1. The importance of clarifying roles of all physicians, RN’s and other health care personnel in the delivery room resuscitation of newborns cannot be overemphasized enough.
2. Ventilation of the lungs is the most important part of resuscitation of the newborn.
3. In situations when intubation of the newborn is done, it is essential to be certain that the endotracheal tube in in the trachea, not esophagus.
ADMINISTRATIVE ASPECTS
Successful resuscitation of the newborn begins well before birth. Issues of medical direction and decision-making responsibility come into play in ways different from most, if not all, other resuscitations in the hospital. Not only will an anesthesiologist be present, having been responsible for the anesthetic care of the parturient, but also a pediatrician or even a neonatologist will be present at the delivery of the newborn. There will also likely be registered nurses (RNs) from the neonatal nursery, unless the delivery of a well, term newborn is expected. Obstetrics (OB) nurses in the delivery room will have been trained in resuscitation of newborns and assisting the other medical professionals involved in that effort. Delivery is absolutely NOT the time to discuss and codify medical direction, the roles of the various team members, the lines of responsibility, and other aspects of the functioning of the team caring for the newborn. These issues should be fully discussed in meetings of all concerned disciplines and all-important details of the functioning of the resuscitation team should be clarified. Leadership of the involved medical and nursing departments as well as hospital leadership should be involved in these very important deliberations. There is much expertise here with the medical and nursing specialties mentioned and the newborn should receive the cooperative benefit of that expertise, not become a victim of arguments between the departments of anesthesiology and pediatrics and, if present in the institution, the division of neonatology. Frank discussions of the knowledge, experiences, and skills of the disciplines involved should take place in a meeting wherein all interested parties have the floor to express their particular points of view.
Once these potentially difficult issues are resolved, care of the newborn will depend upon cooperation between the caregivers. The process of resuscitation of the newborn must be carefully monitored for quality on an ongoing basis. Simply setting up a system, even one very carefully considered and conceived with the consensus of all involved, without critical analysis and continuous evaluation of effectiveness of any problems does not follow the currently accepted model of medical care. Regular assessment of successes and areas for improvement must take place. This sort of critical evaluation will lead to improvements. In the area of newborn resuscitation, not only will there be opportunities for improved care, but also in all likelihood the parturient population will change over time, necessitating changes in the resuscitation plans. As hospitals grow, higher-risk pregnancies tend to be cared for in-house as opposed to being transferred to distant centers. The birth of a child is such a major event and many families greatly prefer to enjoy this wonderful landmark near home rather than at a distant, impersonal medical center. The anesthesiologists involved with delivery of a newborn expected to have postnatal difficulties or even a newborn expected to have no trouble making the transition to extrauterine life should approach the delivery room as another operating room (OR), applying the same care, attention to detail, and thoroughness in preparation of an OR prior to a surgical procedure.
Proper preparation, as is well known to anesthesiologists, will allow the team involved in resuscitation of a newborn to spend their time and energy on the care of the newborn and not on a frantic search for equipment, medication, or suction. Great strides have been made in advanced cardiac life support (ACLS) and pediatric advanced life support (PALS) in improving the function of the resuscitation team by, in addition to developing algorithms for the treatment of various specific problems, also assigning distinctive roles for members of the resuscitation team (Table 34.1).
TABLE 34.1 Recommended delivery room equipment
Warming device, radiant warmer Bulb syringe Suction tubing, catheters of various sizes Functioning in-wall adjustable suction or portable suction Oxygen: wall source and back-up tank Newborn-sized face mask Bag/mask ventilation equipment Self-inflating bag Jackson-Rees type or T-piece bag Newborn, infant-sized OPAs Endotracheal tubes and stylets, 2.5, 3.0, 3.5, 4.0 Laryngoscope handles (2) Newborn-sized laryngoscope blades Neonatal LMA Pulse oximeter probe and oximeter ECG ETCO2 detector Neonatal-sized stethoscope Appropriately-sized IV catheters Umbilical vessel catheterization equipment Appropriate syringes, needles, etc. for medication administration Medications Epinephrine 1:10,000 dilution (100 μg/mL) Naloxone, 0.4 mg/mL or 1.0 mg/mL 10% dextrose 0.9% normal saline 5% albumin Sodium bicarbonate, 4.2% (0.5 mEq/mL) |
OVERVIEW OF RESUSCITATION OF THE NEWBORN
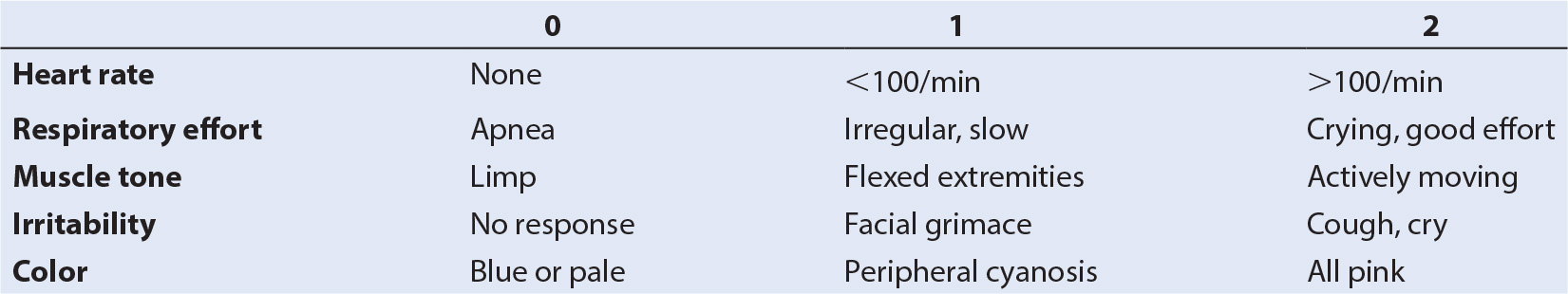
The fundamental principle of newborn resuscitation is that ventilation of the newborn’s lungs is the most important part of resuscitation (1). While most newborns do not require any assistance at all in starting effective breathing at birth, approximately 10% will need some help in making the transition from intrauterine to extrauterine life, but less than 1% require extensive resuscitation (1). However, according to the World Health Organization, birth asphyxia accounts for nearly 20% of neonatal deaths worldwide (2). Interventions should be aimed at correcting problems with airway patency and the adequacy of breathing and circulation. Although the Apgar score is a useful measure of the newborn’s condition and the effects of resuscitation, resuscitation efforts should begin prior to the usual 1-minute interval when the first Apgar score is assigned (Table 34.2). In the normal process of transition to extrauterine life, the newborn’s first vigorous breath expands the lungs, forces fluid from the alveoli, and brings oxygen into the lungs. The presence of oxygen helps initiate the process of decreasing the pulmonary artery resistance that has been present throughout gestation and also begins the process of closure of the patent ductus arteriosus (PDA). With constriction and subsequent clamping of the umbilical vessels, flow to the low-resistance placental circuit is stopped, and thus the systemic vascular resistance is greatly increased, discontinuing or reversing the flow through the PDA (3). In many cases, the need for resuscitation can be predicted prior to the birth (Table 34.3).
TABLE 34.3 Factors associated with birth of a depressed newborn
Maternal conditions
Diabetes
Hypertension
Infection
Substance abuse
Significant cardiac, renal, pulmonary disease
Factors related to the pregnancy
Polyhydramnios
Oligohydramnios
Premature rupture of membranes (PROM)
Multiple gestation
Chorioamnionitis
Nonreassuring fetal heart rate tracing
Placenta previa
Placental abruption
Breech presentation
Meconium-stained amniotic fluid
CHANGES AND CONTROVERSIES IN NEWBORN RESUSCITATION
1. All meconium-stained infants do not require intubation and suctioning of the trachea. Meconium-stained infants with vigorous respiratory efforts and good muscle tone should have their mouths and pharynx suctioned while they are being dried, warmed, and observed (4–6).
2. Positive pressure ventilation, if needed, should be started with 100% oxygen and the FIO2 adjusted based on the pre-ductal SpO2. There is some evidence that effective positive pressure ventilation with 21% oxygen is as effective as with 100% oxygen. If 21% oxygen is used and improvement is not seen within 60 seconds, the FIO2 should be changed to 1.0 (7).
CLINICAL PEARL Newborns born through meconium-stained amniotic fluid who have strong respiratory effort and muscle tone should have their mouths and nose suctioned but not the trachea.
NEWBORN RESUSCITATION
The majority of term newborns born through clear amniotic fluid need not be separated from their mothers as they receive care. They should be dried quickly and either placed directly on their mothers’ skin for warmth or wrapped in dry warm blankets. Simply wiping their face and mouth should clear the airway sufficiently. Newborns born at term through meconium-stained amniotic fluid may require more than the minimal interventions indicated for the term infant born through clear amniotic fluid. Formerly, the recommendations were that all newborns born through meconium-stained amniotic fluid should be intubated and the trachea suctioned. Currently, newborns born through meconium-stained amniotic fluid demonstrating strong respiratory efforts and good muscle tone should only have their mouth and nose suctioned. For nonvigorous infants born through meconium-stained amniotic fluid, intubation and suctioning of the trachea continues to be recommended. A soft plastic suction catheter should be used to clear the pharynx prior to laryngoscopy and intubation. Tracheal suctioning should be repeated if the initial procedure yields meconium. Following the completion of tracheal suctioning, the infant’s mouth and nose should be cleared, tactile stimulation continued, and supplemental oxygen administered. When suctioning the pharynx of a newborn, care must be taken not to suction too vigorously since pharyngeal stimulation may cause a vagal reflex resulting in severe bradycardia and/or apnea. Heart rate assessment can be done using a stethoscope, palpating the pulse at a peripheral artery or, more effectively, at the umbilicus. Clearing the mouth can be done using a bulb syringe. In order to stimulate more vigorous respiratory efforts in a limp newborn, slapping or flicking the foot and rubbing the back are appropriate maneuvers.
Infants generally have primary apnea following a period of tachypnea. Stimulation as described above will stimulate breathing. Infants who go on to have irregular breathing and then secondary apnea will not respond with improved respiratory efforts, even with very vigorous stimulation. These infants often have bradycardia, with heart rates <100 per minute. Newborns who have secondary apnea or continued gasping respirations need positive pressure ventilation. Positive pressure ventilation can be accomplished with a variety of devices and it is important to be familiar with those in use (8). A Jackson-Rees circuit with a balloon-like bag that inflates with fresh gas flow can deliver supplemental oxygen if wall oxygen is flowing and the facemask is held near the newborn’s face. These devices also can deliver continuous positive airway pressure (CPAP) to a spontaneously breathing newborn. Self-inflating bags have the advantage that positive pressure ventilation can be accomplished without a source of compressed fresh gas but CPAP cannot be administered. If the self-inflating bag is squeezed, gas will be delivered to the patients and gas entrained as the bag assumes its shape. If wall oxygen is supplied to the bag, a higher FIO2 can be administered but an FIO2 approaching 1.0 cannot be given without an oxygen reservoir connected to the distal end of the bag. During administration of positive pressure ventilation, heat conservation is important. The oxygen flow meter need not be set higher than 5 L per minute. Higher flows of the cold, dry gas from the wall source can exacerbate the loss of heat in the newborn receiving positive pressure ventilation.
As in all cases of positive pressure ventilation, it is important to have an excellent mask fit, watch carefully for adequate chest rise, and minimize inflation of the stomach. In newborn resuscitation, the breaths should be adequate to inflate the lungs and the respiratory rate should be 40 to 50 per minute. The delivery room equipment will include properly sized masks for use in the newborn. Cushioned masks are preferred because these masks allow a snug fit without excessive pressure on the infant’s face. Prior to institution of positive pressure ventilation, the infant’s airway must be clear of debris, secretions, and/or meconium. In addition, care must be taken to avoid excessive positive pressure. The pop-off valve included with the self-inflating bag should be adjusted to minimize excessive pressure. The flow control valve on the self-inflating bag, if adjusted improperly, can deliver excessive end-expiratory pressure and overinflate the infant’s lungs. Each of these devices can be equipped with a manometer, allowing the operator to see the pressure delivered during the resuscitation. If positive pressure ventilation seems only poorly effective, adjuncts may be needed. An oropharyngeal airway of the correct size may open the airway and allow more effective ventilation of the lungs. Also, if the stomach has been distended with gas from the efforts at ventilation, placement of an orogastric tube may decompress that organ and, again, allow more effective ventilation of the lungs. Effective positive pressure ventilation of the lungs with 100% oxygen should produce rapid and dramatic improvement in the infant’s condition. The color should become pink, at least centrally (acrocyanosis may not improve for hours, even in normal newborns), and the heart rate should increase to >100 per minute. If rapid improvement is not noted, a quick assessment of the infant’s airway patency, proper functioning of the equipment used to provide positive pressure, the adequacy of the oxygen supply, and adequacy of the mask fit should be undertaken. If, after 60 to 90 seconds of positive pressure efforts, ventilation is ineffective in improving the infant’s condition, endotracheal intubation should be accomplished. (see the following section).
Persistent central cyanosis is not normal and indicates systemic hypoxemia. Well newborns can have acrocyanosis and not have systemic hypoxemia. Peripheral cyanosis (acrocyanosis) is seen when 5 g of hemoglobin are deoxygenated, which occurs with some regularity in normal newborns as a result of their high hemoglobin level. If a short period of positive pressure ventilation results in improved color, if pulse oximetry (if available and in use) is reassuring, and the infant exhibits regular respiratory efforts, ventilation can be discontinued and the infant carefully observed. Any newborn who requires positive pressure ventilation and responds with vigorous respiratory efforts, a heart rate >100 per minute and good muscle tone should not be considered a normal newborn. This infant should be monitored in a higher-acuity environment than the routine newborn nursery. If the resuscitation occurs in a community hospital setting, this may require transfer to a facility with a level II nursery.
The longer the resuscitation, the greater the chance that postresuscitation complications may occur. The newborn may develop seizures, disordered breathing, or apnea. If the newborn was born through meconium-stained amniotic fluid, s/he is at risk for development of the meconium aspiration syndrome with respiratory distress, hypoxemia, hypercarbia, and pulmonary artery hypertension. Following resuscitation, infants are also at risk for development of myocardial dysfunction, acute tubular necrosis, and/or necrotizing enterocolitis (1).
Chest compressions should begin within 30 seconds of the institution of positive pressure ventilation if the heart rate does not increase to >60 per minute. The infant’s heart rate can be assessed either by palpating the pulse of the umbilical cord remnant or with a neonatal stethoscope. With the use of the stethoscope, the adequacy of mask ventilation can also be assessed. A low heart rate is suggestive of poor myocardial oxygen supply secondary to systemic hypoxemia, possible hypotension, and probably systemic acidosis. In this situation, it is unlikely that cardiac output will improve spontaneously. Chest compressions are ineffective unless the lungs are being ventilated with oxygen, so it is important to assure that mask ventilation is effective. This is a two-person effort. The person providing positive pressure ventilation stands at the head of the newborn while the person performing the chest compressions (cardiac massage) stands to the side or at the foot of the patient (At this point, endotracheal intubation should be considered, which will be reviewed below).
Chest compressions in the newborn require a different technique than that used in older children and adults. Two different techniques are used to perform cardiac massage in infants and newborns (9,10). The two thumbs can be used to compress the sternum while the fingers support the spine and the hands encircle the infant’s torso. Alternatively, the tips of the middle and index finger of one hand compress the sternum while the other hand supports the baby’s back. If the infant is on a firm surface, support of the back may not be needed. In either technique, the point of compression is in the sternum just below the nipple line. In either technique, the pressure must be exerted vertically only on the sternum, not laterally on the ribs. The depth of compression should be approximately one third of the distance between the sternum and spine prior to starting the compressions. As with cardiac massage in older children and adults, the heart must be allowed to fully refill once the compression is completed. Pressure must be completely released between compressions. The fingers or thumbs used for compressions should nevertheless remain in contact with the sternum during release of the compression; otherwise, the precise location needed for the fingers or thumbs may be lost between compressions and time will be wasted relocating the spot. If the fingers or thumbs are kept in contact with the sternum throughout the cardiac massage cycle, it will be easier to keep a consistent depth of compression. The time spent during the downward part of the compression should be slightly shorter than the time for “diastole,” when the heart is filling.
There are some risks associated with cardiac massage in infants. If pressure is applied to the xiphoid process, liver laceration is possible and if excessive pressure is applied even to the correct location, fracture of a rib or ribs is possible. The cardiac massage and ventilation should be coordinated in a 3:1 ratio. The team performing the resuscitation should administer 30 breaths and 90 compressions each minute. During cardiac massage, the breathing rate is decreased from the rate of 40 to 50 used when only positive pressure ventilation was being administered. In the situation when cardiac massage and positive pressure ventilation are being coordinated, the person performing compressions counts aloud and the person performing ventilation inserts the breath into the compressions so that one breath is given for three compressions. The breath should be administered during the release of the compression and exhalation occurs during the compression itself. If the spontaneous heart rate increases to >100 per minute, cardiac massage can be stopped. Positive pressure ventilation should be continued unless the infant also exhibits regular vigorous respiratory efforts. In this case, postresuscitation care as described above should be arranged. This infant must not be considered a routine normal newborn and must not be cared for in the regular nursery.
Endotracheal intubation can be part of the resuscitation effort at a number of points in the resuscitation. For a limp infant born through meconium-stained amniotic fluid, intubation is indicated in order to suction any aspirated meconium from the trachea. If the infant remains limp and meconium is no longer suctioned from the trachea, reintubation for the purpose of positive pressure ventilation may be indicated. If positive pressure ventilation with a facemask and bag is ineffective as judged by breath sounds, chest movement, and lack of clinical improvement, intubation is indicated. If, despite adequate positive pressure ventilation, cardiac massage is begun for a persistent heart rate <60 per minute, intubation of the trachea may be indicated in order to make coordination of chest compressions and ventilation easier. If cardiac massage and adequate bag/facemask positive pressure ventilation are ineffective in increasing the heart rate to 60 per minute and administration of epinephrine is indicated, intubation may be indicated to provide a route for administration. Prior to laryngoscopy, be sure all equipment is functioning properly and a selection of appropriately-sized endotracheal tubes are available; suction must be available as well. If the endotracheal tubes are too long for use in term and preterm newborns, prior to intubation the tube may be shortened to 15 cm in order to decrease dead space. Be sure the 15-mm endotracheal tube connector is replaced securely once the tube has been cut to the 15-cm length. A stylet is helpful in cases when visualization is suboptimal or a nonstyletted tube is difficult to direct to the larynx. Assure that the stylet does not protrude from the end of the tube or from the Murphy eye and that the stylet fits loosely enough so that it can be easily removed once the trachea is intubated. Intubation of a depressed newborn who is not doing well during resuscitation must be done as quickly as possible by an experienced, accomplished individual. As preparations for intubation are underway, mask ventilation (and cardiac massage if it is being done) must continue without interruption. The same attention to medication and equipment readiness must be given in this circumstance as is given prior to laryngoscopy and intubation in the OR. Assuring proper positioning of the endotracheal tube is difficult in any newborn and particularly so during resuscitation. Breath sounds are easily transmitted, and heard all over the precordium and over the abdomen even in newborns who have been improperly intubated. Clinical signs of an esophageal intubation include: continued cyanosis and bradycardia, absent breath sounds, poor chest movement, gastric distention, and no color change in the CO2 detector. Signs of proper positioning include improvement in the infant’s color, equal breaths sounds over the left and right chest, increase in the heart rate, and color change in the colorimetric detector. Once the infant has stabilized, a chest X-ray (CXR) should be done to confirm proper placement. The use of a colorimetric CO2 detector in this circumstance can be very helpful (11). Even with this monitor, however, this can be misleading. In cases of low cardiac output such as during resuscitation, the pulmonary blood flow may be decreased to the point that there may be insufficient CO2 delivered to the lungs to change the color of the detector. If the pulse is weak or absent or the blood pressure (BP) very low, reliance on the colorimetric detector to confirm tracheal position of the endotracheal tube may lead to the incorrect conclusion that esophageal intubation has occurred (12,13).
Even with successful placement of the endotracheal tube in the trachea, morbidity is possible. The tube can easily be advanced too far, resulting in an endobronchial intubation. In a term newborn, there are only 4 cm between the vocal cords and the carina, so proper positioning of the tube is not a trivial matter. If the length marker indicates 9 or 10 cm. at the upper lip, the endotracheal tube tip should be in the mid-trachea. In cases of failed intubation or when infants appear to have a difficult airway, the use of a laryngeal mask airway (LMA) should be considered. Size 1 LMAs have been successfully used in term newborns. High ventilating pressures cannot be administered through an LMA. However, if mask ventilation is poor or ineffective and intubation cannot be accomplished, the use of an LMA can be lifesaving (14,15).
Nearly all infants who require resuscitation will respond to effective positive pressure ventilation and effective cardiac massage. However, for the small number of newborns who continue with a heart rate <60 per minute and no clinical improvement despite correct endotracheal tube placement in the mid-trachea, positive pressure ventilation with 100% oxygen and effective cardiac massage, administration of resuscitation medications and/or fluids is indicated. Epinephrine and volume expansion are indicated for these newborns. Naloxone can be considered in infants whose mothers have recently received opioids. Sodium bicarbonate can also be administered to infants when there is likely the presence of metabolic acidosis. This hypertonic medication must be given very slowly, over at least 2 minutes, in order to avoid the risk for development of an intraventricular hemorrhage. The recommended dose of sodium bicarbonate is 2 mEq per kg, using the usual 4.2% concentration that contains 0.5 mEq per mL solution yielding a volume of 4 mL per kg IV administered over at least 2 minutes. In infants who have required resuscitation to the point of administration of medication and volume, intravenous access must be obtained. A peripheral IV should be started or, as an alternative, catheterization of the umbilical vessels should be accomplished. Only individuals with expertise and experience in catheterizing umbilical vessels should attempt this procedure. Administration of medication through a catheter placed in the umbilical vein can cause hepatic necrosis and improperly placed umbilical artery catheters can affect renal, mesenteric, or ductal blood flow with serious consequences.
Epinephrine can be administered into an endotracheal tube, peripheral vein, or properly placed (through the liver) umbilical vein. The recommended solution for use in resuscitation of the newborn is 1:10,000. This medication has a concentration of 100 µg per mL. The dose administered is 0.1 to 0.3 mL per kg rapid IV push followed by a flush of 0.5 per 1.0 mL. Higher doses had been recommended but these higher IV doses have not been effective (16). When the epinephrine is given via the endotracheal tube, the dose is 0.3 to 1.0 mL per kg. Once the dose is given via the endotracheal tube, the dose should be followed by several positive pressure breaths in order to assure that the dose gets to the tracheal mucosa for absorption. Absorption of epinephrine into the systemic circulation is not completely reliable, however (16). If there is not a brisk response to the epinephrine, IV administration of epinephrine is recommended. If, after IV epinephrine administration there is not a vigorous cardiovascular response, volume expansion should be begun. 10 to 20 mL per kg of 0.9% normal saline or Ringer lactate should be given IV in this situation (17) (Table 34.4).
TABLE 34.4 Newborn resuscitation medications (1)
Medication | Dose | Notes |
Epinephrine IV | 1:10,000, 0.1–0.3 mL/kg | Flush IV can repeat q5min |
Epinephrine ETT | 1:10,000, 0.3–1 mL/kg | Positive pressure breaths |
IV volume | 10–20 mL/kg | 0.9% NS, LR, 5% albumin |
Naloxone | 1 µg/kg IV | Maternal opioids |
NaHCO3 | 2 mEq/kg IV | Slowly |
CLINICAL PEARL Although epinephrine can be given through the endotracheal tube as well as intravenously, serum levels after endotracheal administration are not reliable and the IV route is greatly preferred.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree