Proper positioning for BESS Balance Testing – Double Leg Stance: Feet together, side by side.

Proper positioning for BESS Balance Testing – Tandem Stance: Heel-to-toe with the patient’s nondominant leg in the back.

Proper positioning for BESS Balance Testing – Single Leg Stance: Balance on the nondominant leg.
Differential Diagnosis – Emergent and Common Diagnoses
Keep the initial differential diagnosis quite broad.
Quickly narrow down the differential using history and physical exam, and make sure to rule out the emergent diagnoses.
Management and Clinical Pathway
If the patient meets the diagnostic criteria for concussion, the majority of the emergency management should involve patient education and counseling.
It is important to always maintain a high degree of suspicion for concussion and err on the side of caution when making this diagnosis.
If the diagnosis is uncertain, do not let athletes return to sports until they have followed up with their primary care or sports medicine physician.
Follow the mantra, “When in doubt, sit them out.”
Imaging is not indicated in the emergency department for diagnosis of concussion. However, if the patient has focal neurologic deficits or there is concern for underlying severe head injury, brain imaging should be obtained. If the patient has signs of a traumatic blow to the head or face, consider imaging to rule out underlying pathology.
Medication management: Nonsteroidal anti-informatory drugs (NSAIDs) should NOT be taken in the first seventy-two hours after a concussion. This is recommended by the current position statements on concussion in sport because of the theoretical risk of bleeding.4 If the patient has a headache or neck or back pain, acetaminophen should be taken.
Brain rest recommendations:
The patient should be advised that the more the brain rests, the quicker the recovery. Brain rest entails resting as much as possible, avoiding physical activity, avoiding computer/cellular use, and, when possible, taking one to two days off from work. In general, patients should avoid any activities that make their symptoms worse. While no further damage will ensue from working, texting, or using the brain, it may take slightly longer for symptoms to resolve.1,4,13
| Emergent Diagnoses | Common Diagnoses |
|---|---|
| Intracranial/subarachnoid hemorrhage | Simple hematoma |
| Subdural/epidural hematoma | Simple contusion |
| Second impact syndrome | Cervical muscle strains |
| Chronic traumatic encephalopathy | Concussion |
| Skull fracture | Minor head injury |
| Cervical spine fracture | |
| Spinal cord injury without radiographic abnormality (SCIWORA) |
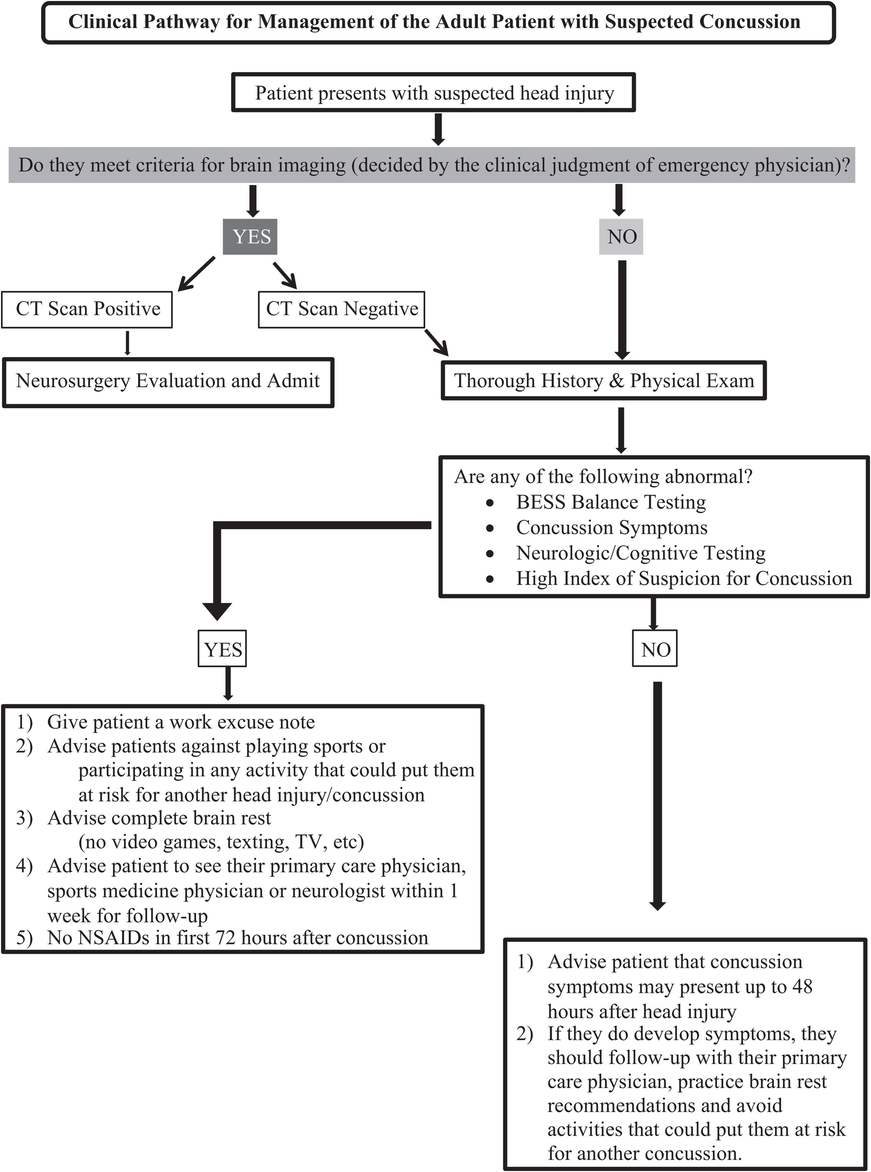
Clinical pathway for the adult patient with suspected concussion.
Disposition
Follow-up: Every patient should follow-up with their primary care doctor (PCP), sports medicine specialist, or neurologist approximately one to three days after a concussion is sustained.1,4,5
Work/athletics recommendations: The more the patient rests the brain, the quicker the recovery will be.1,4,5 In addition, stressing the brain with work, studying, reading, and athletics (from increasing the heart rate and blood pressure) may worsen symptoms during and after the activity. If the patient chooses to go to work, it will not cause any further damage to the brain. The patient should not engage in any activity which could potentially risk sustaining a second concussion before fully healing from the current concussion. See the Pediatrics section for school recommendations.
Brain rest recommendations: The patient should be advised to avoid cellular phone use (including texting), computer use, television, reading, and any activity which raises the heart rate above 100 beats per minute or increases their blood pressure.
Return to work and return to play recommendations: Patients should be advised to obtain clearance to return to sports from their PCP and/or sports medicine physician. It is important that the emergency physician does not clear patients to return to physical activity or sports from the emergency department. General anticipatory guidance may include advising the patient to slowly begin returning to work as tolerated by symptoms. Athletes should not return to play until after they have been completely symptom free for at least forty-eight hours.1,3–5,13 The return to play should be a graded progression of activity so that the patient may gradually ease back into the gym and gradually increase the heart rate over many days without triggering any concussion symptoms. The patient may not return to contact sports until completing return to play progression symptom free and being cleared by either the PCP, sports medicine physician, or neurologist.
Return to play progression:
Step 1: Light general conditioning (15- to 20-minute light workout).
Step 2: General conditioning and sport-specific skill work (individual 30-minute light workout).
Step 3: General conditioning and skill work with team (no contact, workout up to 60 minutes).
Step 4: General conditioning, skill work, and team drills (no contact, workout up to 75 minutes).
Complications
Second impact syndrome: This is a rare life-threatening condition that may occur when an individual sustains a second concussion before the brain has completely healed from the first concussion.6,7.This typically affects young healthy athletes and results in cerebral edema, potential brain herniation, and death.6,7 It is very important for the emergency physician to educate the patient regarding when to return to play and to warn them of the risk of second impact syndrome, especially with contact sports, while symptoms persist.
Chronic traumatic encephalopathy (CTE): This is a rare progressive neuropathological disease that results from repetitive brain trauma.1,5,14 It has been described in athletes such as boxers and football players.1,5,14 Symptoms of CTE include memory disturbances, behavior and personality changes, and speech and gait abnormalities.1,5,14
Pediatric Considerations
Management and Clinical Pathway
Pediatric Emergency Care Applied Research Network (PECARN)15 – Use this validated decision rule to determine need for brain imaging in a pediatric patient with head injury.
History and physical – Complete same H&P as described earlier in the adult section.
Determine whether the patient has symptoms of a concussion, more than ten errors on BESS balance testing, or if there is a high index of suspicion.11,12
If any of the above are positive, then follow the six recommendations provided in Figure 11.5.
If none of the above are positive, then advise the patient and parents that concussion symptoms may develop up to forty-eight hours after the head injury. If symptoms develop, the patient should stay out of physical education (PE) and any sports and should follow-up with their PCP or sports medicine physician.
Patient and parent education (see detailed outline later).
Recommendations for pediatric disposition and management.1,4
School excuse note – Initially it is best to keep the patient out of school for the first twenty-four to forty-eight hours following a concussion to allow for brain rest. After this period, the child may return to school as able based upon symptoms.
Patient and parents should be counseled that certain school accommodations may need to be made if symptoms prevent the patient from doing schoolwork. Accommodations may include:
No tests/quizzes/exams; if the patient must take an exam, request open-note and open-book exams, and allow for extra exam time.
Allow the child to go to the nurse’s office for acetaminophen administration for headaches as needed.
Allow the child to go to nurse’s office for rest and naps as needed throughout the day.
Allow the child frequent breaks from the classroom if experiencing concussion symptoms.
Restrict PE and recess until cleared by PCP or sports medicine physician.13
Allow for use of an elevator (if available) instead of climbing stairs.
Allow the child to wear sunglasses in the classroom as needed for light sensitivity.
PE/recess/sports excuse note until cleared by PCP or sports medicine physician.
Advise parents/patients against doing any activity that puts the patient at risk for another concussion.
Complete brain rest – Patients should avoid watching television, playing video games, texting, emailing, using the computer, reading, and so forth. The more the patient rests and relaxes, the better.1,4
See PCP or sports medicine physician within one to three days for follow-up and potential clearance for return to play and return to school.
Advise against taking NSAIDs for symptoms of headache in the first seventy-two hours after a concussion because of the theoretical risk of bleeding.4
Return to play – While the emergency physician will not be guiding the child’s return to play, it is important to know what this will involve.
Return to play is a guided stepwise progression of activities so as to minimize return of concussive symptoms.
Return to play should not begin until the child has been symptom free for at least seventy-two hours. 4,5,13,16
Neurocognitive testing (such as the Impact Test®) is usually completed prior to clearance for return to play. This includes testing of verbal memory, visual memory, and reaction time via a computer-based exam.
Baseline testing is completed by most high school and college athletes prior to the start of the athletic season. This has become standard of care.
If a concussion is sustained during the season, neurocognitive testing is repeated prior to clearance for return to play. The new composite score is compared to the baseline score.
An athlete should not be cleared for return to play until performance is at or near baseline cognitive levels.
It is known that physical symptoms resolve prior to complete return of reaction time, memory, and cognition. Therefore, neurocognitive computer-based testing is used as a tool to detect subclinical concussions in athletes.
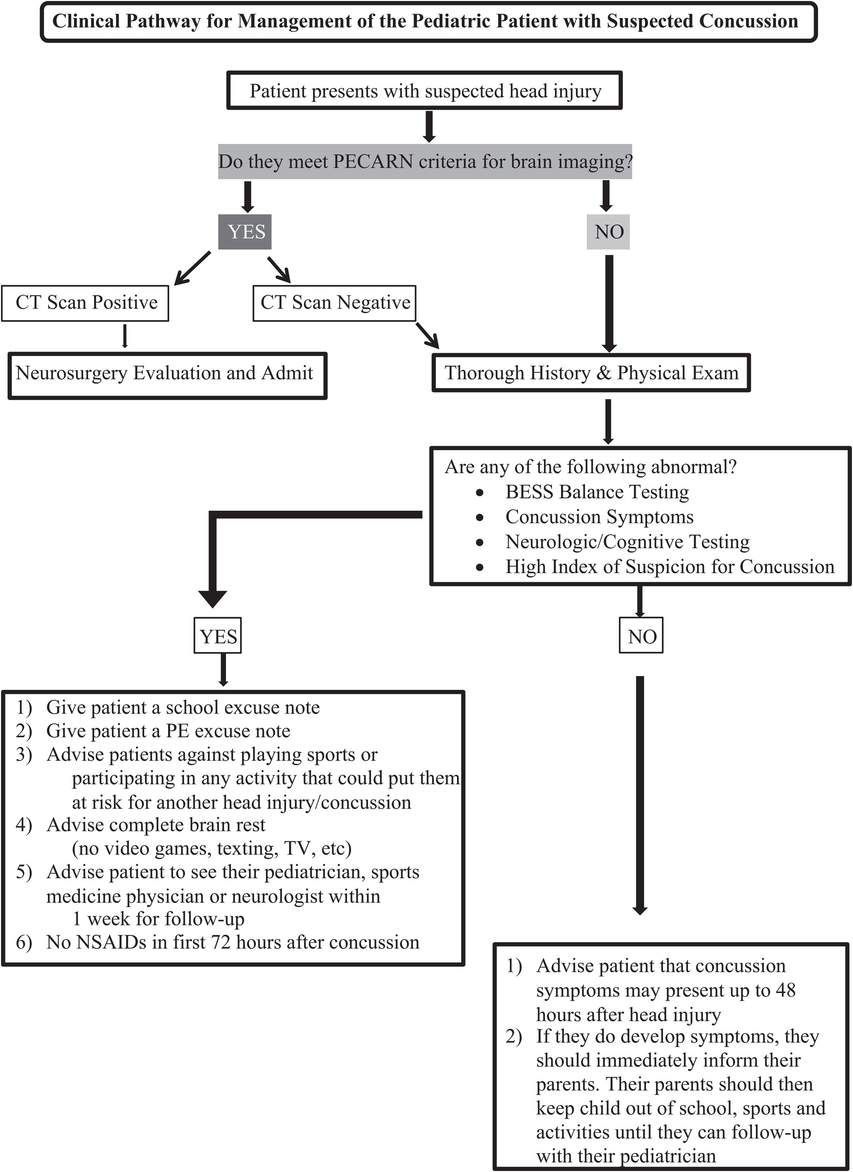
Clinical pathway for the pediatric patient with suspected concussion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








