Dermatologic
14-1 Rashes
Mark Silverberg
It is imperative to describe correctly any rash found on physical examination of a patient. This facilitates communication among physicians and helps to ensure that the patient will receive appropriate diagnosis and treatment. The following are a number of standard definitions for common rash morphologies1:
Macule: A flat, circumscribed change in skin color less than 1 cm in diameter
Patch: A macule that is larger than 1 cm in diameter
Papule: A solid, elevated, superficial lesion smaller than 5 mm in diameter
Plaque: A solid elevated lesion (width greater than height) larger than 5 mm in diameter
Nodule: A solid elevated lesion with depth into the underlying tissue and a diameter between 5 mm and 2 cm
Tumor: A nodule with a diameter greater than 2 cm
Vesicle: An elevated, superficial, fluid-filled blister smaller than 5 mm in diameter
Bulla: An elevated, superficial, fluid-filled lesion larger than 5 mm in diameter
Pustule: A papule or vesicle that contains free pus
Wheal: A rapidly evolving, flat-topped papule or plaque caused by transient cutaneous edema, as seen in an allergic reaction
Abscess: A nodule or tumor containing free pus
REFERENCES
1. Sanfilippo AM, Barrio V, Kulp-Shorten C, Callen JP. Common pediatric and adolescent skin conditions. J Pediatr Adolesc Gynecol 2003;16:269-283.
14-2 Erythema Multiforme
Brenda L. Liu
Clinical Presentation
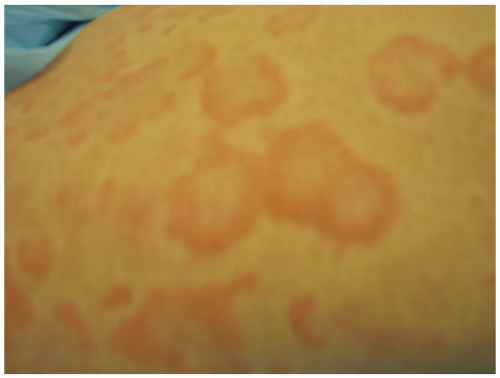
Patients with erythema multiforme (EM) may present with the classic “target” lesions, which are smaller than 3 cm, with concentric rings of color changes, a well-defined border, and a central grey blister or necrotic area.1 EM predominantly affects young adults, aged 20 to 40 years.1,2 Skin lesions are often pruritic and cause burning; oral lesions are painful and can interfere with eating.1,2
Pathophysiology
EM results from host immune reactions to antigens.2 Infectious diseases and pharmacologic agents may precipitate EM.1,2 Herpes simplex virus (HSV) is the most common cause of EM and has been implicated in 50% of cases.2 Mycoplasma infection is also a potential cause of EM.1 Histopathology of EM skin lesions reveals dermal edema with epidermal involvement that tends to be limited to the central area of the target lesion.2
Diagnosis
EM is an acute, self-limited process characterized by symmetric, well-demarcated plaques, located predominantly on the extensor surfaces of the extremities.1 EM is classified into EM minor and EM major, with the latter involving the oral mucosa.2 The diagnosis is a clinical one, based on physical examination.1,2 Laboratory studies usually are normal, although in severe EM major, an elevated erythrocyte sedimentation rate (ESR) and a moderate leukocytosis may occur.2
Clinical Complications
Management
Treatment consists of supportive care. Medications suspected of causing EM should be stopped if possible.1 Comfort measures include systemic or topical anesthetics for skin lesions and oral anesthetics (e.g., viscous lidocaine rinses) for oral lesions.2 Patients should be instructed to avoid spicy and acidic foods, and the importance of sufficient fluid intake should be stressed.2 Topical antibiotics may prevent secondary bacterial infection of the skin. In individuals with recurrent EM and known HSV infection history, acyclovir prophylaxis may be beneficial in preventing recurrences.1,2
REFERENCES
1. Ferrera PC, Dupree ML, Verdile VP. Dermatologic problems encountered in the emergency department. Am J Emerg Med 1996;14:588-601.
2. Ayangco L, Rogers RS 3rd. Oral manifestations of erythema multiforme. Dermatol Clin 2003;21:195-205.
14-3 Stevens-Johnson Syndrome
Jennifer Kiss
Clinical Presentation
Patients with Stevens-Johnson syndrome (SJS) present with tenderness and erythema of skin and mucosa, which develops into extensive cutaneous and mucosal exfoliation. This can become life-threatening with multisystem involvement.1
Pathophysiology
SJS and toxic epidermal necrolysis (TEN) are part of the same spectrum. Both diseases can be caused by the same drugs, and a disease starting as SJS can lead to fullblown TEN. The histopathologic hallmark of SJS-TEN is epidermal necrosis.2 The most frequently implicated drugs are sulfa drugs, allopurinol, hydantoins, and carbamazepine.1 The exact pathogenesis is unknown but is most likely an immune response, such as a cell-mediated cytotoxic reaction against epidermal cells.3 Onset of SJS in drug-associated cases is usually 7 to 21 days after a new medication is started. SJS has several nondrug associations, including recurrent herpes and Mycoplasma pneumoniae infection.1
Diagnosis
Diagnosis is mainly clinical but may be confirmed by biopsy. SJS is usually drug-induced. The triad of mucous membrane erosion, target lesions, and epidermal necrosis with skin detachment characterizes SJS. The ultimate extent of full-thickness epidermal detachment is less than 10% in SJS.1
Clinical Complications
Management
Suspected inciting agents must be discontinued immediately. Management should include admission to an intensive care unit or burn unit and prompt cessation of potentially associated medications. Intravenous fluids should be managed as for a patient with full-thickness burns, with débridement of devitalized epidermis, burntype skin care, close monitoring, and prompt treatment of all infections, including sepsis.1
REFERENCES
1. Sullivan JR, Shear NH. Drug eruptions and other adverse drug effects in aged skin. Clin Geriatr Med 2002;18:21-42.
2. Revuz J. New advances in severe adverse drug reactions. Dermatol Clin 2001;19:697-709.
3. Riedl MA, Casillas AM. Adverse drug reactions: types and treatment options. Am Fam Physician 2003;68:1781-1790.
14-4 Toxic Epidermal Necrolysis
Aman Parikh
Clinical Presentation
Patients with toxic epidermal necrolysis (TEN) may report a prodromal phase consisting of fever, upper respiratory tract symptoms, conjunctival burning, and skin tenderness along with fever, headache, muscle aches, joint aches, nausea, vomiting, and diarrhea. Patients present with generalized pain and a rash. Patients may have diffuse involvement with skin sloughing, persistent fevers, and rash. Conjunctival involvement may lead to eye pain and photophobia. The skin manifestations of TEN are acute and progress very rapidly.
Pathophysiology
TEN is believed to be an immunologic reaction that causes disruption of the dermal-epidermal junction. The most common offending agents are antibiotics (penicillin, fluoroquinolones, macrolides, chloramphenicol), cyclooxygenase-1 (COX-1) and COX-2 inhibitors,1 antiepileptic medications, and allopurinol. Many cases are idiopathic, but causes include lymphoma, leukemia, measles, and viral syndromes. TEN is more common in adults, whereas staphylococcal scalded skin syndrome (SSSS) is more common in children and immunocompromised adults.
Diagnosis
The most important factor leading to diagnosis is strong clinical suspicion. A skin biopsy should be obtained if the diagnosis is being considered. The biopsy shows necrosis of the entire epidermis with minimal inflammatory cells. The epidermis may be completely detached from the dermis, which is characteristic for the disease. The definitive histologic diagnosis requires finding that the TEN blister is “subepidermal with overlying epidermal necrosis.”3 The differential diagnosis should include Stevens-Johnson syndrome (SJS), erythema multiforme (EM), Kawasaki disease, and SSSS.
Clinical Complications
Because of the loss of the skin barrier, bacterial infection and sepsis are common complications. Other complications include electrolyte imbalances, dehydration, hypoxemia, and renal insufficiency. Severe gastrointestinal hemorrhage may result from gastrointestinal mucosal sloughing. Ocular complications may include corneal scar formation, permanent visual impairment, entropions, and pseudomembrane formation.
Management
Discontinuation of the offending medication and meticulous supportive care are essential. Patients with oral involvement are at risk for dehydration and malnutrition, and fluid management is critical. Antibiotics should be started empirically if there are signs of infection. Steroid treatment for TEN is a controversial therapy, and intravenous immunoglobulin G (IVIG) has been proposed as an adjunctive treatment.2 The mortality rate for drug-induced TEN is approximately 20%, and that of idiopathic TEN is approximately 50%.3
REFERENCES
1. Friedman B, Orlet HK, Still JM, Law E. Toxic epidermal necrolysis due to administration of celecoxib (Celebrex). South Med J 2002;95:1213-1214.
2. Stella M, Cassano P, Bollero D, Clemente A, Giorio G. Toxic epidermal necrolysis treated with intravenous high-dose immunoglobulins: our experience. Dermatology 2001;203:45-49.
3. Ringheanu M, Laude TA. Toxic epidermal necrolysis in children: an update. Clin Pediatr (Phila) 2000;39:687-694.
14-5 Erysipelas
Harneet Sethi
Clinical Presentation
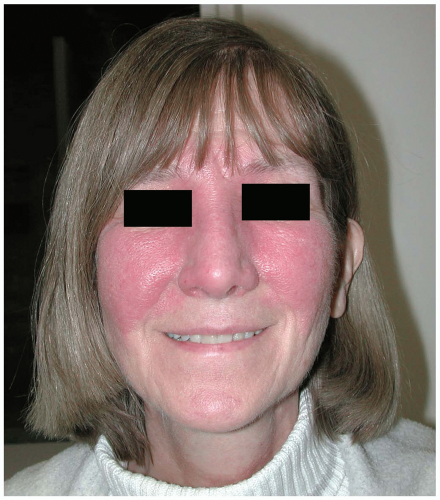
Patients with erysipelas present with well-demarcated skin lesions with spreading edges that advance at a rate of 2 to 10 cm per day. Erysipelas is most common on the lower extremities but may also involve the face, upper extremities, and trunk. This disease tends preferentially to afflict the very young and the elderly.
Pathophysiology
Erysipelas is a subset of cellulitis involving the superficial dermis. It is caused by Staphylococcus pyogenes or group A streptococci. Streptococcus agalactiae (B) and streptococci C and G have also been implicated.1
Diagnosis
Erysipelas is diagnosed clinically by the presence of an erythematous rash characterized by an elevated, advancing or spreading margin. Physical findings may include lymphadenopathy and lymphanagitis.1 The complete blood count (CBC) may reveal an increased white blood cell (WBC) count with leftward shift. An elevated C-reactive protein (CRP) concentration has been associated with erysipelas, but this is a nonspecific finding and may be impractical in the emergency department (ED) setting. It is important to perform a careful search for potential sites of introduction of infection, the most common of which is athlete’s foot. Venous stasis ulcers and leg wounds provide additional portals of entry. The area surrounding the lesions is notable for erythema and edema. In the majority of presentations (85%), fever is present.1
Clinical Complications
Complications include abscess formation, expanding cellulitis, septicemia, and recurrence. Gangrene, venous thromboemboli, and necrotizing cellulitis also may occur.1
Management
Most cases of erysipelas can be treated with penicillin, and oral administration is a first-line treatment, with the intramuscular route reserved for cases of noncompliance.2 Macrolides and cephalosporins are also effective. The extent of cutaneous involvement, the patient’s immune status, and the patient’s social situation should be weighed when considering inpatient treatment. Pain and fever control also should be addressed. Follow-up within 48 hours is recommended to ascertain the extent of any possible expansion of swelling and erythema. Failure to respond to antibiotic treatment within 48 hours should raise suspicion of a diagnosis other than erysipelas.1 Marking the extent of the lesion during the initial visit can provide a baseline from which to measure successful antibiotic treatment or lesion progression.
REFERENCES
1. Bonnetblanc JM, Bedane C. Erysipelas: recognition and management. Am J Clin Dermatol 2003;4:157-163.
2. Bishara J, Golan-Cohen A, Robenshtok E, Leibovici L, Pitlik S. Antibiotic use in patients with erysipelas: a retrospective study. Isr Med Assoc J 2001;3:722-724.
14-6 Shingles
Colleen Campbell
Clinical Presentation
Patients with shingles usually present with a neuropathic pain along the involved dermatome. Patients often describe the pain as tingling or burning, but it can also be itching, lancinating, or sharp. The pain varies from constant to intermittent and can precede the rash by 1 week.1 In “zoster sine herpete,” no rash forms after the prodromal phase.2 Five percent of patients also have prodromal symptoms of fever, malaise, and headache.3 The rash is localized to one dermatome and does not cross the midline. It usually involves one area of skin innervated by a single sensory dermatome.3 In 50%of patients, the rash is found in the thoracic region.1 The T5 and T6 dermatomes are most commonly affected,2 followed by the first trigeminal branch. The rash is characterized by clusters of vesicles with underlying erythema.1 The lesions evolve from macules and papules to vesicles and then pustules, finally forming a crust within 7 to 10 days.
Pathophysiology
Shingles (herpes zoster) is a localized, vesicular, cutaneous eruption caused by reactivation of varicella-zoster virus.
Older patients are more commonly affected than younger, immunocompetent individuals. There is no seasonal prevalence to the disease, and there is no difference in incidence by race or gender.1
Diagnosis
The diagnosis of herpes zoster is largely clinical. The characteristic unilateral vesicular rash is easily identified. There is commonly an accompanying regional lymphadenopathy as well. Hutchinson’s sign signals the involvement of the nasociliary branch of the ophthalmic nerve and is characterized by vesicles on the tip of the nose. Ramsey Hunt syndrome signifies involvement of the facial or auditory nerve and is evident with unilateral facial palsy and lesions on the ear or the anterior two thirds of the tongue.3 A Tzanck smear of early lesions that reveals multinucleated giant cells and intranuclear inclusion bodies confirms the diagnosis.3
Clinical Complications
The most common complication of shingles is postherpetic neuralgia, which occurs in 9% to 15% of patients overall,1 and up to 50% of those older than 65 years of age. Half of the patients with involvement of the ophthalmic branch of the trigeminal nerve (V1) have ophthalmic complications, including cranial nerve palsy (III, IV, VI), mucopurulent conjunctivitis, keratitis, uveitis, and episcleritis.2 Granulomatous cerebral angitis is a delayed complication of ophthalmic involvement and manifests as transient ischemic attacks (TIAs) or stroke.3 Up to 0.5% of patients develop meningoencephalitis or myelitis with shingles infection. Rarely, nausea, vomiting, and gastrointestinal distress occurs because of vagus nerve involvement. Motor paralysis can also occur if the infection spreads from the dorsal root ganglia to the anterior horn cells.3 Widespread dissemination can occur in immunocompromised individuals.
Management
The main therapeutic goal in the treatment of shingles is control of pain. Early treatment with antiviral drugs that inhibit varicella-zoster virus replication has been shown to reduce pain and shorten the time until the rash resolves. The use of oral corticosteroids may increase early healing of the rash, but it has not shown efficacy in reducing the time to resolution of symptoms.
REFERENCES
1. Wallace MS, Oxman MN. Acute herpes zoster and postherpetic neuralgia. Anesth Clin North Am 1997;15:371-398.
2. McCarary ML, Severson J, Tyring SK. Varicella zoster virus. J Am Acad Dermatol 1999;41:1-14.
3. Stankus SJ, Dlugopolski M, Packer D. Management of herpes zoster (shingles) and post-herpetic neuralgia. Am Fam Physician 2000;61:2437-2448.
14-7 Urticaria
Colleen Campbell
Clinical Presentation
Patients with urticaria present with dermal papules and plaques that usually are pruritic.1 The papules may be erythematous, whereas plaques often have white centers with surrounding erythema.1 These lesions may remain on the skin for longer than 24 hours.1 Hives may appear round, oval, or serpiginous. Hives may resolve in one area, only to appear in another area shortly thereafter.
Pathophysiology
Urticaria is a raised skin lesion that occurs in response to an immune trigger.1 This disorder is also known as “hives” or “wheals.”
Urticaria reportedly affects up to 20% of the population.1 It is considered to be acute if symptom duration is less than 6 weeks and chronic if symptoms have been present for longer than 6 weeks.1 Acute urticarial reactions are more common in children and young adults.1 Mast cell activation is the primary physiologic mechanism of hives, but urticaria also can be seen in type I, II, or III allergic responses.1,2 It is believed that the wheal is formed when fluid leaks from blood vessels in response to mast cell degranulation.1 Urticaria is most commonly idiopathic, but it occurs with a greater frequency in atopic individuals.2 Other causes are physical, immunologic, or toxic.1 Physical causes include temperature, pressure, and vibration. Urticaria can be mediated by immunoglobulin E (IgE), such as by aeroallergens. Immunoglobulin G (IgG) and immunoglobulin M (IgM) are mediators in infections. Autoimmune diseases and connective tissue disease induce urticaria through complement-mediated mechanisms.2 Toxic causes include exposure to nettles, strawberries, and insects.1 Nonsteroidal antiinflammatory drugs (NSAIDs) can cause histamine release and are also a common cause of urticaria.1,3
Diagnosis
Diagnosis of urticaria is based on a careful history and physical examination.2 A history of preexisting atopy and presence of classic wheals confirms the diagnosis. The history must be relied on to determine the inciting cause, although often it is difficult to identify a single significant precipitant.
Clinical Complications
The most dangerous manifestation of urticaria is rapid progression to anaphylaxis, which can lead to death.2 Superinfection of the skin can occur secondary to scratching of the pruritic areas.
Management
The most important issue in treatment is identification and removal of the cause of the urticaria, if possible.2 Antihistamines are the mainstay of therapy but are not always effective. It is recommended that antihistamine usage be continued for 96 hours after resolution of symptoms.2 A nonsedating antihistamine may be used during the day, in combination with diphenhydramine at night.2 Doxepin lotion may be used in addition to oral medications. Hydroxyzine and doxepin have both been shown to have greater H1 receptor blockade effects than diphenhydramine, and greater H2 receptor blockade effects than cimetidine.2 Oral corticosteroids can be added for a short course (5 days) for severe cases of acute urticaria.1,2 Alternate-day therapy with low-dose steroids may be useful for those patients whose symptoms recur on steroid withdrawal.1 Subcutaneous epinephrine injections may be required for sudden severe urticaria. Patients with chronic urticaria should be referred to their primary care physicians for further laboratory work-up and skin testing.1,3
REFERENCES
1. Kennedy MS. Evaluation of chronic eczema and urticaria and angioedema. Immunol Allerg Clin North Am 1999;19:19-32.
2. Beltrani VS, Thiers BH. Urticaria and angioedema. Dermatol Clin 1996;14:171-198.
3. Leung DYM, Boguniewicz M. Advances in allergic skin diseases. J Allerg Clin Immunol 2003;111:S805-S812.
14-8 Eczema
Yanick Isaac
Clinical Presentation
The eczematous reaction can manifest acutely as erythematous vesicular plaques or as a papulovesicular rash that is oozing, weepy, and intensely pruritic. As lesions progress and become subacute, the vesicles crust over and scale. Chronically, this rash is characterized by lichenification, hyperpigmentation, and scaling. Children older than 2 years of age and adults commonly present with the rash in the antecubital, popliteal, and flexural areas, whereas infants have lesions on the scalp, face, cheeks, and extensor surfaces of the extremities.1
Pathophysiology
Eczema is a generic term used to describe a spectrum of inflammatory skin diseases that manifest as a red, itchy rash. These include the subclasses of dermatitis, such as atopic, contact, dyshidrotic, seborrheic, stasis, and phototoxic dermatitis, in addition to lichen simplex chronicus and niacin and riboflavin deficiencies.1,2
Both immunologic and nonimmunologic mechanisms have been implicated in the development of eczema.1 The triggers of this type of response are numerous and include viruses, extremes of temperature, detergents, and cosmetics. These triggers stimulate the production of cytokines, which increase the ratio of type 2 helper (Th2) T cells to Th1 cells. This leads to increased levels of immunoglobulin E (IgE) and eosinophilia, in addition to increased basophil and mast cell degranulation. Despite the cause, biopsy specimens of eczematous lesions reveal epidermal intracellular edema and dermal perivascular intracellular T-cell infiltration.1
Diagnosis
A good history and physical examination are usually adequate to make the diagnosis of eczema. Patients often offer a personal or family history of atopy, allergic rhinitis, or asthma.1
Clinical Complications
Complications include bacterial superinfection, typically with Staphylococcus aureus. Studies show that use of antibacterial soaps lowers the colonization of eczematous lesions.2
Management
Several modalities have been devised for the treatment of eczema. These include skin hydration, short-course topical corticosteroids, antihistamines for symptomatic relief of pruritus, and avoidance of irritants. Maintenance topical corticosteroids are not recommended, because they can potentially cause skin atrophy, hypopigmentation, and immunosuppression.1 Immunomodulators that block T-cell activation, such as pimecrolimus and tacrolimus, have been shown to be more beneficial than corticosteroids, because they do not appear to induce systemic immunosuppression or cutaneous atrophy.1,2
REFERENCES
1. Beltrani V. Clinical features of atopic dermatitis. Immunol Allergy Clin North Am 2002;22;25-42.
2. Boguniewicz M. Conventional therapy for atopic dermatitis. Immunol Allergy Clin North Am 2002;22;107-124.
14-9 Contact Dermatitis
Colleen Campbell
Clinical Presentation
Patients usually present with intense itching in the area of contact. An acutely demarcated area of erythema, edema, papules, and vesicles can be seen in the area of skin contact.1 In more extreme cases, there may be serous drainage from the involved site. Dry, chapped skin with erythema is seen more often with irritant contact dermatitis.1 The hands are the most commonly affected site, followed by the face (especially the eyelids).1 In children, areas commonly affected are the diaper area and the face, especially in the perioral region (i.e., “lip licker dermatitis”).1
Pathophysiology
Contact dermatitis is a local skin reaction that occurs in response to an immunologic, chemical, mechanical, or physical mediator applied to the skin.1
Contact dermatitis may be allergic- or irritant-mediated.1 Both types have similar time courses from exposure to reaction, and they are difficult to differentiate.1 Allergic-mediated contact dermatitis can occur after a single exposure or after years of chronic exposure. This is a type IV allergic reaction.2 The most common allergic-mediated contact dermatitis in North America is from poison oak or poison ivy exposure.2 Neomycin, nickel, and components of rubber (especially latex) are common causes of allergic contact dermatitis.2 Wool is also a common contact irritant.3 Irritant contact dermatitis is most often the result of repeated contact with low-grade physical, mechanical, or chemical irritants.1 This may occur as a result of repeated hand washing or from natural irritants such as saliva. Light-skinned individuals are more commonly affected.2
Diagnosis
The diagnosis is made largely on the basis of a careful history and physical examination. The exact cause of allergic contact dermatitis often is difficult to determine, because the exposure can antedate the reaction by as much as 2 weeks, as in the case of primary sensitization.2 Referral back to the patient’s primary care doctor for patch testing may be necessary in cases of chronic contact dermatitis.2
Clinical Complications
Complications associated with contact dermatitis are not common. However, bacterial superinfection of affected areas is the most common complication.4
Management
In most cases, elimination of contact with the irritant suffices. Oral antihistamines may be used for pruritus, in addition to topical corticosteroid creams.2 In more severe cases with vesicles and serous drainage, Burow’s solution (aluminum acetate) with wet-to-dry dressings may further facilitate healing.2
REFERENCES
1. Rietschel RL. Comparison of allergic and irritant contact dermatitis. Immunol Allergy Clin North Am Aug 1997;17:359-364.
2. Shaw JC. Allergic and non-allergic eczematous dermatitis. Immunol Allergy Clin North Am 1996;16:119-134.
3. Beltrani VS. Clinical features of atopic dermatitis. Immunol Allergy Clin North Am 2002;22:25.
4. Friedlander SF. Contact dermatitis. Pediatr Rev 1998;19:166-171.
14-10 Nickel Dermatitis
Colleen Campbell
Clinical Presentation
Patients with nickel dermatitis usually present with an intense itching in the area of contact. An acutely demarcated area of erythema, edema, papules, and vesicles can also be seen in the area of contact.1 The hands are the most commonly affected area, and nickel dermatitis is an occupational hazard for many workers.2 Women who wear jewelry composed of nickel may present with erythema of the earlobes or in the neck region. There have been reported cases of inhalation exposure to nickel causing a widespread papuloerythematous rash several hours after exposure.2
Pathophysiology
Nickel is the metal that most commonly causes contact dermatitis.2 Nickel dermatitis can occur after one exposure or after years of exposure. This is a type IV allergic reaction. Women and younger individuals are most commonly affected by nickel dermatitis.3 Approximately 10% of people who undergo patch testing (using 5% nickel sulfate) are sensitized to nickel.3 Occupations with risk for nickel sensitization include metal furnace operator and electroplater.3
Diagnosis
The diagnosis of nickel dermatitis is suspected by careful history and physical examination. It can be confirmed after referral back to the patient’s primary care doctor for patch testing, with results usually available after 3 days.3
Clinical Complications
Complications from contact dermatitis are rare. Bacterial superinfection of affected areas is the most common complication.
Management
In most cases, elimination of contact with the nickel suffices. Oral antihistamines may be used for pruritus, in addition to medium- to high-potency topical corticosteroid creams.1 In more severe cases when vesicles and serous drainage are present, Burow’s solution (aluminum acetate) with wet-to-dry dressings may further facilitate healing.1 Patients with work-related exposures should be referred to an occupational medicine specialist for further follow-up.
REFERENCES
1. Shaw JC. Allergic and non-allergic eczematous dermatitis. Immunol Allergy Clin North Am 1996;16:119-134.
2. Candura SM, Locatelli C, Butera R, Gatti A, Fasola D, Manzo L. Widespread nickel dermatitis from inhalation. Contact Dermatol 2001;45:174-175.
3. Uter W, Pfahlberg A, Gefeller O, Geier J, Schnuch A. Risk factors for contact allergy to nickel: results of a multifactorial analysis. Contact Dermatol 2003;48:33-38.
14-11 Psoriasis
Michael Greenberg
Clinical Presentation
Pathophysiology
The precise cause of psoriasis is not known. However, a genetic predisposition is probable, because there is an increased prevalence of this disease among family members. Psoriasis has been associated with specific human leukocyte antigens. Psoriasis clearly involves excessive proliferation of keratinocytes, as well as a substantial decrease in the time required for epidermal cells located within psoriatic plaques to divide. Altered immune mechanisms are probably involved, because activated T cells, and upregulation of immune-mediated adhesion molecules on keratinocytes have been observed. In addition, psoriasis may improve with treatments that modify cutaneous T-cell infiltration.1,2
Diagnosis
Psoriasis is a chronic skin disease with distinctive cutaneous lesions. Usually, the diagnosis is easily made on clinical examination by finding erythematous and well-demarcated cutaneous plaques, commonly located on the extensor surfaces of the elbows and knees, on the scalp, and in the lumbosacral region.1,2 The most common form of psoriasis is the chronic plaque form known as psoriasis vulgaris, which accounts for approximately 90% of cases. Characteristic nail findings include pits and areas of yellowish discoloration known as “oil spots.” Thickened and yellow nail plates occur in up to 50% of patients.1,2
Clinical Complications
Complications include local skin infections, and psoriatic arthritis, which occurs in up to 20% of cases. Psoriatic arthritis appears to be more common in patients who have nail and scalp psoriasis. Mechanical, chemical, or ultraviolet (UV) injury to the skin may result in the Koebner phenomenon (local skin damage followed by development of the disease state in that previously normal area of skin).1,2 Various infections, including streptococcal and acute viral infections, may trigger the development of psoriatic lesions.1,2
Management
Although no treatment is curative, various therapies may be effective. The emergency physician is rarely called upon to initiate or alter therapy. Current treatment regimens may include emollients, keratolytics, corticosteroids, tar, anthralin, vitamin D analogues, retinoids, phototherapy, acitretin, methotrexate, cyclosporine, and the Goeckerman treatment, or a combination of these.3
REFERENCES
1. Espinoza LR, van Solingen R, Cuellar ML, Angulo J. Insights into the pathogenesis of psoriasis and psoriatic arthritis. Am J Med Sci 1998;316:271-276.
2. Peters BP, Weissman FG, Gill MA. Pathophysiology and treatment of psoriasis. Am J Health Syst Pharm 2000;57:645-659.
3. Witman PM. Topical therapies for localized psoriasis. Mayo Clin Proc 2001;76:943-949.
14-12 Atopic Dermatitis
Harneet Sethi
Clinical Presentation
Pathophysiology
The precise causes and mechanisms involved in AD are not fully understood. The role of provoking allergens has been suggested, but in some studies refuted. AD appears to be an immune disturbance that involves increased immunoglobulin E (IgE) levels in conjunction with T-cell dysregulation.1 Histamine release is not involved in AD.
Diagnosis
Criteria for the diagnosis of AD include the presence of a pruritic skin rash within the past 12 months (obligatory), plus three or more of the following: history of flexural dermatitis, onset before the age of 2 years, personal history of asthma or hay fever, history of dry skin, and visible flexural dermatitis.2 More detailed criteria have been delineated in the past, but they are too burdensome to be used in the emergency department (ED). Laboratory testing is of limited value in the ED setting; however, an elevated serum IgE value may be helpful in making the diagnosis.3
Clinical Complications
Complications include bacterial and viral superinfections.
Management
Dermatologic referral is appropriate in all cases. Sweat and skin heat are often provoking factors, and avoidance is recommended. Bathing in lukewarm water and use of mild soaps are recommended; emollients may be applied to moist skin to maximize moisture retention.1 Midpotency steroids may be applied twice daily for AD exacerbations. Antibiotics should be reserved for use with evidence of infection.
REFERENCES
1. Borirakchanyavat K, Kurban AK. Atopic dermatitis. Clin Dermatol 2000;18:649-655.
2. Thestrup-Pedersen K. Clinical aspects of atopic dermatitis. Clin Exp Dermatol 2000;25:535-543.
3. Williams HC, Burney PG, Pembroke AC, et al. The UK Working Party’s diagnostic criteria for atopic dermatitis: derivation of a minimum set of discriminators for atopic dermatitis. Br J Dermatol 1994;131:383-396.
14-13 Hidradenitis Suppurativa
Michael Greenberg
Clinical Presentation
Many patients present knowing that they carry the diagnosis of hidradenitis suppurativa (HS), and that history is forthcoming. These patients present with pain, swelling, itching, bleeding, and purulent drainage from multiple sinus tracts in the axillae and/or anogenital areas. Other patients first present at the onset of puberty with tender subcutaneous nodules and deep abscesses that are characteristically round in shape. HS-related abscesses tend to manifest initially with symmetric lesions in the axillary or anogenital regions.1,2,3
Pathophysiology
Women are more commonly affected than men (3:1). The disease incidence peaks in the second and third decades of life and declines by the fifth decade. The precise cause of HS is not certain; however, genetic predisposition and various endocrine factors appear to be important. Obesity is an exacerbating factor. There appears to be an association between HS development and smoking. Coagulase-negative staphylococci and Staphylococcus aureus organisms are frequently isolated from patients with HS.1
Diagnosis
The diagnosis is made based on clinical findings of multiple recurrent anogenital and axillary abscesses, purulent draining sinus tracts, and fistulas.
Clinical Complications
Complications include fibrosis and scarring with contracture formation and decreased mobility of extremities. Fistulas may develop in the anorectal and urethral areas. Other complications include frequent recurrences, anemia, squamous cell carcinoma, arthropathies, amyloidosis, renal failure, and death.
Management
Medical management involves encouraging weight loss, smoking cessation, and meticulous local care of abscesses and fistulas. Topical and enteral clindamycin is helpful in many cases. Antiandrogen therapy and finasteride may be helpful. Retinoids and immunosuppressive doses of corticosteroids may also be useful. Recent reports of radiotherapy for HS are impressive but unconfirmed. Surgical treatment is probably the best option for severe cases; it may range from simple drainage to radical excision procedures.1,2
REFERENCES
1. Slade DE, Powell BW, Mortimer PS. Hidradenitis suppurativa: pathogenesis and management. Br J Plast Surg 2003;56:451-461.
2. Tanaka A, Hatoko M, Tada H, Kuwahara M, Mashiba K, Yurugi S. Experience with surgical treatment of hidradenitis suppurativa. Ann Plast Surg 2001;47:636-642.
3. Silverberg MA, Rahman MZ. Axillary breast tissue mistaken for suppurative hidradenitis: an avoidable error. J Emerg Med 2003;25:51-55.
14-14 Cutaneous Abscess
Matthew Pius
Clinical Presentation
Patients with cutaneous abscess may present with localized swelling that may or may not be painful or tender. Fever generally is not reported unless bacteremia has occurred.
Pathophysiology
Abscesses typically arise after a break in the skin, which provides bacteria a portal of entry through the protective, cornified layers of the epidermis.1 Intertriginous areas, where the skin may become macerated, and shaved areas, where there may be microabrasions, are particularly prone to abscess formation.1,2 Skin flora (e.g., Staphylococcus aureus) are commonly responsible for skin abscess formation, although most collections contain a mixture of aerobic and anaerobic bacteria.1 Lesions in the inguinal and perineal area may contain a predominance of anaerobes (especially Bacteroides species) and other normal flora of the anorectal region.2
Diagnosis
On physical examination, a fluctuant mass may be present. These are often exquisitely tender to palpation. There may be erythema and warmth of the surrounding skin if cellulitis has also developed. Spontaneous drainage of pus may be seen. Lymphangitis and lymphadenopathy may also be present.1
Clinical Complications
Abscesses may spread to the surrounding skin, resulting in localized cellulitis. They may also track through the skin, forming fistulas that may or may not persist. The collection can penetrate the skin into deeper structures, resulting in abscess formation within the muscle or osteomyelitis. Untreated abscesses can also result in bacteremia, sepsis, and death.
Management
The definitive treatment for an abscess is surgical incision and drainage. If the abscess cavity is sizable, it should be packed with sterile packing material to prevent resealing of the incision site and reaccumulation of pus. Because the abscess cavity itself has very little vascular supply, systemic antibiotics are not well delivered to the site of infection. However, those patients whose clinical picture suggests bacteremia or other systemic infection, those with immunocompromise, and those with overlying cellulitis may benefit from systemic antibiotics.1,2 Impending abscess formation (i.e., advanced cellulitis that has not yet organized into a collection of pus) should be treated with 10- to 15-minute soaks in warm water every 2 hours, to accelerate organization of the pus collection and to stimulate possible spontaneous drainage.1,2
REFERENCES
1. Caruthers LD, Griggs R, Snell GF. Office management of epithelial cysts and cutaneous abscesses. Prim Care 1986;13:477-491.
2. Meislin HW, McGehee MD, Rosen P. Management and microbiology of cutaneous abscesses. JACEP 1978;7:186-191.
14-15 Scabies
Aman Parikh
Colleen Campbell
Clinical Presentation
Patients with scabies complain of an intensely pruritic rash. The pruritus may be more severe at night and may affect any part of the body, but the most commonly affected areas are the interdigital web spaces, axillae, genital area, buttocks, and breasts.1
Pathophysiology
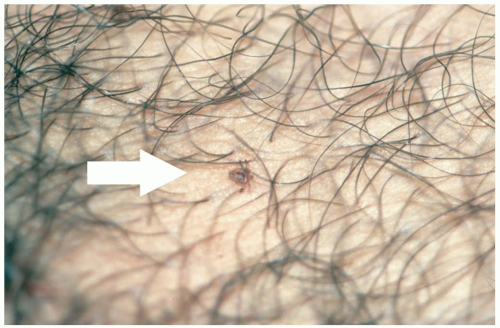
Sarcoptes scabiei var. hominis is a mite, approximately 0.5 mm in length, that causes human scabies. The female mite burrows under the skin and produces eggs and scybala. A type IV delayed hypersensitivity reaction occurs after approximately 1 month in unsensitized patients or within hours in sensitized patients. This leads to the severe pruritus that is characteristic of scabies infection.
Diagnosis
If scabies is suspected, the diagnosis can be confirmed by opening of a burrow or other skin lesion with a number 15 scalpel blade. The contents are placed on a slide, and a drop of oil is applied. Diagnosis is confirmed with identification of mites, eggs, or scybala (feces) on microscopic examination.
Clinical Complications
Complications are usually limited to secondary infection, and are usually a problem only in immunocompromised patients. A generalized form of scabies (Norwegian or “crusted” scabies) is associated with severe secondary infections in immunocompromised patients.2 This form of scabies caused hyperkeratosis and an erythematous rash of the face, trunk, and extremities. Crusted scabies is highly contagious and is a special risk for health care workers. Pruritus may last for months after successful treatment of the infection.
Management
Treatment of scabies involves topical application of lindane, permethrin, or a sulfur agent. Lindane 1% lotion is not recommended for children younger than 2 years of age, because of the potential neurotoxicity and risk of aplastic anemia. Patients who are allergic to chrysanthemums, as well as pregnant and lactating women, should not be given lindane. Permethrin (5%) can be used for infants as young as 2 months of age and should be applied for 8 to 14 hours. This is considered the treatment of choice, with a cure rate in excess of 90%.1 Sulfur ointment 6% (applied for three consecutive nights) is an alternative treatment.2 Patients need to be advised to wash and dry all clothing and sheets to prevent reinfection. Sulfur ointment has not yet been approved by the U.S. Food and Drug Administration (FDA) for treatment of scabies. Close household contacts and sexual contacts should be treated to avoid reinfection.3
REFERENCES
1. Morgan-Glenn PD. Scabies. Pediatr Rev 2001;22:322-323.
2. Brook I. Secondary bacterial infections complicating skin lesions. J Med Microbiol 2002;51:808-812.
3. Buffet M, Dupin N. Current treatments for scabies. Fundam Clin Pharmacol 2003;17:217-225.
14-16 Head Lice
Edgar Collazo
Clinical Presentation
Patients with head lice present with scalp pruritus, although some patients are asymptomatic. Head lice infestation is usually discovered by another person, who sees the nits or lice. The eggs or nits are tiny, white ovals less than 1 mm in length that adhere to the hair shaft. The louse is 2 to 3 mm in length, has six legs, and may be seen on the scalp.
Pathophysiology
Pediculosis capitis is the infestation of a human scalp by the tiny head louse, Pediculus humanus capitis. It is common in children 3 to 12 years of age. A female louse can lay more than 100 eggs during the span of 3 to 4 weeks. The eggs are attached to the hair shaft close to the scalp by a glue-like substance.1,2,3 Head lice do not jump from person to person, nor can they fly, so transmission comes from close, prolonged head-to-head contact such as co-sleeping, sharing hats, and sharing combs or brushes.1,2,3
Diagnosis
A positive diagnosis can be made on seeing a live, active head louse. Visualization of nits on the scalp of a child is not sufficient to diagnose active lice infestation, because the eggs tend to remain attached long after the louse has hatched.
Clinical Complications
There are no clinical complications; however, most children are sent home from school on discovery of the infestation.
Management
Over-the-counter topical pyrethroids are available. These usually destroy the lice but not the eggs; therefore, a second treatment is recommended after 7 to 10 days. Persistent scalp itching without visualization of live lice does not warrant reapplication. Prescription lice treatment is available in the form of malathion 0.5% lotion or lindane 1%. Lindane is absorbed through the skin and can cause seizures or death if applied improperly, applied too often, or given to the very young. Bed linens, towels, and clothes must be washed in hot water. Items that cannot be washed should be dry cleaned. Brushes and combs must be soaked in hot, soapy water for at least 1 hour. Floors and furniture must be vacuumed, including the car seats of younger children. Stuffed animals should be washed if the child sleeps with them.1,2,3
REFERENCES
1. Dolianitis C, Sinclair R. Optimal treatment of head lice: is a no-nit policy justified? Clin Dermatol 2002;20:94-96.
2. Meinking TL, Burkhart CG, Burkhart CN. Head lice. N Engl J Med 2002;347:1381-1382.
3. Hill N. Treatment of head lice. Lancet 2000;356:2007.
14-17 Pubic Lice
Colleen Campbell
Clinical Presentation
The most common clinical symptom of pubic lice infestation is pruritus, which occurs in 85% of cases.1 Patients often have very few lice during infection, so pubic hair must be inspected carefully for the presence of 1- to 2-mm, brown-colored lice.2 Other findings suggestive of infestation are maculae caeruleae, bluish-gray macules that appear at feeding sites; rust-colored fecal material may be evident as well.2
Pathophysiology
Phthirus pubis are approximately 1 mm in size and have three sets of legs. They can live away from human hosts for up to 24 hours.1 Pubic lice are easily transmitted via physical contact.2 The most common mode of transmission is through sexual contact. Rarely, they can also be found in facial hair, thigh hair, and eyelashes.3 Men are infected more commonly than women, possibly because women typically have less pubic hair.3 Eggs are attached to the base of hair follicles and mature over the next 3 weeks to become adults. Adults can lay up to 100 eggs during their lifespan of 1 month.2
Diagnosis
The diagnosis of pubic lice is based on clinical evidence of disease. To confirm the diagnosis, hair follicles may be examined under low-power microscopy.2
Clinical Complications
The most common complication of infestation is spread to other individuals. Bacterial superinfection can occur as a result of excoriation.
Management
Treatment of pubic lice is with topical lindane, permethrin, or pyrethrins. Lindane 1% is applied to the affected area for 4 minutes.4 Complications from lindane use for this limited amount of time are very rare. However, this treatment is contraindicated in women who are pregnant or lactating and in children younger than 2 years of age because of the risk of seizures and aplastic anemia.2 Treatment with permethrin (1% crème) or pyrethrins should be for 10 minutes. Treatment may need to be repeated in 1 week if symptoms persist.4
All clothing and bedding should be washed to prevent reinfestation. Nits can be removed with a fine-toothed comb. Because one third of patients infested with pubic lice have a concomitant sexually transmitted disease, all patients should be screened and treated appropriately.2 Urethritis and vulvovaginitis were the most commonly associated sexually transmitted diseases in one study.3 All sexual partners (contacts within the previous month) should be treated as well.4
REFERENCES
1. Ko WT, Adal KA, Tomecki KJ. Infectious diseases. Med Clin North Am 1998;82:1001-1031.
2. Brown TJ, Yen-Moore A, Tyring SK. An overview of sexually transmitted diseases: part II. J Am Acad Dermatol 1999;41:661-677.
3. Varela JA, Otero L, Espinosa E, Sanchez C, Junquera ML, Vazquez F. Phthirus pubis in a sexually transmitted disease unit: a study of 14 years. Sex Transm Dis 2003;30:292-296.
4. Workowski KA, Levine WC. CDC STD treatment guidelines 2002. MMWR Morb Mortal Wkly Rep 2002;51(RR-6):1-78.
14-18 Pityriasis Rosea
Anthony S. Mazzeo
Clinical Presentation
Patients with pityriasis rosea (PR) usually present in the second or third decade of life complaining of a diffuse and itchy rash, which may be associated with a viral prodrome that includes fever, headache, fatigue, malaise, and arthralgias.
Pathophysiology
Various factors support a viral origin, including a predilection for fall and spring months, increased incidence among immunocompromised persons, lifelong immunity after the rash, and case clusters.1 Human herpes virus-6 (HHV-6) or HHV-7 may be the inciting factor, although a definitive association remains controversial.2 A PR-like rash may appear in conjunction with use of medications such as captopril, metronidazole, clonidine, and barbiturates.3
Diagnosis
Diagnosis is based on clinical examination; 50% of patients have or recall having a “herald patch,” which is a lone, erythematous area, 2 to 10 cm in diameter, with raised, edematous borders. This lesion is usually on the trunk, but it may be located elsewhere. Between 7 and 10 days after the appearance of the herald patch, a diffuse eruption of smaller, pink, oval-shaped, papulosquamous patches appears along the skin tension lines. This distribution of the lesions leads to the so-called “Christmas tree” pattern on the back. They have a fine scale that may be located around the edges. The lesions can coalesce and recur.
Clinical Complications
PR can last for months, with a waxing and waning course. The course is generally benign and healing complete, although patients should be informed that postinflammatory pigmentation changes may persist.3 If lesions persist for longer periods or are associated with other symptoms, the patient should be referred for dermatologic evaluation for psoriasis guttata and other conditions that mimic PR.
Management
Education and reassurance are the most important aspects of treatment for this benign, self-limited entity. Ultraviolet (UV) light has been reported anecdotally to shorten the duration, but it has no documented long-term benefit and in some cases may worsen changes in pigmentation. For those patients who experience pruritus, standard oral antihistamines may ease symptoms. Topical steroids may also provide symptomatic relief. Despite the recent evidence of HHV association and studies showing that erythromycin may hasten resolution, at this time antimicrobial therapy is not indicated.2
REFERENCES
1. Chuh AA, Lee A, Molinari N. Case clustering in pityriasis rosea: a multicenter epidemiologic study in primary care settings in Hong Kong. Arch Dermatol 2003;139:489-493.
2. Watanabe T, Kawamura T, Jacob SE, et al. Pityriasis rosea is associated with systemic active infection with both human herpesvirus-7 and human herpesvirus-6. J Invest Dermatol 2002;119:793-797.
3. Allen RA, Janniger CK, Schwartz RA. Pityriasis rosea. Cutis 1995;56:198-202.
14-19 Bullous Impetigo
Dziwe Ntaba
Clinical Presentation
Bullous impetigo (BI) is a common cutaneous infection that is seen primarily in infants and children. Presenting signs are typically flaccid blisters and bullae measuring between 0.5 and 3 cm in diameter.1 Their distribution can be either local or diffuse, and they typically occur on the face. The trunk, perineum, and extremities can also be affected.1,2
Pathophysiology
BI is caused almost exclusively by coagulase-positive Staphylococcus aureus, although involvement of streptococcal species has been reported. The staphylococcal epidermolytic toxin is thought to be responsible for the tenderness and bullae formation that are characteristic of the disease.1 Infection usually occurs in the absence of any apparent prior injury to the skin. If untreated, the bullae rupture in 1 to 2 days, leaving a honey-colored crust and superficial erosions.
Diagnosis
The diagnosis can usually be made on clinical grounds, but atypical presentations may resemble thermal or chemical burns.1 Definitive diagnosis may be established by biopsy; however, this is reserved for unusual cases.
Clinical Complications
Complications (usually seen in infants) include local extension of infection that leads to osteomyelitis or septic arthritis. If the infection involves phage-group II, type-71 Staphylococcus, then larger bullae (up to 8 cm) may form as the toxin produces intradermal cleavage.2 More severe but unusual presentations of this spectrum include staphylococcal scalded skin syndrome (SSSS), which involves generalized epidermolysis with desquamation.3
Management
Azithromycin and cephalosporins are the currently recommended drugs of choice. Dicloxacillin and first-generation cephalosporins are acceptable alternatives. Some fluoroquinolones have been shown to be effective, but they currently are approved only for adults. Erythromycin is no longer recommended because of microbial resistance.2
REFERENCES
1. Scales JW, Fleischer AB Jr, Krowchuk DP. Bullous impetigo. Arch Pediatr Adolesc Med 1997;151:1168-1169.
2. Stulberg DL, Penrod MA, Blatny RA. Common bacterial skin infections. Am Fam Physician 2002;66:119-124.
3. Edlich RF, Horowitz JH, Nichter LS, Silloway KA. Morgan, RF. Clinical syndromes caused by staphylococcal epidermolytic toxin. Compr Ther 1985;11:45-48.
14-20 Pemphigus Vulgaris
Reid Brackin
Clinical Presentation
Patients with pemphigus vulgaris (PV) may present with blisters or erosions of the skin, lesions in the mouth, secondary complications of the disease, or poor control of symptoms.
Pathophysiology
PV is a rare autoimmune disease involving mucocutaneous blister formation. Immunoglobulin G (IgG) antibody is targeted against desmoglein-3, an adhesion protein found in desmosomes, disturbing these main adhesion structures of the epidermis. The result is acantholysis (separation between keratinocytes), suprabasilar blister formation, and mild superficial dermal inflammatory infiltrate. The exact mechanism remains controversial.1,2
 FIGURE 14-20 Intraepidermal blistering and dermal disruption characteristic of pemphigus vulgaris. (© David Effron, MD, 2004. Used with permission.) |
PV is the most common form of pemphigus. Other major types include pemphigus foliaceus and paraneoplastic pemphigus. Frequency is increased in people of Mediterranean or Jewish descent. The mean age at onset is between 50 and 60 years. Men and women are equally affected.1,3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree