Chapter 40 Dermatological presentations to emergency
Dermatology presentations to emergency department are common, accounting for 15–20% of visits,1 with the majority of presentations due to an infective aetiology or the result of drug reactions. Overall, there are four basic categories of dermatological presentation to emergency department (see Table 40.1).
Table 40.1 Isolated dermatological disorders
| Reason for presentation | Common or important clinical examples |
|---|---|
| New onset or flare | Eczema (atopic dermatitis)Papular urticaria—mainly a paediatric emergency presentation usually representing an exaggerated local hypersensitivity to an insect bite which can be clinically dramatic and/or severe, such as a blistering skin reaction |
| Subacute or chronic with complication | Impetiginised scabies, eczema |
| Dermatological presentations with systemic associations | |
| Fifth disease | Pregnant woman—increased risk of hydrops fetalis or aplastic crisis if underlying haematological disorder |
| Systemic disorders resulting in acute presentations with prominent cutaneous manifestations | |
| SLE/PAN/cholesterol emboli | Vasculitis, trash foot, broken livedoid eruption |
| Systemic disorders with associated cutaneous changes or disorders | |
| Inflammatory bowel disease and/or inflammatory arthritis | Pyoderma gangrenosum |
| Systemic disorders with unrelated/incidental cutaneous findings | |
| Common presentations | Seborrhoeic dermatitis (> 50% elderly but also more common in particular clinical settings, e.g. advanced HIV/AIDS, neurological disorders, especially Parkinson’s disease) |
HIV/AIDS, human immunodeficiency virus/acquired immune deficiency syndrome; PAN, polyarteritis nodosa; SLE, systemic lupus erythematosus
Table 40.2 Terminology for skin lesions
| Lesion | Description |
|---|---|
| Bulla(e) | Large fluid-filled lesion > 0.5 cm in diameter |
| Cyst | Closed cavity/sac with epithelial lining containing solids or fluids |
| Discoid | Disc-shaped (nummular) |
| Erythema | Redness of the skin from vascular congestion or increased flow such as in inflammation |
| Macule | Flat alteration in colour and/or texture of the skin, e.g. colour change due to skin inflammation including erythema and/or hyper/hypopigmentation (change in melanin, haemosiderin); if larger than several centimetres, referred to as a patch |
| Nodule | Solid mass > 0.5 cm in diameter, palpable |
| Papule | Solid elevation of the skin < 0.5 cm in diameter |
| Petechiae | Pinpoint, flat, round, purplish red spots caused by intradermal or submucosal haemorrhage |
| Plaque | Solid, elevated lesion; may be formed by coalescence of papules |
| Purpura | Bleeding into the dermis; may be macular or papular |
| Pustule | Circumscribed collection of pus, commonly staphylococcal, but may be sterile in inflammatory and autoimmune dermatoses, e.g. pustular psoriasis |
| Telangiectasia(e) | Tiny visible blood vessels in the upper dermis ± inflammation |
| Verrucous | Rough, warty |
| Vesicle | Visible accumulation of fluid within or beneath the epidermis, < 0.5 cm |
| Wheal | Transient area of dermal oedema, pale, compressible, papular or plaque-like |
Surface characteristics: scale, crust, horn, excoriation, maceration, lichenification
Table 40.3 Diagnosis of dermatological disease
| Diagnosis | |
| Accurate characterisation of skin eruption | E.g. exanthematic eruption, skin rash due to or mimicking a viral infection |
| Isolated skin presentation versus any worrisome systemic involvement; concerning symptoms or associated findings | E.g. high fever (> 40°C) or ‘sick’ patient presentation |
| Differential diagnosis | |
| Infection: viral, bacterial, fungalDrug eruption: isolated (simple) exanthematic hypersensitivity reaction (and/or the manifestation of a systemic hypersensitivity reaction)Connective tissue disease, graft versus host disease (due to an acute disease flare and/or active inadequately controlled disease) | |
| Drug and other exposures | |
| Medications history | When medications, including over-the-counter and alternative or natural therapies, were started and/or stopped; any previous reactions to similar or crossreacting medications, vaccinations or injections |
| Other exposure | IVDU, environmental exposure, history of infective symptoms, travel |
| Diagnostic testing | |
| Diagnosis | Most diagnoses are suspected in emergency but confirmed at a later date. e.g. drug reactions largely a diagnosis of exclusion |
| Differential diagnosis | May require baseline (acute) viral and autoimmune serologyALWAYS perform a bacterial culture for M/C/S if itchy/weeping/crusted/purulent, ± viral culture if painful |
| Associated diseases/toxicities/complications | E.g. hepatitis, nephritis as part of a drug hypersensitivity syndrome and/or connective tissue disease flare. Drug hypersensitivity reactions are more common in those living with HIV/AIDS, lymphoma ± CTD |
| Determine probabilities | |
| Paediatric | Infectious aetiology more likely |
| Adult | Consider comorbidities and always consider drug causes, especially in the elderly |
| Dermatologist consult | |
| Urgent | E.g. suspected SJS/TEN |
| Organise follow-up/discuss | |
CTD, connective tissue disease; IVDU, intravenous drug use; M/C/S, microculture and sensitivity; SJS, Stevens-Johnson syndrome; TEN, toxic epidermal necrolysis
Table 40.4 Infective complications of dermatoses in immunocompetent patients
| Bacterial | |
| Viral | Herpes simplex virus 1, 2 |
| Fungal | Trichophyton rubrum and T. tonsurans (especially in rural and remote Indigenous populations) |
Table 40.5 Assessing patients with dermatological emergency presentations
MORPHOLOGICAL CLASSIFICATION OF DERMATOLOGICAL PRESENTATIONS
1 Urticaria (hives) ± angio-oedema ± anaphylaxis
History
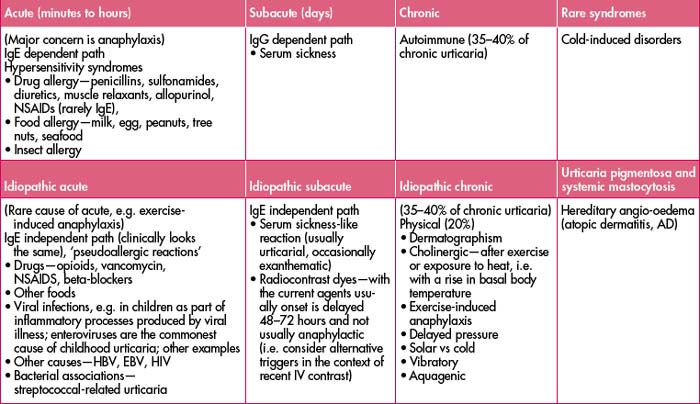
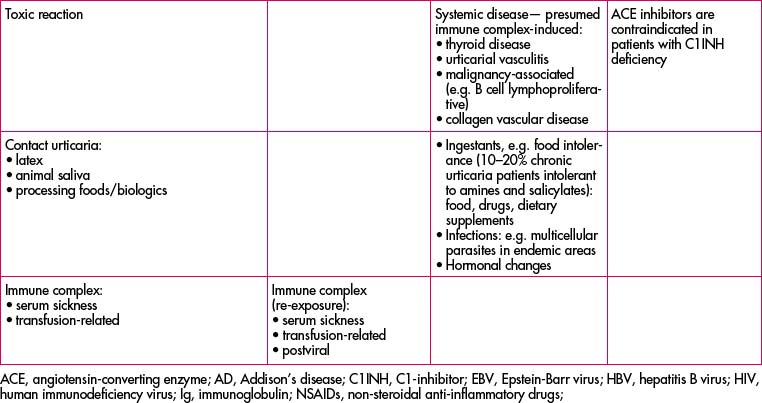
Onset of hives, swelling and itch in relation to stimulus. Acute presentations are typically seen in acute infections and hypersensitivity reactions to foods, medications or insect bites. See Table 40.6 below for classification of causes.
Clinical features
Differential diagnosis: erythema multiforme (EM)
Management: symptomatic ± acyclovir ± nutritional supplementation if there is significant mucosal involvement.
Management
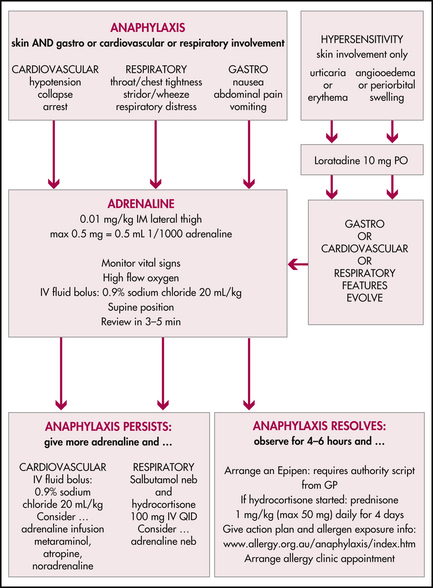
Refer to the flow chart, which includes anaphylaxis management, in Figure 40.1.
Table 40.7 Medications in angio-oedema, anaphylaxis and acute and ‘subacute’ urticaria
| Medication | Recommended adult dose | Comment |
|---|---|---|
| Adrenaline | 0.5–1.0 mL of 1:1000 IM | Used if evidence ofanaphylaxis |
| 4 mg q4–6 h, max 24 mg/day | ||
| Acute severe episodes, avoid chronic use, especially in patients with chronic urticaria |
Table 40.8 Treatment of chronic urticaria (often a distressed patient with chronic symptoms presenting with a flare)
| Simple measures | Keep cool, loose clothing | |
|---|---|---|
| 4mg q4–6 h, max 24 mg/day | ||
| Useful in chronic urticaria in addition to H1 antihistamines | ||
| Cyproheptadine | 4 mg TDS | Sedating antihistamine plays an important role in chronic urticaria, e.g. with nocturnal exacerbations or insomnia due to urticaria, and appetite stimulant |
| Doxepin | 10–50 mg/day | H1- and H2-blocking properties, sedating, appetite stimulant, higher doses have anxiolytic and antidepressive effects |
| Acute severe episodes, avoid chronic use, especially in patients with chronic urticaria | ||
| Other immunosuppressives | For immunologist referral |
2 ‘Spotty, blanching’ exanthematic eruptions
Exanthematic eruption
Clinical features
Note: For exanthematic ‘spotty, blanching’ eruptions, ALWAYS consider the seriousness of the presentation: skin changes ± mucosal features ± systemic features, i.e. eruption plus systemically well versus eruption plus systemically unwell patient.
Investigations
Differential diagnosis
Table 40.9 Differential diagnosis, exanthematic eruption
| Paediatric exanthematic eruption | Adult exanthematic eruption |
|---|---|
• Inflammatory includes connective tissue disease; other, as part of a flare or warning of disease activity in the context of systemic illness | |
Kawasaki’s disease
Table 40.10 Features and management of common viral exanthems in paediatric patients
| Disease/virus | Signs/symptoms | Management |
|---|---|---|
| Enterovirus | Commonly respiratory or gastroenterology presentations ± exanthem or urticaria | Presentation dependent |
Mid-prodrome—pruritic vesicles that break and crust, starts centrally or facially and spreads to the extremities | ||
Prodrome fever, malaise, coryza, conjunctivitis, cough then erythematous maculopapular rash face, trunk, legs, buccal mucosal lesions, Koplick spots | Symptomatic management, contact considerations, vaccinations | |
| No prodrome during incubation 14–21days. | Symptomatic, consider contacts including pregnant contacts | |
| Infants 6–8 mo—high fever, relatively well; multiple pale pink macules/papules as fever breaks | Supportive | |
| Sore throat, cough, headache, nausea, fever with rash, slapped cheek appearance followed by lace-like erythema on the extremities and buttocks | Supportive but consider concurrent haematological disease or pregnant exposure | |
| Scarlet fever/toxins from Streptococcus pyogenes | ||
| Mumps | Morbilliform rash with lymphadenopathy, an issue in young males with potential infertility | Despite vaccination consider occurrence |
| Mycoplasma pneumoniae | Antimicrobial therapy for Mycoplasma, e.g. rifampicin | |