CHAPTER 107
De Quervain Paratenonitis
(Thumb Tenosynovitis)
Presentation
The patient, usually a middle-aged woman, experiences an insidious onset of difficulty with tasks such as opening jars because of pain localized to the dorsoradial aspect of the wrist that is exacerbated with thumb and wrist motion, and which may also be present on awakening. Mothers of infants aged 6 to 12 months and daycare workers are frequently affected because of repetitive lifting of infants. De Quervain disease is also common in racquet sports, fishing, and golf.
On examination, the first dorsal compartment over the radial styloid is thickened and tender to palpation. Crepitus of the tendon may be felt on active and passive thumb motion. Tenderness will be elicited on palpating or stretching the extensor pollicis brevis and abductor pollicis longus tendons bordering the palmar side or, less commonly, the extensor pollicis longus tendon bordering the dorsal side of the anatomic snuff box (Figure 107-1).

Figure 107-1 First dorsal wrist compartment and the extensors of the thumb.
What To Do:
 Obtain a careful history to reveal the underlying causative activity as well as to inquire into the patient’s general health. An alternate source of this paratendinopathy may be uncovered, such as gonococcal tenosynovitis or fluoroquinolone-induced tendinopathy.
Obtain a careful history to reveal the underlying causative activity as well as to inquire into the patient’s general health. An alternate source of this paratendinopathy may be uncovered, such as gonococcal tenosynovitis or fluoroquinolone-induced tendinopathy.
 Perform a physical examination to determine the exact source of pain and tenderness.
Perform a physical examination to determine the exact source of pain and tenderness.
 Document normal circulation and sensation. Compress the thumb metacarpal onto the scaphoid (axial loading of the carpometacarpal joint) to rule out arthritis at the joint with a painless maneuver.
Document normal circulation and sensation. Compress the thumb metacarpal onto the scaphoid (axial loading of the carpometacarpal joint) to rule out arthritis at the joint with a painless maneuver.
 Have the patient fold the thumb into the palm, close the fingers over it into a fist, then passively ulnar deviate the wrist. This is known as the Finkelstein test (Figure 107-2) and reproduces the pain of de Quervain tenosynovitis of the extensor pollicis brevis and abductor pollicis longus tendons. A positive test causes sharp pain over the first dorsal compartment.
Have the patient fold the thumb into the palm, close the fingers over it into a fist, then passively ulnar deviate the wrist. This is known as the Finkelstein test (Figure 107-2) and reproduces the pain of de Quervain tenosynovitis of the extensor pollicis brevis and abductor pollicis longus tendons. A positive test causes sharp pain over the first dorsal compartment.

Figure 107-2 Demonstration of the Finkelstein test. (Adapted from Parmelee-Peters K, Eathorne SW: The wrist: common injuries and management. Prim Care 32:35-70, 2005.)
 Acute de Quervain paratenonitis responds best to corticosteroid injection into the tendon sheath (Figure 107-3). Results of a recent meta-analysis of treatments for de Quervain tenosynovitis showed that there was an 83% cure rate with injection alone. This rate was much higher than any other therapeutic modality (61% for injection and splint, 14% for splint alone, and 0% for rest or nonsteroidal anti-inflammatory drugs [NSAIDs]). Tendon-sheath injection is a technique that can be used by the more experienced clinician. Using a 27-gauge, ½- to 1-inch needle, slowly penetrate the skin and soft tissue, aiming for the middle of the tendon. When the tendon is hit, it may produce a muscle reflex, increased resistance to advancement of the needle, and pain, which are signals to withdraw the needle slightly. Move the muscle-tendon unit so it slides back and forth, and readvance the needle until the tendon is felt slightly scraping the point. Back off 1 mm, steady the syringe and needle, and inject 1 mL of betamethasone (Celestone) or 20 mg of triamcinolone (Aristocort) along with 2 mL of bupivacaine (Marcaine) 0.5%. While injecting, palpate the tendon, feeling for a “sausaging” effect as the mixture inflates the sheath. Warn the patient that there may be a transient flare in pain when the anesthetic wears off, which may last 24 to 48 hours. The corticosteroid should begin to have a noticeable therapeutic effect within a few days.
Acute de Quervain paratenonitis responds best to corticosteroid injection into the tendon sheath (Figure 107-3). Results of a recent meta-analysis of treatments for de Quervain tenosynovitis showed that there was an 83% cure rate with injection alone. This rate was much higher than any other therapeutic modality (61% for injection and splint, 14% for splint alone, and 0% for rest or nonsteroidal anti-inflammatory drugs [NSAIDs]). Tendon-sheath injection is a technique that can be used by the more experienced clinician. Using a 27-gauge, ½- to 1-inch needle, slowly penetrate the skin and soft tissue, aiming for the middle of the tendon. When the tendon is hit, it may produce a muscle reflex, increased resistance to advancement of the needle, and pain, which are signals to withdraw the needle slightly. Move the muscle-tendon unit so it slides back and forth, and readvance the needle until the tendon is felt slightly scraping the point. Back off 1 mm, steady the syringe and needle, and inject 1 mL of betamethasone (Celestone) or 20 mg of triamcinolone (Aristocort) along with 2 mL of bupivacaine (Marcaine) 0.5%. While injecting, palpate the tendon, feeling for a “sausaging” effect as the mixture inflates the sheath. Warn the patient that there may be a transient flare in pain when the anesthetic wears off, which may last 24 to 48 hours. The corticosteroid should begin to have a noticeable therapeutic effect within a few days.
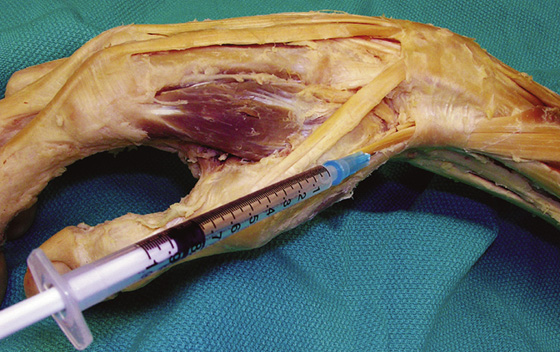
Figure 107-3 Inject site for de Quervain tenosynovitis. (Adapted from Parmelee-Peters K, Eathorne SW: The wrist: common injuries and management. Prim Care 32:35-70, 2005.)
What Not To Do:
 Do not allow NSAIDs to be used. They have been shown to be of no value in this condition and have potentially hazardous side effects.
Do not allow NSAIDs to be used. They have been shown to be of no value in this condition and have potentially hazardous side effects.
 Do not inject directly into the tendon. This may weaken the tendon and lead to future rupture.
Do not inject directly into the tendon. This may weaken the tendon and lead to future rupture.
 Do not inject steroids into the very superficial layer of the subcutaneous tissue. This may cause skin depigmentation, which is particularly noticeable in dark-skinned individuals.
Do not inject steroids into the very superficial layer of the subcutaneous tissue. This may cause skin depigmentation, which is particularly noticeable in dark-skinned individuals.
 Do not splint the wrist and thumb after steroid injection. This reduces the cure rate over injection alone.
Do not splint the wrist and thumb after steroid injection. This reduces the cure rate over injection alone.
Discussion
Symptoms of de Quervain syndrome are related to overuse. The involved tendons course under the extensor retinaculum in a groove along the radial styloid process. Repetitive wrist motion causes shear stress on the tendons in their small compartment, which results in inflammation of the tenosynovium. This is more accurately called paratenonitis. The term includes what was previously called peritendinitis, tenosynovitis (single layer of areolar tissue covering the tendon), and tenovaginitis (double-layer tendon sheath). Clinically, paratenonitis presents with acute edema and hyperemia of the paratenon with infiltration of inflammatory cells. After a few hours to a few days, a fibrinous exudate fills the tendon sheath and causes the crepitus that can be felt on clinical examination.
This condition is often seen in supermarket cashiers and piecework factory workers and after intensive computer keyboarding. De Quervain disease is approximately 6 times more common in women than in men. It is important to have the patient avoid the activity that brought on the condition.
Tendon sheath injections are well tolerated and can be repeated safely at least three times, spaced several months apart. Most often, one injection is effective. One small study suggested that postpartum women with de Quervain disease respond well to conservative management without steroid injection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


