2 Core Review Test 2
2-1. A patient with ARDS has a PaO2 of 60% on mechanical ventilation with an FiO2 of 80% and 20 cm H2O of PEEP. Physical assessment findings include patient is unresponsive to pain, respiratory rate at ventilator setting of 12/min, temperature 101.6° F (38.6° C), BP 88/64 mm Hg, HR 112/min. Urine output is 20 mL for 2 hours. Chest x-ray shows complete opacification on left lung as well as right lower and middle lobes with radiolucence in right middle lobe. Which of the following immediate interventions should the nurse now anticipate?
2-2. A patient has been in the ICU for 5 days with maximal medical management after a large left-sided (dominant) middle cerebral artery ischemic stroke. Since admission, the patient has not improved from a Glasgow Coma Scale score of three. Pupils are equally nonreactive, and the neurologist is at the bedside to evaluate the patient for brain death. Which of the following neurologic deficits would the nurse correctly interpret as supporting a determination of brain death?
2-3. A 77-year-old man is admitted for dysrhythmias and chest pain after 4 days of frequent vomiting. His workup for myocardial infarction is negative, and his nurse suspects that the patient’s clinical problems may be related to electrolyte deficiencies. Which of the following sets of clinical findings would support the nurse’s contention?
2-4. A patient is admitted to the CCU following a motor vehicle crash with a diagnosis of thoracic trauma with a flail chest. Assessment of this patient’s chest reveals “paradoxical chest wall motion,” which refers to the unstable, injured segment moving
2-5. A patient complains of chest pain, and a 12-lead ECG is performed that demonstrates sinus rhythm with ST segment depression of 2 mm and T wave inversion in leads V5 and V6. These ECG findings are consistent with
2-6. Which of the following patient descriptions suggests a late complication of renal injury?
2-7. The nurse is providing patient teaching while administering immunosuppressive therapy to an organ transplant recipient. Which of the following statements indicates that the patient has a correct understanding of their planned immunosuppressive regimen?
2-8. A 62-year-old patient recently admitted with new onset of heart failure appears distressed regarding her health condition. During the admission assessment, the nurse should determine how this patient has viewed past successes in life as well as her health and satisfaction with life because considering these issues can
2-9. During a code blue incident in an outpatient clinic, the patient was found to be hypoglycemic. Resuscitative efforts were successful after 50 mL of 50% dextrose were administered. When should the patient’s capillary glucose measurement be repeated?
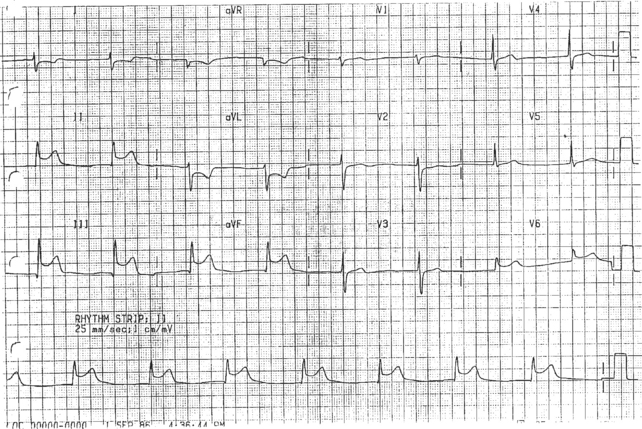
2-10. The most appropriate action for the nurse obtaining the ECG above would be to
2-11. A patient has a central venous catheter, which was placed emergently during a code. Which of the following is indicated to help reduce the incidence of a catheter-related bloodstream infection?
2-12. Recommendations for monitoring patients thought to have carbon monoxide poisoning include obtaining carboxyhemoglobin levels and ABG samples to evaluate the SaO2. In this patient population, the primary reason why pulse oximetry measurements (SpO2) are considered unreliable and inaccurate for monitoring SaO2 is because the
2-13. Treatment for pulmonary artery hypertension with a mean pulmonary artery pressure of 30 mm Hg and signs of right heart failure including tricuspid regurgitation murmur consists of administration of oxygen and
2-14. A morbidly obese patient is admitted to the unit following a laparoscopic cholecystectomy. The nurse knows that this patient is at risk for developing a hospital-associated pneumonia because
2-15. A patient is in the critical care unit following emergent right hemicolectomy for a penetrating shotgun wound. Clinical findings include pulse 145 beats/min, temperature 102° F, abdominal distention, hypoactive bowel sounds, BP had been 140/86 mm Hg but is now 108/80 mm Hg, and extremities very warm to touch with bounding pulses. The physician orders rapid fluid administration, blood cultures, and antibiotics. What clinical finding would the nurse look for in this patient as evidence of an optimal clinical response to rapid IV fluid administration?
2-16. Which of the following medications is administered to prevent sudden death associated with dilated cardiomyopathy?
2-17. A patient is admitted with pallor, shortness of breath, dyspnea on exertion, syncope, and chest pain related to right ventricular ischemia. He has a loud S2 in the pulmonic area, a right ventricular heave, and a pulmonary flow murmur. He is diagnosed with pulmonary hypertension and is to be started on treprostinil sodium (Remodulin®). Which of the following topics should the nurse be prepared to discuss with the patient regarding treprostinil administration?
2-18. A 54-year-old end-stage renal disease (ESRD) patient is admitted to the ICU after falling down three flights of stairs. The patient’s BP is 200/116 mm Hg, HR is 118/min, and RR is 32/min. The patient complains of fatigue, headache, lightheadedness, and palpitations; laboratory work reveals hemoglobin 7.6 g/dL, hematocrit 22.8%. The patient is currently receiving 3000 units of Epoetin Alfa (Epogen, Procrit) three times per week. Which of the following interventions is the most warranted at this time?
2-19. A patient who has had chest pain intermittently for 16 hours, unrelieved by aspirin and nitroglycerin, is admitted to the ICU. A 12-lead ECG shows ST segment elevation in leads II, III, and aVF. Which of the following interventions would most benefit this patient?
2-20. When the health care team plans care for a patient with sepsis, coordination of laboratory studies with fluid and pharmaceutical therapies becomes especially important. Which of the following collaborations is consistent with current recommendations for optimal management of the patient with sepsis?
2-21. A patient is admitted to the ICU after a motor vehicle collision. The patient is currently alert and oriented but had experienced a transient loss of consciousness at the scene. The only significant injury is a linear left temporal skull fracture. Within 2 hours of admission, the patient’s neurological status deteriorates. The nurse should now anticipate which of the following actions?
2-22. A teenager who has received a heart transplant was recently admitted to the Intensive Care Unit with pyelonephritis, urinary frequency, and cloudy urine, which she has experienced for a number of weeks. Which of the following should the nurse relate to effectively address the patient’s knowledge deficit and prevent delays in treatment of future infections?
2-23. Three days after surgical repair of an abdominal aortic aneurysm, a morbidly obese patient continues to be mechanically ventilated. The patient required fiberoptic intubation preoperatively. Current ventilator settings include FiO2 40%, TV 600 mL, SIMV rate 10/min. The patient over-breathes the ventilator during the day, but not at night. Daily chest x-rays show an enlarged heart and linear densities consistent with alveolar hypoventilation. Arterial blood gas values consistently demonstrate a PaO2 over 80 mm Hg and PaCO2 40 mm Hg. Which of the following should the nurse anticipate as this patient’s weaning strategy?
2-24. A postoperative patient who sustained multiple trauma from a motor vehicle crash is in the ICU. On multidisciplinary rounds, which of the following should the nurse suggest to help prevent deep vein thrombosis in this patient?
2-25. A patient with a high output enterocutaneous fistula is NPO on hyperalimentation at a rate of 80 mL/hr. The patient is listless but responds to commands appropriately. Heart rate is 124/min sinus tachycardia, BP 88/50 mm Hg. Respiratory rate is 24/min on 40% face mask with an SpO2 of 100%. Other assessment findings include 2+ edema in dependent areas and capillary refill time of 4 seconds. Admission laboratory values include hematocrit 30%, serum sodium 150 mEq/L, glucose 90 mg/dL, albumin 1.9 g/dL. The nurse anticipates immediate administration of which of the following?
2-26. A patient presents with flu-like symptoms, lymphadenopathy, a diffuse erythematous rash, and severe muscle weakness. The nurse admits the patient for close monitoring and further diagnostic workup to identify the cause of these findings. The patient suddenly loses consciousness followed by a brief period of muscle rigidity and then rhythmic muscle jerking. The best immediate course of action for the nurse is to
2-27. A patient of Chinese descent is in the ICU for aggressive fluid resuscitation. When nursing staff inform the physician that the patient appears to be experiencing hallucinations and delusional episodes and periodically is aggressive toward the staff, haloperidol (Haldol®) 2.5 mg intramuscularly is prescribed. The nurse caring for this patient should initially
2-28. Which of the following medication regimens would be most appropriate to relieve chest pain in a patient with a diagnosis of myocarditis?
2-29. A patient presents to the emergency department with acute jaundice, elevated liver enzymes, and malaise. Throughout nursing assessment of this patient, a primary concern will be to determine whether this patient manifests clinical features associated with
2-30. A patient complains of substernal pressure and becomes diaphoretic. A 12-lead ECG obtained during chest pain demonstrates tall, broad R waves and ST segment depression in leads V1-V2. These findings suggest that the nurse now needs to
2-31. A 16-year-old female admitted with diabetic ketoacidosis has a serum glucose of 250 mg/dL and is asking to use the phone to call her friends to assure them that she is all right. Since her vital signs and other clinical parameters are stable, the nurse may allow the patient to use the phone in order to respond to the patient’s needs for
2-32. A 30-weeks’-pregnant female is admitted to the ICU with heart failure owing to cardiomyopathy. The patient has a BP of 140/90 mm Hg, heart rate 116/min, sinus tachycardia, respiratory rate 28/min, labored with pulmonary rales. Anticipated treatment for this patient would include
2-33. A patient with chronic pulmonary disease is admitted to ICU with worsening dyspnea and pulmonary mechanics. The patient’s medical history includes chronic bronchitis that requires home oxygen, anxiety, and a 5-kg weight loss over the last 4 weeks. In noting these findings, the critical care nurse will plan nursing care with the understanding that in this patient population, weight loss is typically associated with
2-34. An orientee is caring for a patient 1 week post gastric bypass surgery. The patient has been unable to be weaned from mechanical ventilation. While reviewing the orientee’s care of this patient, which of the following interventions would the nurse preceptor likely suggest adding to improve this patient’s chances of survival?
2-35. During sheath removal after percutaneous coronary intervention (PCI), a patient’s heart rate decreases to 40 beats/min, BP decreases to 80/50 mm Hg, and the patient complains of nausea. Appropriate treatment for this patient would include which of the following?
2-36. A patient with a history of angina, hypercholesterolemia, and hypertension is admitted to the ICU for management of chest pain. Current medications include atenolol (Tenormin®) and hydrochlorothiazide. The patient also uses garlic pills for the hypercholesterolemia. Which of the following should be taught to the patient if invasive tests or procedures are required in the future?
2-37. Treatment of right ventricular myocardial infarction includes administration of which of the following?
2-38. During the neurologic assessment of a patient who was the driver involved in a head-on collision, the critical care nurse finds no evidence of motor function or ability to sense pain or temperature below the nipple line. These neurologic findings suggest that this patient will require nursing management for
2-39. A patient is admitted after receiving several shocks in succession from his AICD. Device interrogation reveals that the shocks were delivered appropriately. What further assessments are warranted to identify this patient’s problem?
2-40. A patient recuperating from a stroke continues to exhibit diminished level of consciousness and expressive aphasia and is being closely monitored for any difficulty coughing or swallowing. To detect the earliest clinical evidence of aspiration in this patient, which of the following should the nurse look for?
2-41. The patient was admitted with a serum glucose level of 468 mg/dL. After 2 hours of therapy with 4 units/hr of regular Humulin in normal saline via the intravenous route, the patient’s serum glucose is 400 mg/dL. Which of the following is the most appropriate nursing intervention at this time?
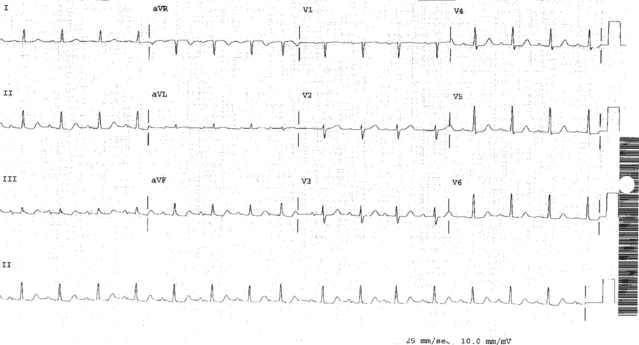
2-42. A patient complains of chest pain. The 12-lead ECG performed prior to administering 1/150 grains of nitroglycerin appears below. Serum troponin is 0.1 ng/mL. The treatment plan for this patient would include which of the following?
2-43. A nurse working the ICU night shift notes that over the past 6 months a number of patients with abdominal aortic aneurysm (AAA) repairs have experienced poor outcomes. The nurse approaches her nurse manager and asks if this trend has been noted by anyone else. The manager replies “No,” and suggests that the nurse should
2-44. Which action should the nurse anticipate for a patient with supratentorial intracerebral hemorrhage?
2-45. A patient undergoes a right posterolateral thoracotomy for repair of a membranous tracheal tear located 4 cm above the carina associated with pneumomediastinum and bilateral pneumothoraces. A few hours after the patient’s return from surgery, a bronchoscopy is performed to clear secretions. Over the next few hours, it is important that the nurse monitors the chest drainage system to ensure
2-46. A patient in the critical care unit continues to exhibit signs and symptoms of hypoperfusion related to septic shock despite receiving adequate amounts of crystalloid and colloid for fluid resuscitation, so the physican now orders initiation of vasopressor therapy. Given the following patient information, which vasopressor agent would be the best choice for this patient? HR 110/min, sinus tachycardia; BP 80/40 mm Hg; ScVO2 60%; PAP 30/16 mm Hg; PCWP 14 mm Hg; CO 10.0 L/min; CI 5.2 L/min/cm2; SVR 500 dynes/sec/cm−5.
2-47. A trauma patient will require massive transfusions of red blood cells and aggressive fluid resuscitation. Which of the following nursing interventions will prevent the greatest number of complications for this patient?
2-48. A patient with a left ventricular assist device placed as a bridge to cardiac transplant is at greatest risk for which of the following complications?
2-49. A patient is admitted to the ICU with a diagnosis of hypertensive urgency 2 weeks after roux-en-y gastric bypass surgery. The patient says, “I don’t understand how my blood pressure can still be so high. I thought that operation was going to fix my blood pressure problems.” The most appropriate nursing response is
2-50. Upon turning a postoperative coronary artery bypass patient, the nurse observes 200 mL of bloody drainage in the chest tube drainage system. The nurse should perform which of the following?
< div class='tao-gold-member'>