history that support the diagnosis of ocular allergy. Examination discloses generalized injection of the conjunctiva, with thinning out toward the cornea. (Localized inflammation suggests some other diagnosis, such as presence of a foreign body, an inverted eyelash, episcleritis, or a viral or bacterial ulcer.)
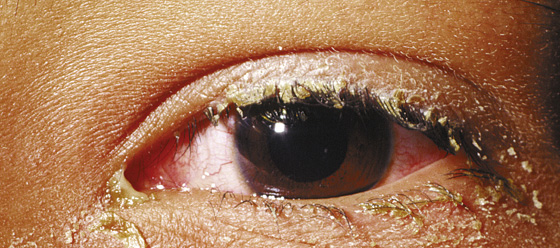
Figure 14-1 Bacterial conjunctivitis. (Adapted from Palay DH, Krachmer JH: Primary Care Ophthalmology, ed 2. St Louis, 2005, Mosby.)

Figure 14-2 Viral conjunctivitis. (Adapted from Palay DH, Krachmer JH: Primary Care Ophthalmology, ed 2. St Louis, 2005, Mosby.)
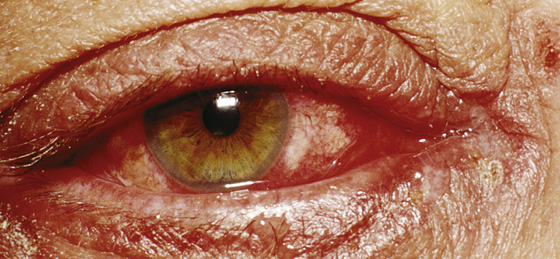
Figure 14-3 Allergic conjunctivitis. (Adapted from Palay DH, Krachmer JH: Primary Care Ophthalmology, ed 2. St Louis, 2005, Mosby.)
Vision and pupil reactions should be normal, and the cornea and anterior chamber should be clear. Any discomfort should be temporarily relieved by the instillation of topical anesthetic solution.
If few symptoms are present on awakening but discomfort worsens during the day, dry eye is probable. Eye-opening during sleep, which leads to corneal exposure and drying, results in ocular redness and irritation that is worse in the morning.
Physical and chemical conjunctivitis, caused by particles, solutions, vapors, and natural or occupational irritants that inflame the conjunctiva, should be evident from the history.
Deep pain, pain not relieved by topical anesthetic, severe pain of sudden onset, photophobia, vomiting, decreased vision, and injection that is more pronounced around the limbus (ciliary flush) suggest more serious involvement of the cornea or the globe’s internal structures (e.g., corneal ulcer, keratitis, acute angle-closure glaucoma, uveitis) and demand early or immediate ophthalmologic consultation.
What To Do:
 Instill proparacaine (Alcaine, Ophthaine, Ophthetic) anesthetic drops to allow a more comfortable examination and to help determine whether the patient’s discomfort is limited to the conjunctiva and cornea. If there is no pain relief, the pain comes from deeper eye structures.
Instill proparacaine (Alcaine, Ophthaine, Ophthetic) anesthetic drops to allow a more comfortable examination and to help determine whether the patient’s discomfort is limited to the conjunctiva and cornea. If there is no pain relief, the pain comes from deeper eye structures.
 Examine the eye, including assessment of visual acuity (correct for any refractive error and record results) and pupil reaction and symmetry, inspection for foreign bodies, estimation of intraocular pressure by palpating the globe above the tarsal plate, and examination with a slit lamp (when available), and fluorescein staining and ultraviolet or cobalt blue light to assess the corneal epithelium.
Examine the eye, including assessment of visual acuity (correct for any refractive error and record results) and pupil reaction and symmetry, inspection for foreign bodies, estimation of intraocular pressure by palpating the globe above the tarsal plate, and examination with a slit lamp (when available), and fluorescein staining and ultraviolet or cobalt blue light to assess the corneal epithelium.
 Ask about and look for signs of any rash, arthritis, or mucous membrane involvement, which could point to Stevens-Johnson syndrome, Kawasaki syndrome, Reiter syndrome, or some other syndrome that can present with conjunctivitis.
Ask about and look for signs of any rash, arthritis, or mucous membrane involvement, which could point to Stevens-Johnson syndrome, Kawasaki syndrome, Reiter syndrome, or some other syndrome that can present with conjunctivitis.
 For bacterial conjunctivitis, instruct the patient to begin therapy by applying warm or cool compresses (for comfort and cleansing) q4h, followed by instillation of ophthalmic antibiotic solutions, such as trimethoprim plus polymyxin B (Polytrim) 10 mL, 1 to 2 drops q2-6h; azithromycin 1% (AzaSite) 2.5 mL, 1 drop bid for 2 days, then 1 drop qd for 5 more days; or ciprofloxacin 0.3% solution (Ciloxan) 5 mL, 1 to 2 drops q2-4h; or instillation under the lower lid of topical antibiotic ointments (which transiently blur vision and may be cosmetically unacceptable), such as erythromycin 0.5% (Ilotycin), bacitracin–polymyxin B (Polysporin), or tobramycin 0.3% (Tobrex), 3.5 g each, with oral analgesics as needed.
For bacterial conjunctivitis, instruct the patient to begin therapy by applying warm or cool compresses (for comfort and cleansing) q4h, followed by instillation of ophthalmic antibiotic solutions, such as trimethoprim plus polymyxin B (Polytrim) 10 mL, 1 to 2 drops q2-6h; azithromycin 1% (AzaSite) 2.5 mL, 1 drop bid for 2 days, then 1 drop qd for 5 more days; or ciprofloxacin 0.3% solution (Ciloxan) 5 mL, 1 to 2 drops q2-4h; or instillation under the lower lid of topical antibiotic ointments (which transiently blur vision and may be cosmetically unacceptable), such as erythromycin 0.5% (Ilotycin), bacitracin–polymyxin B (Polysporin), or tobramycin 0.3% (Tobrex), 3.5 g each, with oral analgesics as needed.
 No clinical sign or symptom can adequately distinguish all viral from bacterial infections. Therefore, if it is unclear whether the problem is viral or bacterial, it is safest to treat it as bacterial.
No clinical sign or symptom can adequately distinguish all viral from bacterial infections. Therefore, if it is unclear whether the problem is viral or bacterial, it is safest to treat it as bacterial.
 Continue therapy for approximately 5 days or for at least 24 hours after all signs and symptoms have cleared. It should be noted that several studies suggest that bacterial conjunctivitis is self limiting and will resolve without any antibiotics in most patients. Therefore it is reasonable to use the less expensive topical preparations on the less severe cases (i.e., polymyxin B/trimethoprim–generic).
Continue therapy for approximately 5 days or for at least 24 hours after all signs and symptoms have cleared. It should be noted that several studies suggest that bacterial conjunctivitis is self limiting and will resolve without any antibiotics in most patients. Therefore it is reasonable to use the less expensive topical preparations on the less severe cases (i.e., polymyxin B/trimethoprim–generic).
 With contact lens wearers (in whom Pseudomonas is more likely to be a problem), it is more justifiable to use a more expensive fluoroquinolone (i.e., moxifloxacin [Vigamox] 0.5% solution 3 mL, 1 to 2 drops tid, or gatifloxacin [Zymar] 0.3% solution 5 mL, 1 to 2 drops every 2 hours when awake, then taper to 1 to 2 drops qid).
With contact lens wearers (in whom Pseudomonas is more likely to be a problem), it is more justifiable to use a more expensive fluoroquinolone (i.e., moxifloxacin [Vigamox] 0.5% solution 3 mL, 1 to 2 drops tid, or gatifloxacin [Zymar] 0.3% solution 5 mL, 1 to 2 drops every 2 hours when awake, then taper to 1 to 2 drops qid).
 For mild to moderate viral and chemical conjunctivitis, apply cold compresses and weak topical vasoconstrictors, such as naphazoline 0.1% (Naphcon), every 3 to 4 hours, unless the patient has a shallow anterior chamber that is prone to acute angle-closure glaucoma with mydriatics. Inform the patient or parents about the self-limited nature of most cases and the lack of benefits (with some risk for complications) from topical antibiotics. You could reassure them further by offering a delayed prescription that they could get filled if the symptoms have not resolved after 5 days. If necessary, provide mild systemic analgesics.
For mild to moderate viral and chemical conjunctivitis, apply cold compresses and weak topical vasoconstrictors, such as naphazoline 0.1% (Naphcon), every 3 to 4 hours, unless the patient has a shallow anterior chamber that is prone to acute angle-closure glaucoma with mydriatics. Inform the patient or parents about the self-limited nature of most cases and the lack of benefits (with some risk for complications) from topical antibiotics. You could reassure them further by offering a delayed prescription that they could get filled if the symptoms have not resolved after 5 days. If necessary, provide mild systemic analgesics.
 For allergic conjunctivitis, apply cold compresses and prescribe ketotifen fumarate 0.025% (Zaditor) [over the counter] or azelastine hydrochloride 0.05% (Optivar), 1 drop bid. These are H1-antihistamines and mast cell stabilizers. The antihistaminic effect of ketotifen occurs within minutes after administration and has a duration of up to 12 hours. Combining this topical therapy with systemic antihistamines may give the maximal symptomatic relief. Topical corticosteroid drops provide dramatic relief, but prolonged use increases the risk for opportunistic viral, fungal, and bacterial corneal ulceration; cataract formation; and glaucoma. When a steroid is required, loteprednol (Alrex) 0.2% suspension, 1 drop qid, reportedly does not cause cataract or glaucoma. Ophthalmologic consultation is recommended. If a severe contact dermatitis is suspected, a short course of oral prednisone is indicated (see Chapter 160).
For allergic conjunctivitis, apply cold compresses and prescribe ketotifen fumarate 0.025% (Zaditor) [over the counter] or azelastine hydrochloride 0.05% (Optivar), 1 drop bid. These are H1-antihistamines and mast cell stabilizers. The antihistaminic effect of ketotifen occurs within minutes after administration and has a duration of up to 12 hours. Combining this topical therapy with systemic antihistamines may give the maximal symptomatic relief. Topical corticosteroid drops provide dramatic relief, but prolonged use increases the risk for opportunistic viral, fungal, and bacterial corneal ulceration; cataract formation; and glaucoma. When a steroid is required, loteprednol (Alrex) 0.2% suspension, 1 drop qid, reportedly does not cause cataract or glaucoma. Ophthalmologic consultation is recommended. If a severe contact dermatitis is suspected, a short course of oral prednisone is indicated (see Chapter 160).
 If the problem is dry eye (keratoconjunctivitis sicca), treat with artificial tear drops (Refresh Tears, Lacri-Lube, Gen Teal). If chlorine from a swimming pool is causing chronic red eye (student athletes and recreational swimmers), using a nonsteroidal anti-inflammatory drug (NSAID) eye drop (Ketorolac [Acular] 0.5%, 1 drop qid) may provide some comfort, but swimming goggles are the best solution.
If the problem is dry eye (keratoconjunctivitis sicca), treat with artificial tear drops (Refresh Tears, Lacri-Lube, Gen Teal). If chlorine from a swimming pool is causing chronic red eye (student athletes and recreational swimmers), using a nonsteroidal anti-inflammatory drug (NSAID) eye drop (Ketorolac [Acular] 0.5%, 1 drop qid) may provide some comfort, but swimming goggles are the best solution.
 Instruct the patient to follow up with an ophthalmologist if the infection does not completely resolve within 2 days. Obtain earlier consultation if there is any involvement of the cornea or iris, impaired vision, light sensitivity, inequality in pupil size, or other signs of corneal infection, iritis, or acutely increased intraocular pressure. In addition, refer patients who have had eye surgery, have a history of herpes simplex keratitis, or wear contact lenses to an ophthalmologist.
Instruct the patient to follow up with an ophthalmologist if the infection does not completely resolve within 2 days. Obtain earlier consultation if there is any involvement of the cornea or iris, impaired vision, light sensitivity, inequality in pupil size, or other signs of corneal infection, iritis, or acutely increased intraocular pressure. In addition, refer patients who have had eye surgery, have a history of herpes simplex keratitis, or wear contact lenses to an ophthalmologist.
 Return to school or daycare should parallel behavior in the common cold.
Return to school or daycare should parallel behavior in the common cold.
What Not To Do:
 Do not forget to wash hands and equipment after examining the patient; herpes simplex or epidemic keratoconjunctivitis (Figure 14-4) can be spread to clinicians and other patients. For viral forms of conjunctivitis, do not forget to instruct the patient regarding the contagious nature of the disease and the importance of hand washing and use of separate towels and pillows for 10 days after the onset of symptoms.
Do not forget to wash hands and equipment after examining the patient; herpes simplex or epidemic keratoconjunctivitis (Figure 14-4) can be spread to clinicians and other patients. For viral forms of conjunctivitis, do not forget to instruct the patient regarding the contagious nature of the disease and the importance of hand washing and use of separate towels and pillows for 10 days after the onset of symptoms.

Figure 14-4 Epidemic keratoconjunctivitis. (Adapted from Palay DH, Krachmer JH: Primary Care Ophthalmology, ed 2. St Louis, 2005, Mosby.)
 Do not use ophthalmic neomycin, because of the high incidence of hypersensitivity reactions.
Do not use ophthalmic neomycin, because of the high incidence of hypersensitivity reactions.
 Do not patch an infected eye; this interferes with the cleansing function of tear flow.
Do not patch an infected eye; this interferes with the cleansing function of tear flow.
 Do not routinely culture an eye discharge. Cultures should only be obtained with neonatal conjunctivitis or when the infection does not respond to treatment.
Do not routinely culture an eye discharge. Cultures should only be obtained with neonatal conjunctivitis or when the infection does not respond to treatment.
 Do not use topical antiviral drugs for simple cases of viral conjunctivitis. They are of no benefit.
Do not use topical antiviral drugs for simple cases of viral conjunctivitis. They are of no benefit.
 Do not give steroids without arranging for ophthalmologic consultation, and never give steroids if a herpes simplex infection is suspected.
Do not give steroids without arranging for ophthalmologic consultation, and never give steroids if a herpes simplex infection is suspected.
 Do not make a diagnosis of conjunctivitis unless visual acuity is normal and there is no evidence of corneal involvement, iritis, or acute glaucoma.
Do not make a diagnosis of conjunctivitis unless visual acuity is normal and there is no evidence of corneal involvement, iritis, or acute glaucoma.
Discussion
Warm or cool compresses are soothing for all types of conjunctivitis, but antibiotic drops and ointments should be used only when bacterial infection is likely. Neomycin-containing ointments and drops should probably be avoided because allergic sensitization to this antibiotic is common. Any corneal ulceration found with fluorescein staining requires ophthalmologic consultation. Most viral and bacterial conjunctivitis hosts will resolve spontaneously, with the possible exception of Staphylococcus, Meningococcus, and Gonococcus organism infections, which can produce destructive sequelae without treatment.
Most bacterial conjunctivitis in immunocompetent hosts is caused by Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus, or Moraxella catarrhalis. Routine conjunctival cultures are seldom of value, but Gram’s method should be used to stain and culture any copious yellow-green, purulent exudate that is abrupt in onset and quickly reaccumulates after being wiped away (findings with both Neisseria gonorrhoeae and N. meningitidis). N. gonorrhoeae infection confirmed by gram-negative intracellular diplococci requires immediate ophthalmologic consultation and treatment with IM ceftriaxone as well as topical antibiotics. Corneal ulceration, scarring, and blindness can occur in a matter of hours.
Chlamydial conjunctivitis will usually present with lid droop, mucopurulent discharge, photophobia, and preauricular lymphadenopathy. Small, white, elevated conglomerations of lymphoid tissue can be seen on the upper and lower tarsal conjunctiva, and 90% of patients have concurrent genital infection. In adults, doxycycline, 100 mg PO bid for 3 weeks, or azithromycin (Zithromax), 1 g PO × 1 dose, plus topical tetracycline (Achromycin Ophthalmic Ointment) 1%, q3-4h for 3 weeks should control the infection. (Also treat sexual partners.) Although it is somewhat difficult to culture, Chlamydia can be confirmed by monoclonal immunofluorescent antibody testing from conjunctival smears or by polymerase chain reaction (PCR) testing.
Newborn conjunctivitis requires special attention and culture of any discharge, as well as immediate ophthalmologic consultation. The pathogens of greatest concern are N. gonorrhoeae, C. trachomatis, and herpes simplex virus (HSV). N. gonorrhoeae infections usually begin 2 to 4 days after birth, whereas C. trachomatis infections start 3 to 10 days after birth. If conjunctivitis is noted on the first day of life, this is more likely to be a reaction to silver nitrate prophylaxis.
Epidemic keratoconjunctivitis is a bilateral, painful, highly contagious conjunctivitis usually caused by an adenovirus (serotypes 8 and 19). The eyes are extremely erythematous, sometimes with subconjunctival hemorrhages. There is copious watery discharge and preauricular lymphadenopathy. Treat the symptoms with analgesics, cold compresses, and, if necessary, corticosteroids (loteprednol [Alrex], 0.2% suspension, 1 drop qid). Because the infection can last as long as 3 weeks and may result in permanent corneal scarring, provide ophthalmologic consultation and referral. Patients should be instructed on hand washing with soap, changing pillowcases, and not sharing household items. Patients should also be told to avoid communal activities (work, school, daycare) for 10 to 14 days or while there is a discharge, to avoid infecting others. These patients should also avoid wearing contact lenses. Nondisposable contacts should be sterilized, and patients with disposable contacts should use new lenses after 14 days.
Herpes simplex conjunctivitis is usually unilateral. Symptoms include a red eye, photophobia, eye pain, and blurred vision with a foreign-body sensation. There may be periorbital vesicles, and a branching (dendritic) pattern with bulbar terminal endings of fluorescein staining confirms the diagnosis. Treat with trifluridine 1% (Viroptic), 1 drop q2h, 9×/day, then reduce dose to 1 drop q4-6h after reepthelialization for another 7 to 14 days (maximum of 21 days of treatment). In addition, instill 1 cm of Vidarabine (Vira-A) ointment 5× daily at 3-hour intervals up to 21 days. Also give acyclovir, 800 mg PO 5× daily for 7 to 10 days, or valacyclovir (Valtrex), 1 g bid for 7 to 10 days. Analgesics and cold compresses will help provide comfort. Cycloplegics, such as homatropine 5% (1 to 2 drops bid to tid), may help control pain resulting from iridocyclitis. Topical corticosteroids are contraindicated, because they can extend duration of the infection. Because corneal herpetic infections frequently leave a scar, ophthalmologic consultation is required.
Herpes zoster ophthalmicus is shingles of the ophthalmic branch of the trigeminal nerve, which innervates the cornea and the tip of the nose. It begins with unilateral neuralgia, followed by a vesicular rash in the distribution of the nerve. Ophthalmic consultation is again required (because of frequent ocular complications), but topical corticosteroids may be used. Prescribe systemic acyclovir (Zovirax), 800 mg q4h (5× daily) for 7 to 10 days, or valacyclovir (Valtrex), 1 g PO tid for 7 to 10 days.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


