Chapter 50 Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State
3 What is the pathogenesis of DKA?
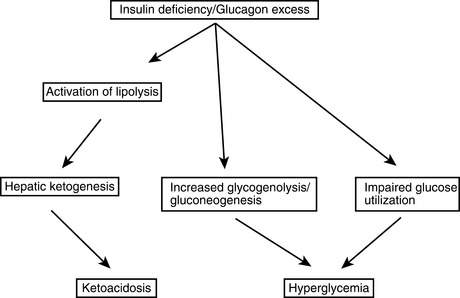
DKA starts withabsolute insulin deficiencybecause of a broken or clogged insulin pump, missed injections, or progression of an unknown illness to overt insulin deficiency or withrelative insulin deficiencyfrom a rise in tissue insulin requirements from infection, trauma, or other stresses. Glucose production from the liver increases, and glucose clearance into peripheral tissues is impaired, causing the blood glucose level to rise. Stress-related increases in counterregulatory hormones exacerbate these effects. As the renal glucose threshold is passed, an osmotic diuresis occurs causing urinary losses of water and electrolytes. The ensuing dehydration further increases the level of catecholamines. Also, because glucagon and insulin levels are normally inversely related, the insulin deficiency causes hyperglucagonemia. The increased catecholamines and glucagon and the insulin deficiency promote excess release of fatty acids from the adipose tissue that further impairs insulin-mediated glucose uptake into peripheral tissues. The capacity of the liver for β-oxidation of the fatty acids is exceeded, resulting in ketone production. This ketonemia and the resulting acidosis often cause nausea and vomiting; the patient’s polydipsia therefore stops, worsening the dehydration. The patient is now in DKA with this whole process occurring over a 12- to 48-hour period. This sequence of events is depicted inFigure 50-1.
9 How does the hyperosmolar hyperglycemic state (HHS) differ from DKA?
 Occurs most often in the elderly and those with known type 2 diabetes
Occurs most often in the elderly and those with known type 2 diabetes
 Very high blood glucose levels of 600 mg/dL or greater
Very high blood glucose levels of 600 mg/dL or greater
 Markedly elevated serum osmolarity of 320 mOsm/kg or greater
Markedly elevated serum osmolarity of 320 mOsm/kg or greater
 Frequent occurrence of altered mental state or coma
Frequent occurrence of altered mental state or coma
 More serious hypotension and overt dehydration including substantially larger electrolyte losses than DKA
More serious hypotension and overt dehydration including substantially larger electrolyte losses than DKA
 High mortality rate that averages 15% versus less than 2% in uncomplicated DKA
High mortality rate that averages 15% versus less than 2% in uncomplicated DKA
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree