Key Clinical Questions
Introduction
In the United States, a driver’s license assumes competency to drive a car despite absence of proof that competency exists and despite statistics that as many as 50,000 Americans die and many more are disabled from car accidents annually. The same is true for obtaining a license to own a gun. When patients agree with recommendations of their physicians, the issue of competency is rarely raised despite the absence of competency. It is when patients and physicians disagree—when patients make decisions that clinicians feel are detrimental to their well being—that issues of competency are raised. The issue of competency is complex. Many medical decisions are affected by personal issues, religious and spiritual beliefs, or social pressures.
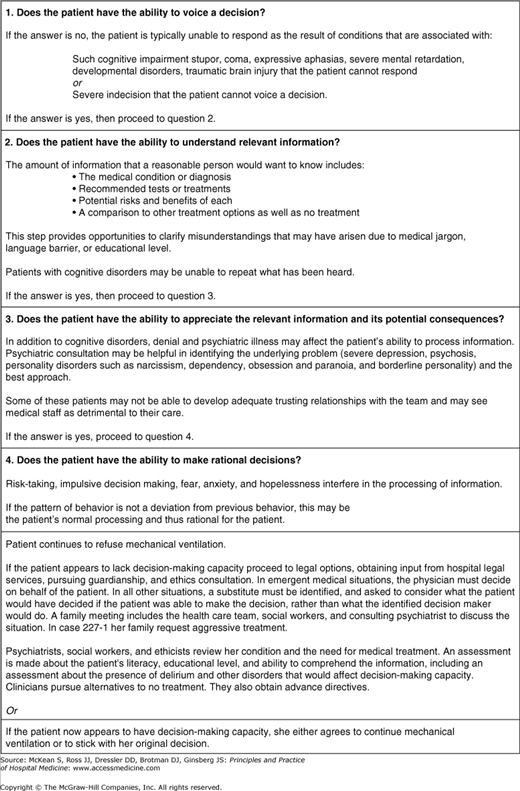
Competency is primarily a legal term rather than a medical one. Informed consent implies that patients have certain rights and expectations when it comes to making decisions regarding their own medical care. Patients have the right to be informed, their decision making should be voluntary, and they must be competent to make adequate decisions. In the hospital setting, the most common question posed to consultation liaison psychiatrists relates to decision-making capacity. Psychiatrists may help in the assessment of a patient’s cognitive and emotional ability to make a decision. The hospital’s ethics committee may help resolve the primary issue affecting the patient, especially if it is more a moral decision involving life and death decision making rather than a clinical one. The patient’s spiritual advisor or hospital chaplain may be invaluable in sorting out the relevant issues and promoting resolution of conflict when decisions are made that make the medical providers uncomfortable (Figure 227-1).
MECHANICAL VENTILATION Three weeks ago a 68-year-old woman sustained a cervical spinal cord injury from a fall. Quadriplegic, she will likely die if artificial ventilation is discontinued. The patient stated that “my life as it is now is not worth living. I am not happy.” The patient seems to understand the implications of discontinuing artificial ventilation. The patient’s family wants her to continue mechanical ventilation and they are concerned about the patient’s thought process. Is this patient competent to make such a decision? Is this patient competent to make medical decisions relating to her care? |
This patient wants to discontinue mechanical ventilation. Does this patient truly understand the choice she is making? Is this patient depressed? Could this patient’s mental state impact her decision to stop mechanical ventilation? Does this patient have the right to refuse to continue mechanical ventilation? The first question to ask is whether this patient has the decision-making capacity to choose whether to continue with mechanical ventilation.
Competency is defined as the minimal mental, cognitive, or behavioral ability, trait, or capability that is required for a person to perform a particular legally recognized act or to assume a legal role. Only a judge can determine the competency of an individual. A legal concept, this determination relates to a specific situation, meaning a person may be competent to perform one act but may not be competent to perform another. Applelbaum and Grisso articulate four legal standards for the determination of competency:
The communication of choice
Understanding relevant information as it applies to that choice
Appreciating the situation and its consequences
Rational decision-making.
|
In a clinical situation, the judge will factor in the clinician’s assessment of a patient’s decision-making capacity in his determination of competency.
In the hospital setting, all patients are assumed to be competent and on admission sign a general statement consenting to treatment. A patient may be competent to identify a health care proxy but not competent to decide whether to proceed with mechanical ventilation. In the hospital, the determination of decision-making capacity can be made by any licensed physician and does not require the evaluation of a psychologist or psychiatrist even though one is often consulted to make that determination. The determination of decision-making capacity (like competency) is task specific, meaning a specific determination cannot be generalized to other decisions being made. Similar to the concept of competency, decision-making capacity utilizes four standards:
An understanding of the information provided
Communication of choice
An appreciation of available options
Rational decision-making.
|
This refers to patients being able to express a basic understanding of their medical illness, the reasons for hospitalization, and the treatment options, including noting the risk and benefits of the options presented to them. In the case example, the patient should be able to explain her situation, ie, that she is in the hospital on mechanical ventilation due to paralysis. She should be able to explain that she has one of two options, either to continue on mechanical ventilation or to stop mechanical ventilation. Her physicians need to assess her awareness of the benefits and risks of mechanical ventilation and the risks and benefits associated with termination of mechanical ventilation.
The patient should be able to express a preference or decision about a specific treatment. Indecisiveness may be a clue that a patient lacks decision-making capacity.
In the case example, the patient has clearly expressed her wishes that mechanical ventilation should be discontinued.
Does the patient have the ability to truly understand how her decisions regarding treatment apply to her? It is more than just a factual understanding of the risks and benefits of a treatment decision, but rather an understanding of how that treatment decision results in consequences that directly affect future outcomes. In the case example, can the patient truly appreciate that her decision to discontinue mechanical ventilation will most likely result in her death?
This refers to the decision process behind the communication of choice being made. Does the patient have a good explanation for why she is making her decision? If such a thought process is appropriate, then such a decision may be rational even if the clinician totally disagrees with the decision being made. If our patient is able to explain rationally why she wishes to discontinue mechanical ventilation, then the decision may be appropriate even if it results in her death.
A patient must be able to satisfy all four of these standards to have decision-making capacity. How to evaluate a patient for decision-making capacity utilizing these standards depends on the patient’s illness, the treatment that is in question, and the consequences of the decision being made with respect to treatment.
In 1977, Roth proposed a sliding scale approach to the determination of decision-making capacity and therefore competency. The determination of decision-making capacity would vary according to risk-benefit ratio. In the case example, the level of determination of decision-making capacity would be high because the patient has made the decision that she no longer wants to continue with mechanical ventilation, and the discontinuation of ventilation places the patient at high risk of harm and likely death. However, if the patient was in agreement for continued mechanical ventilation, then the threshold for determining decision-making capacity would be very low because not only is she in agreement with her physicians, but the risk to the patient would be much lower than if she were to stop mechanical ventilation.
Bostwick, and colleagues suggested utilizing a three-dimensional model for determining decision-making capacity. The model looks at the benefits of the proposed treatment (high versus low); the risk of the proposed treatment (high versus low); and the patient’s decision to either accept or refuse treatment. This model allows the clinician to make a quick assessment of whether or not the threshold for determining decision-making capacity will be high or low. Any physician, regardless of specialty, can make a general assessment of decision-making capacity when appropriate. This chapter will address three factors:
The circumstances under which the question of decision-making capacity should be asked
How to assess decision-making capacity
Indications for psychiatric consultation to assess decision-making capacity.
The patient’s refusal of treatment is the most common reason to assess decision-making capacity of a patient. In addition, it is appropriate to assess a patient’s decision-making capacity to ensure informed consent or capacity to make a decision to leave against medical advice.
There are five basic questions that the primary team can ask of the patient when assessing decision-making capacity.
Will you explain the treatment we recommend?
What is your understanding of how this treatment can help you?
What is your understanding of what could happen if you do not receive this treatment?
What alternatives would you choose instead to address the problem?
Why have you decided to accept or refuse the treatment suggested?
These basic questions allow the clinician to cover the four standards of assessment of decision-making capacity (understanding the illness, communication of choice, appreciation of their choice, and rational decision making).
The hallmark of a good physician is to ask for help when there is uncertainty about a patient’s decision-making capacity. Asking for a psychiatrist’s opinion may be most helpful in the following situations:
A patient’s psychiatric history raises questions about competency
Cognitive impairment such as delirium may jeopardize decision-making capacity

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree