Chapter 16 Complications of Sacroiliac Joint Injection and Lateral Branch Blocks, Including Water-Cooled Rhizotomy
 Appropriate Accreditation Council for Graduate Medical Education mentored subspecialty training in interventional pain management is vital to ensure patient-centered care.
Appropriate Accreditation Council for Graduate Medical Education mentored subspecialty training in interventional pain management is vital to ensure patient-centered care. Accurate and expertly placed needles in appropriately selected patients are essential to ensure accurate diagnosis and successful treatment.
Accurate and expertly placed needles in appropriately selected patients are essential to ensure accurate diagnosis and successful treatment. The sacroiliac joint is a large structure with rich, variable innervation. Numerous techniques have been described for intraarticular, extraarticular, lateral branch, and RF treatments.
The sacroiliac joint is a large structure with rich, variable innervation. Numerous techniques have been described for intraarticular, extraarticular, lateral branch, and RF treatments. RF treatments are not created equal, and an appreciation for each underscores their different applications and associated risks.
RF treatments are not created equal, and an appreciation for each underscores their different applications and associated risks. Common complications, regardless of RF modality used, include transient increased localized pain and usually self-limiting neuritis.
Common complications, regardless of RF modality used, include transient increased localized pain and usually self-limiting neuritis. Infectious complications are uncommon if appropriate sterile technique and avoidance of multidosing from single-dose vials are used.
Infectious complications are uncommon if appropriate sterile technique and avoidance of multidosing from single-dose vials are used. Injection of steroids or enteral antiinflammatory medications may help with postprocedural pain and neuritis.
Injection of steroids or enteral antiinflammatory medications may help with postprocedural pain and neuritis.Introduction
Estimates of sacroiliac joint sources of back and leg pain have been estimated to be between 10% and 38% using compared diagnostic injections, with a false-positive rate estimated between 0% and 53.8%.1–3 Not only have diagnostic provocative tests failed to be accurate,4,5 but there have been numerous efforts to treat sacroiliac joint pain, including intraarticular injections, extraarticular injections, radiofrequency (RF) treatments, fusion, and prolotherapy6–9 with level II-3 evidence for both short- and long-term relief.2
Sacroiliac pain or dysfunction has been implicated in diverse patient populations and associated morbidities, including pediatric low back pain, pregnancy, cancer, infection, ankylosing spondylitis, and inflammatory bowel disease.10–13 Controversy surrounds diagnostic accuracy and technique14–21 because some advocate intraarticular injections but others advocate extraarticular injections or lateral branch blocks before RF treatment. Summarily, interventions are directed to either the afferent nociceptive nerves supplying the joint or the actual joint itself. A corollary can be drawn to zygapophyseal treatments because intraarticular or median branch blocks are used before RF treatment, just as sacroiliac intraarticular injection or lateral branch blocks are performed before using RF. Although widely accepted clinically, this treatment algorithm has recently been questioned.3
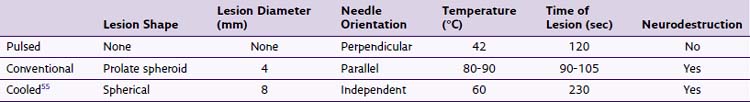
Before proceeding, readers are directed to the chapters that correspond to sacroiliac joint injections; lateral branch blocks; and traditional (see Fig. 15-2), pulsed, and cooled RF treatments (see Fig. 15-5). A brief review of the differences in RF modalities are listed in Table 16-1, and reviewed elsewhere in the text (see Chapter 7). Other modalities to treat sacroiliac joint pain include fusion and prolotherapy,22 this chapter focuses on complications specific to RF neurotomy.
Even after appropriate safeguards and training, significant complications have been described in scattered case reports. Theoretical risks are listed in Box 16-1, and they are typically localized or systemic in nature.
Selected Complications
Meta-analysis of treatment outcomes is difficult because the treatment arm is highly variable regarding RF technique, inconsistent patient selection, outcome endpoints, and definitions of success. Although there is a plethora of literature describing sacroiliac joint interventions, few describe complications.2–4,9,10,13,23–29
Postprocedure Pain or Neuritis
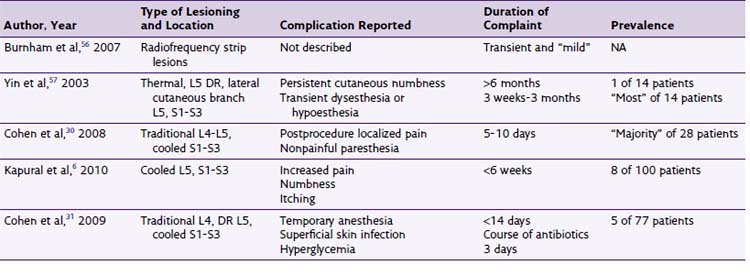
Transient postprocedural pain often follows RF treatments and has been described in numerous studies for lumbar facetogenic interventions; however, few describe sacroiliac lateral branch denervation. Cooled RF and traditional thermal RF have been accompanied by postprocedure local pain (Table 16-2), typically of a transient nature,6,30,31 and Vallejo et al9 reported that no complications arose from pulsed RF treatments of the lateral branches.
No published study has compared the efficacy and complications of cooled versus traditional RF. In an unpublished retrospective analysis of 88 patients at the Cleveland Clinic, there was no statistically significant difference in duration of pain relief, and anecdotally, more patients who underwent cooled RF reported transient postprocedure localized back pain. Kapural et al6 described transient itching, numbness, and pain.
Steroids are injected after denervation to lessen postprocedural pain. This may seem counterintuitive because the goal in thermal rhizotomy is to create a histologically detectable lesion, blocking neural afferent nociception. Dobrogowsi et al32 investigated strategies to reduce the inflammatory pain associated with the lesioning using pentoxifylline or methylprednisolone. In a randomized prospective trial, patients were randomized to 1 mL of intraoperative methylprednisolone, pentoxifylline, or saline. No “severe local tenderness” was reported in either the methylprednisolone group or the pentoxifylline group.32 Other authors33 contend that 3-day dosage of enteral diclofenac is effective in reducing procedural pain after conventional RF neurotomy of lumbar median branches.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree