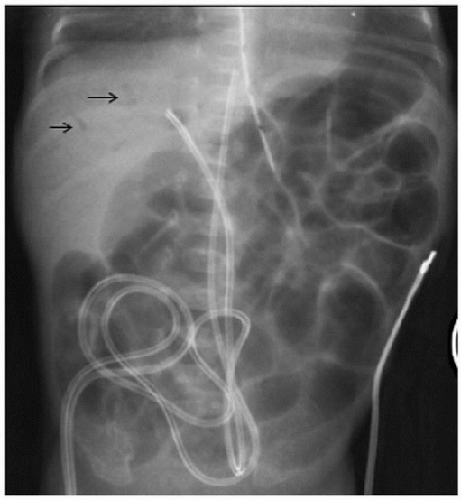 FIGURE 102.9. Portal venous gas. Abdominal radiograph showing branching linear lucencies (arrows) along the periphery of the liver owing to portal venous gas. |
Abdominal masses: The appearance of a soft-tissue opacity or mass is a common finding in a child with abdominal pathology. Plain abdominal radiographs are the initial imaging tests performed in the evaluation of a suspected abdominal mass. The radiographs may help determine the location of the mass, whether there is associated bowel obstruction, and whether calcifications are present. Calcifications are seen in several types of tumors including neuroblastoma and teratoma. Calcifications could also represent stones in the biliary or renal tracts. Sonography is a very useful adjunct study in the workup of abdominal masses.
CONTRAST STUDIES
The UGI series is often modified so that it both answers the clinical question and limits the radiation dose (4,5). An UGI study includes the esophagus, stomach, and duodenum to the duodenojejunal junction and is adequate to assess malrotation. Barium is the most commonly used contrast agent and is excellent for delineating GI tract anatomy. A small-bowel follow-through (SBFT) is used to assess the small bowel beyond the duodenum to the cecum, using serial imaging over several hours (Fig. 102.11A,B). Low osmolar, nonionic contrast agents (such as iohexol) are important and have clinical uses, but are much more expensive. These nonionic agents are used when there is concern for possible leak, as in the case of a repaired TE fistula. Hyperosmolar contrast (i.e., gastrografin) can be therapeutic in cases of meconium ileus, meconium plug, and chronic constipation. Water-soluble agents should be used if there is a potential for perforation.
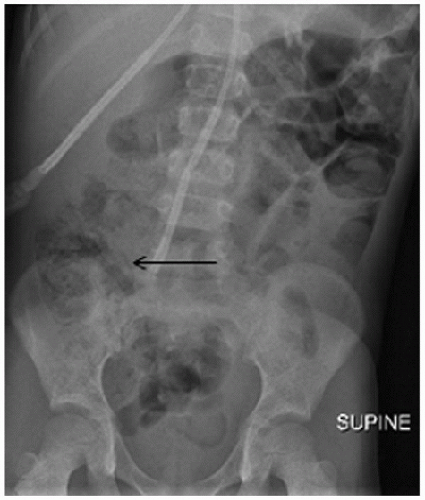 FIGURE 102.10. Pneumatosis intestinalis. Intramural air in the right-sided bowel is seen as streaky lucencies in the right abdomen (arrow). This patient was a 7-year-old with inflammation of the ileocecal area who developed PI. |
ULTRASOUND
 Ultrasonography is a key imaging tool with important applications in diagnosing abdominal pathology in children in the PICU. It is usually the first investigation in a child with a palpable abdominal mass after a plain film. In addition to identifying the solid or cystic nature of the mass, determination of the organ of origin may be assessed. US can be used to evaluate the relationship of the superior mesenteric artery (SMA) with the superior mesenteric vein (SMV) in cases of malrotation (11,12). High-resolution US can be used to evaluate
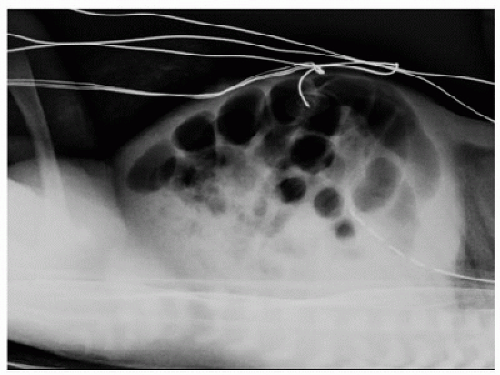
Ultrasonography is a key imaging tool with important applications in diagnosing abdominal pathology in children in the PICU. It is usually the first investigation in a child with a palpable abdominal mass after a plain film. In addition to identifying the solid or cystic nature of the mass, determination of the organ of origin may be assessed. US can be used to evaluate the relationship of the superior mesenteric artery (SMA) with the superior mesenteric vein (SMV) in cases of malrotation (11,12). High-resolution US can be used to evaluate  the bowel wall and to detect pneumatosis and portal venous gas. US is the modality of choice to confirm the presence of absence of intussusception. US is also an excellent tool to assess for ascites and can be used to guide paracentesis (Fig. 102.12). The lack of ionizing radiation, easy portability, and availability make it an ideal modality for use in children. The disadvantages of US include a potentially limited window in the presence of various catheters, tubes and dressings, interference by overlying bowel gas, as well as operator dependence.
the bowel wall and to detect pneumatosis and portal venous gas. US is the modality of choice to confirm the presence of absence of intussusception. US is also an excellent tool to assess for ascites and can be used to guide paracentesis (Fig. 102.12). The lack of ionizing radiation, easy portability, and availability make it an ideal modality for use in children. The disadvantages of US include a potentially limited window in the presence of various catheters, tubes and dressings, interference by overlying bowel gas, as well as operator dependence.Color and Spectral Doppler
Doppler US is useful in the evaluation of major vessels prior to cardiac shunt surgeries or extracorporeal membrane oxygenation in intensive care patients, and detection of post-liver transplant vascular complications and venous thrombosis. In the case of a post-liver transplant patient, the normal low resistance waveform of the hepatic arterial flow is replaced by a high-resistance waveform with resistive index elevated
above 0.8. Hepatic arterial thrombosis is highly suspicious if there is no diastolic and/or systolic hepatic arterial flow. Other vascular complications such as hepatic arterial stenosis, pseudoaneurysm, or venous thrombosis are also detected by Doppler (13). US is the first approach in suspected post-liver transplant complications including hepatic necrosis, perihepatic fluid collections, and biliary obstructions. Doppler also reliably determines the portal vein flow direction and velocity.
above 0.8. Hepatic arterial thrombosis is highly suspicious if there is no diastolic and/or systolic hepatic arterial flow. Other vascular complications such as hepatic arterial stenosis, pseudoaneurysm, or venous thrombosis are also detected by Doppler (13). US is the first approach in suspected post-liver transplant complications including hepatic necrosis, perihepatic fluid collections, and biliary obstructions. Doppler also reliably determines the portal vein flow direction and velocity.
 FIGURE 102.12. Ascites. Free abdominal fluid detected on US as anechoic collection under the abdominal wall. Hyperechoic floating bowel loops are seen. Same patient as in Figure 102.4. |
COMPUTED TOMOGRAPHY
 Concern for an increased risk of cancer in children exposed to radiation during CT makes it a less favored imaging modality. CT is performed only when radiographs or US do not diagnose the condition. CT is more useful than US in cases of trauma and to delineate the extent of visceral and intraperitoneal abscesses. The benefits of CT are excellent spatial and contrast resolution; newer scanners are fast enough that the patient may not need sedation. Younger patients receiving IV contrast for the CT often require sedation despite the use of fast scanning techniques because they tend to move when the contrast is administered. When ordering CT imaging, one should consider alternative imaging modalities not involving ionizing radiation such as US or MRI. Research is currently being done to provide CT scanner algorithms that decrease radiation dose while maintaining images of diagnostic quality (14,15). High scanning speed can decrease motion artifacts and at the same time decrease the radiation dose to the patient.
Concern for an increased risk of cancer in children exposed to radiation during CT makes it a less favored imaging modality. CT is performed only when radiographs or US do not diagnose the condition. CT is more useful than US in cases of trauma and to delineate the extent of visceral and intraperitoneal abscesses. The benefits of CT are excellent spatial and contrast resolution; newer scanners are fast enough that the patient may not need sedation. Younger patients receiving IV contrast for the CT often require sedation despite the use of fast scanning techniques because they tend to move when the contrast is administered. When ordering CT imaging, one should consider alternative imaging modalities not involving ionizing radiation such as US or MRI. Research is currently being done to provide CT scanner algorithms that decrease radiation dose while maintaining images of diagnostic quality (14,15). High scanning speed can decrease motion artifacts and at the same time decrease the radiation dose to the patient.MAGNETIC RESONANCE IMAGING
Improved detail due to better soft-tissue contrast and lack of ionizing radiation make MRI an important problem-solving
tool. The limitations for MRI are its cost, availability, and motion artifacts due to long scanning time. Various fast imaging techniques can reduce motion artifact. Techniques such as MR cholangiopancreatography to evaluate biliary and pancreatic abnormalities, MR enterography for gastrointestinal pathologies, and MR urography for evaluation of renal collecting system abnormalities and renal function are available. Diffusion-weighted sequences are used widely for imaging of neoplasms (16).
tool. The limitations for MRI are its cost, availability, and motion artifacts due to long scanning time. Various fast imaging techniques can reduce motion artifact. Techniques such as MR cholangiopancreatography to evaluate biliary and pancreatic abnormalities, MR enterography for gastrointestinal pathologies, and MR urography for evaluation of renal collecting system abnormalities and renal function are available. Diffusion-weighted sequences are used widely for imaging of neoplasms (16).
Differential Diagnosis and Imaging of Abdominal Pathology
1. Congenital and developmental disorders: Congenital anomalies of the gastrointestinal tract are a common cause of morbidity in children. These include obstructive defects in the intestine, anomalies of rotation and fixation, duplications, and anorectal anomalies.
a. Esophageal atresia with tracheoesophageal fistula: Esophageal atresia (EA) is the most common congenital abnormality of the esophagus. It results from failure of division of the primitive foregut (at the fifth gestational week) into two distinct tubes forming the esophagus and the trachea. In almost 90% of cases, EA is associated with a fistula to the posterior wall of the trachea. Proximal EA with distal tracheoesophageal fistula (TEF) is the most common type, seen in 85% of cases. This condition is usually part of the spectrum of VACTERL association: Vertebral, (imperforate) Anus, Cardiac, TracheoEsophageal fistula, Renal, and Limb (radial ray). A skeletal survey, cardiac echo, and abdominal US are required investigations in such cases to rule out these associated anomalies. Prenatal US is unlikely to diagnose EA with accuracy; nonspecific findings seen in a few cases are polyhydramnios and nonvisualization of the stomach. A dilated esophageal pouch in the neck with absent abdominal bowel gas may be seen in EA without a distal fistula (Fig. 102.13A). The most suggestive finding on the radiograph in a newborn is coiling of the nasogastric tube in the proximal esophagus (Fig. 102.13B) (4,5).
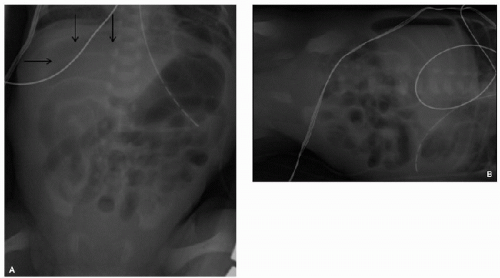
b. Diaphragmatic (Bochdalek) hernia: Incomplete closure of the pleuroperitoneal canal results in a posterior lateral diaphragm defect. Newborns with a large hernia beginning early in utero have a poorly developed ipsilateral lung (6). The contralateral lung may also be hypoplastic. Lung volume estimation is performed with serial antenatal USs, and preferably with MRI for prognostic purposes. On the chest radiograph, bowel loops are seen within the thoracic cavity with contralateral mediastinal shift (Fig. 102.14). The position of the tip of the nasogastric tube localizes the stomach. The bowel loops ideally are kept deflated in order to decrease intrathoracic pressure until surgical repair is performed.
c. Hypertrophic pyloric stenosis: Hypertrophic pyloric stenosis (HPS) affects 2-3 in 1000 infants and is most common in first-born males. The infant is typically 6 weeks old and presents with vomiting, dehydration, and hypokalemic alkalosis. The caterpillar sign (markedly dilated stomach with exaggerated incisura) may be seen on plain film and represents a distended, peristalsing stomach. US is the imaging gold standard and the method of choice for both diagnosis and exclusion of HPS with a sensitivity and specificity of close to 100% (Fig. 102.15A,B) (17,18). Scanning in the right posterior oblique position is helpful. Prior to vast improvements in US imaging, the UGI was used to evaluate children with projectile vomiting and would show signs such as the mushroom sign, antral shouldering, the string sign, and the double-track sign (redundant mucosa in the narrowed pyloric lumen causing separation of the barium into two channels) (Fig. 102.15C). The treatment for HPS is surgical myotomy.
d. Congenital gastric/duodenal obstruction: This includes antral atresia, duodenal atresia, duodenal stenosis (DS), duodenal web (or diaphragm), annular pancreas, and preduodenal portal vein. Duodenal atresia is the most common cause of high intestinal obstruction in a child. Its associations include Down syndrome and congenital heart disease. The diagnostic plain radiograph finding is a double bubble, with air present in the distended stomach and duodenal bulb (Fig. 102.16A) (16
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree