Depression: The Sad Child
Enitza D. George MD
INTRODUCTION
A sad or dysphoric mood that generally is transient and occurs in response to negative events is common among children and adolescents. The term “depression” may refer to symptoms of depression, a depressive syndrome, or a depressive disorder. Depression as symptoms refers to the child’s mood or emotional feeling. Depression as a syndrome includes vegetative, psychomotor, and cognitive changes. If a depressive syndrome lasts for 2 weeks or more and causes marked dysfunction, then it is considered a depressive disorder.
Depression can affect individuals at any time in life. Substantial differences exist, however, between children and adults in the clinical expression of depression and responses to specific treatments. Among patients who were depressed as children or adolescents, a high rate of suicide, recurrence of symptoms, and continuation of depressive illness extends into adulthood (Kent et al., 1997). Certainly, early recognition and effective management of depression are essential for all age groups but particularly in childhood when individuals acquire most of their social and cognitive skills.
Ethnic and cultural factors can influence the presentation of depression. Furthermore, these factors can make interpretation of symptoms difficult or lead to misinterpretation if the provider is not culturally aware. In addition, when assessing children, clinicians require a clear understanding of what is developmentally normal and age-appropriate to identify risk factors and diagnose pathology. The reader is referred to Chapter 8, Chapter 9, Chapter 10, Chapter 11 and Chapter 12 for more information.
• Clinical Pearls
The clinical presentation of and assessment for depression vary across the life span.
The most important clue in diagnosing depression in a child is a change in mood, affect, or behavior that is not easily explained.
There are no robust markers for mental illness, and given the wide range of “normal behaviors” in children, it may be difficult to make a definitive diagnosis (Jensen & Watanabe, 1999). Symptoms of sadness and low spirit are common at all ages, especially during times of rapid changes. When such symptoms are persistent and intense, however, they should alert clinicians to the possibility of depression.
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
Strong evidence supports a genetic predisposition to depression. Adoption studies are compelling, documenting up to an eight-fold increase in depression among biologic relatives of adoptees with affective illness (Jellinek & Snyder, 1998). The reader is referred to Chapter 6 for more information about adoption.
Major depressive disorder in a grandparent or parent is associated with depression and other mood disorders in the child (Warner et al., 1999). The concordance rate of depression between monozygotic twins (76%) is much higher than between dizygotic twins (19%) (Jellinek & Snyder, 1998). Familial cases of major depression are characterized by earlier onset, longer duration, intermediate levels of recurrence, high levels of impairment, and recurrent thoughts of death or suicide (Kendler et al., 1999).
Several neuroendocrine abnormalities have been implicated in the pathogenesis of depression. Theorists have hypothesized that dysfunction may be found in the serotonergic, catecholaminergic, and dopaminergic systems. In particular, studies report a relative or absolute serotonergic deficiency in major depression (Lestra et al., 1998). The exact mechanism leading to a relative deficiency of serotonin is unknown. Both children and adults who are depressed are known to have cortisol hypersecretion, dexamethasone nonsuppression, hyposecretion of growth hormone in response to an insulin challenge, and sleep electroencephalographic abnormalities (Jellinek & Snyder, 1998). The clinical significance of these findings is still under evaluation.
Children with depression may have relative right posterior hemisphere dysfunction and difficulty processing receptive affective modulations in pitch, timing, and volume of speech (Emerson et al., 1999). As a result, these children have significantly decreased abilities to recognize happy, angry, sad, and neutral voice inflections within congruent and incongruent verbal statements.
Stress has long been recognized as a key element in the etiology of depression. Rejection or abuse may be a precipitating factor, especially in genetically susceptible children. Chronic diseases, emotional or financial deprivation, and loss are common antecedents to depression in children. Children with diabetes, for example, have a high incidence of depression. Early identification and treatment of the affective disorder will ease the management of the metabolic disorder (Lernmark et al., 1999). Chapter 27 and Chapter 49 may offer further insights into how exogenous issues can potentiate depression.
EPIDEMIOLOGY
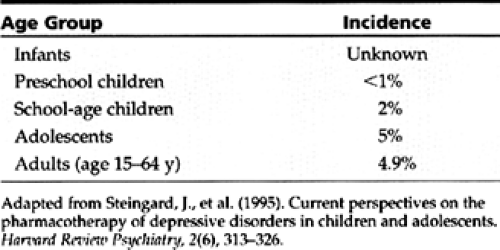
The incidence and prevalence of depression in the pediatric population vary according to age group evaluated, sampling methods, diagnostic criteria, and measurement techniques. In general, the prevalence of major depression in children is about 2% and in adolescents is about 4% to 8% (Table 28-1) (AACAP, 1998).
Current statistics suggest that the prevalence of depression in children is rising. Some experts also suggest that the onset for a first major depressive episode is occurring at
younger ages (Kovacs & Gatsonis, 1994). It is not clear if these observations indicate an impending epidemic of depression in the pediatric population or are a result of better diagnostic instruments.
younger ages (Kovacs & Gatsonis, 1994). It is not clear if these observations indicate an impending epidemic of depression in the pediatric population or are a result of better diagnostic instruments.
Prepubertal rates of depression are similar for both genders. After puberty, the female to male ratio for depression is 2:1 (Jellinek & Snyder, 1998). Depression is more prevalent among children who experience emotional or financial deprivation and in children affected with chronic debilitating diseases.
HISTORY AND PHYSICAL EXAM
If parents express concerns about their child’s emotional development, providers should explore both explicit and implicit concerns. History taking and physical examination should focus not only on the child’s difficulties but also on the child’s strengths and attributes (Thomas, 1998).
Infants, Toddlers, and Preschoolers
Differences between the child’s temperament and parental expectations may contribute to stressful family relationships. The provider should gather a history of the child’s past and current difficulties and how they are affecting family dynamics. The provider must ask about the parent’s own childhood experiences, as well as the experiences of the child’s older siblings. Finally, the clinician needs to assess the degree to which these experiences contribute to the parent’s view of the child’s behavior.
In obtaining the history, providers should remember that parents often feel anxious or guilty and may fear that the provider is questioning their parenting skills. Clinicians must be cognizant that how they ask questions may influence such feelings.
In undertaking the history, the provider needs to gather data on familial medical and psychiatric disorders. To obtain a complete history, it may be necessary and appropriate to interview as many individuals as possible who have knowledge of the family and the child’s current and past functioning. Besides parents, older siblings, and other caregivers, providers may include baby sitters, grandparents, aunts, and uncles.
The provider should perform a complete physical exam, ascertaining that no organic condition can explain parental concerns. Interdisciplinary assessment may unmask other areas of concern. The clinician should consider adjunctive assessment by developmental experts, as well as referrals for child psychology, neurology, genetics, nutrition, ophthalmology, audiology, speech and language therapy, occupational therapy, physical therapy, or social and educational services as indicated. Adjunctive assess ment should occur in a variety of settings, including the patient’s home, child care agency, school, or other settings where the child spends time. These adjunctive assessments can assist in the diagnosis and evaluation of a child and are helpful in tracking the patient’s progress once treatment begins. Refer to Chapter 21 and Chapter 22 for further discussion of co-morbidity and management information.
If feasible, the provider may want to consider scheduling a session for clinical observation of the child’s interaction with parents. A pediatric social worker can assist in providing for this observation, its assessment, and interpretation. Providers must inform parents of the purpose of the session, which should last at least 15 to 20 minutes. The session involves observing the family in a small carpeted room with a few age-appropriate toys. The examiner notes the quality of parent-child behavior and the child’s reaction to brief parental separation and reunion. If the referral concern involves feeding problems, the professional making the assessment needs to observe the child and parent during feeding. Videotaping the session may serve as an adjunct for further discussion with the parents. When compared, serial videotapes can assist in evaluating progress after initiation of treatment (Thomas, 1998).
School-age Children
In taking the history, the provider needs to ask about family dynamics, including history of marital discord, birth of a new child, illness, or death. Questions such as “Did the family recently move?” can be illuminating. Even relatively local moves can be disturbing, especially if a child “loses” neighborhood friends and schoolmates. The clinician also needs to gather information about the child’s participation in school. He or she also should ask whether the parents have noted a recent deterioration in grades. Providers also can suggest that parents question the child’s teacher and as many classmates as possible for a complete picture of the child’s functioning. If the child participates in sports or other extracurricular activities, the provider may want to ask coaches about recent changes in performance during these activities. The reader is referred to Chapter 27 for further understanding of situations that can trigger depression. Chapter 29 can offer further insight for providers who are dealing with children who have more serious problems.
Some depressed children try desperately to compensate for feelings of poor self-worth by attempting to please others, trying not to cause trouble, and “being good” (Jellinek & Snyder, 1998). In reality, such behavior only affords temporary relief for a sense of failure. Behind these struggles, depression persists. If a provider is considering a diagnosis of depression, he or she should investigate any inexplicable change in the child’s behavior, even if seemingly “good.”
Adolescents
As with younger children, obtaining the history directly from the patient is useful. Indirect information from parents, teachers, coaches, and friends also may prove helpful. Providers should keep in mind that there may be poor correlation between adolescent self-report of depression and parental report (Kent et al., 1997). When evaluating adolescents, providers must be as clear, concise, and specific as possible in history taking, within the context of the teen’s
developmental stage. They also must assure patients of the confidential nature of all conversations.
developmental stage. They also must assure patients of the confidential nature of all conversations.
• Clinical Pearl
Providers should be available by phone or e-mail in case adolescents would like to add to any information they provided during their visit.
It is of paramount importance for providers to ask children directly and clearly about ideas or plans for committing suicide. They also should ask about access to firearms and ammunition.
A more mature dysphoric mood is a hallmark of puberty, thus increasing the risk of acting on such feelings by committing suicide (Jellinek & Snyder, 1998). The 1997 Youth Risk Behavior Surveillance revealed that 7.7% of adolescents with depression had attempted suicide during the previous year (MMWR, 1998). Asking about ideas regarding death will not increase the risk of suicide. Instead, such questioning will give adolescents an opportunity to discuss their thoughts and feelings. Providers should remember, however, that there is no way to predict suicide among depressed children and adolescents, except in those who have made previous attempts (Jellinek & Snyder, 1998).
Besides suicide, practitioners must ask about alcohol and drug use. Not only will this information identify adolescents at risk for depression, but also will alert others to the possibility of accidental suicide while under the influence of a drug. Of similar importance is to ask about weapon availability and membership in gangs. Refer to Chapter 25, Chapter 26, and Chapter 29 on for more information.
Finally, the provider should gather information about the seasonality of symptoms, symptom clusters, atypical symptoms, psychosis, and hypomania. Such data will assist in making a differential diagnosis. They also will help identify subtypes of depression that may require special treatment strategies.
DIAGNOSTIC CRITERIA
The Diagnostic and Statistical Manual IV criteria for major depression emphasize that the “core” symptoms are the same for children and adults, but that the prevalence of certain symptoms vary with age (American Psychiatric Association, 1994). For a diagnosis of depression, five or more of the following symptoms must be present during the same two-week period and represent a change from previous functioning. At least one symptom must be either depressed mood or loss of interest or pleasure in an activity. A second (or additional) symptom must come from the following:
Depressed or irritable mood
Diminished interest or pleasure in activities
Weight change or appetite disturbance
Insomnia or hypersomnia
Psychomotor agitation or retardation
Fatigue or loss of energy
Feelings of worthlessness or guilt
Disturbed concentration or indecisiveness
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree