Objectives/indications
The applications of ultrasound for procedural assistance and guidance are rapidly evolving. One of the basic principles of pediatric emergency and critical care medicine is to establish and maintain the airway during resuscitation. When intubation is indicated, point-of-care ultrasound provides a rapid, direct, and real-time method for confirming proper endotracheal tube (ETT) placement within the trachea. In situations where direct visualization of the ETT passing through the vocal cords is not possible, ultrasound may provide advantages over traditional secondary means of confirming ETT placement.
In situations of chest trauma, thoracostomy tubes, or chest tubes, are often indicated as an adjunct to airway management. Traditional methods of confirming proper placement include radiographs and CT scan. More recently, it has been suggested that ultrasound may be a useful means by which the correct placement of intrathoracic thoracostomy tubes may be confirmed.
The objectives of this chapter are to describe how point-of-care ultrasound may be utilized to evaluate proper endotracheal tube placement within the larynx and trachea, and proper thoracostomy tube positioning within the thoracic cavity. While these are novel applications, the suggested techniques for performing these applications are reviewed. Further research needs to be performed in order to validate these applications.
Endotracheal tube placement
Background
Endotracheal tube (ETT) placement is often indicated in order to establish and stabilize an airway during resuscitations. Traditional methods by which a clinician may confirm proper ETT placement include auscultation, capnography, and chest radiography.
Recently, ultrasound was also introduced to serve as an adjunct to traditional methods of ETT confirmation. Since ultrasound of the airway is an emerging indication for point-of-care sonography, there are relatively few studies on using ultrasound for ETT confirmation. Thus far, when compared to the traditional methods of auscultation and capnography, airway ultrasound is more sensitive in detecting esophageal intubation. In addition, ultrasound is more rapid when compared to conventional chest radiography. Prior literature focuses on the indirect signs of proper endotracheal tube placement, which include the evaluation of bilateral lung expansion following intubation (see Chapter 6).
Several small studies evaluating ultrasound’s ability to determine correct ETT placement have been performed in the controlled environments of intensive care units and operating rooms. In both pediatric and adult patients, sonography has been shown to be both 100% sensitive and specific in confirming the intratracheal position of the ETT. Research in the uncontrolled environment of the adult emergency department has shown that bedside sonography may be highly accurate in determining endotracheal versus esophageal intubation. Further studies need to be performed in pediatric patients in the emergency department.
Anatomy
Key structures of the larynx and hypopharynx are important to be familiar with. Most important is the relationship between the trachea, esophagus, and external anatomic landmarks (Figure 22.1).
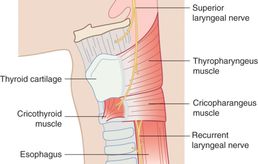
Figure 22.1 Anatomy of the larynx. External landmarks. It is important to recognize the location of the trachea in relation to the esophagus. Artwork created by Emily Evans © Cambridge University Press.
Technique
Transducer selection and orientation
The superficial location of the upper airway structures makes ultrasound visualization with a high-frequency (5–10 MHz), linear transducer ideal. The indicator should be oriented towards the patient’s right side.
Patient position and preparation
Proper patient positioning is the key to a successful intubation and should be at the discretion of the individual performing the intubation. Frequently, the sonographer is positioned at the right-hand side of the patient, holding the transducer over the anterior neck of the patient (Figure 22.2a).
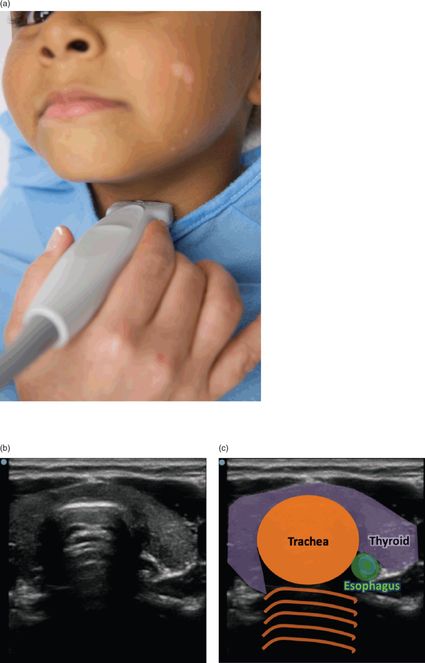
Figure 22.2 Sonography of the airway. (a) Transducer position for localizing the lower cervical trachea and esophagus. The transducer is positioned at the height of C6 or the isthmus of the thyroid gland. If the transducer is moved more cephalad, the sonographer can also attempt to provide cricoid pressure with the transducer. (b) Ultrasound image of the lower neck anatomy. (c) Illustration depicting important structures: the trachea, esophagus, and thyroid. Reprinted with permission, Beatrice Hoffmann, MD PhD.
Ultrasound imaging
The vocal cords can be located by placing the transducer midline on the anterior neck at the level of the mid-thyroid or just below the thyroid (Figure 22.2a), and scanning cephalad to the level of the thyroid cartilage. The vocal cords appear as hyperechoic, linear structures in the shape of an inverted “V,” and can be observed to open or close with respiration and phonation. In the transverse view, the trachea appears as a midline, hypoechoic structure with a brightly echogenic line immediately behind it representing air in the tracheal lumen. The tracheal rings can best be appreciated in the long-axis view. The esophagus appears as a collapsed, oval, multilayered structure immediately to the left of the trachea and posterior to the left thyroid lobe (Figure 22.2b,c). It is important to note that the position of the esophagus relative to the trachea may differ depending on the level at which it is being visualized.
Ultrasound-guided procedure
Ultrasound may be performed simultaneously during intubation, or following intubation. It may be preferred to perform real-time visualization during intubation, since the ETT is rarely visualized within the trachea following intubation. This is due to the fact that the air between the wall of the trachea and the ETT causes an acoustic impedance mismatch (Figure 22.3). Exceptions include near-drowning patients and those with significant airway secretions, where this air is replaced by fluid (Figure 22.4). In order to improve the direct visualization of the ETT, one may fill the ETT cuff with normal saline. Other secondary signs of successful intubation include normal bilateral lung sliding on lung ultrasound (see Chapter 6).

Figure 22.3 Tracheal intubation. Ultrasound image showing the trachea (arrow) and an empty esophagus (arrowhead) without visualization of the actual ETT. Reprinted with permission, Beatrice Hoffmann, MD PhD.
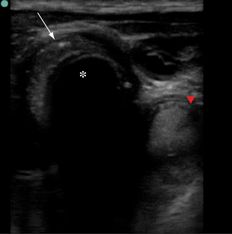
Figure 22.4 Tracheal intubation with a fluid-filled airway after drowning. Fluid-filled trachea (arrow), fluid-filled esophagus (arrowhead). The dark luman of the ETT (*) can also be visualized. Reprinted with permission, Beatrice Hoffmann, MD PhD.
In order to perform simultaneous, real-time visualization, some investigators suggest observing the region of the larynx simultaneously for a brief “widening” or distortion of the glottis as the ETT is passed. Others have shown successful sonographic detection of tracheal and esophageal intubations with positioning of the transducer close to the middle or inferior aspect of the thyroid in midline. In this location, the trachea and often the esophagus can both be identified and monitored during intubation. The sonographer can observe a brief and transient “flush” at the anterior aspect of the trachea, as the ETT is passed into the trachea, while the esophagus remains empty.
In contrast, improper ETT placement, or esophageal intubation, must be considered if distortion of the glottis and upper trachea is not noted during intubation. On ultrasound, an esophageal intubation can be recognized by the visualization of the “double trachea” sign. The esophagus that is stented open by an errant ETT which appears as curved echogenic lines with posterior acoustic shadowing located lateral to the trachea, giving the appearance of a second trachea (Figure 22.5).
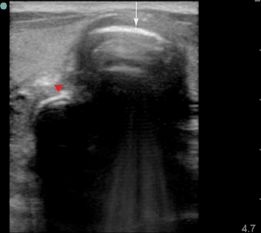
Figure 22.5 Esophageal intubation: “double trachea” sign. The stented open esophagus (arrowhead) appears similar to a second trachea (arrow). Reprinted with permission, Beatrice Hoffmann, MD PhD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








