Chapter 15 Complications of Radiofrequency Rhizotomy for Facet Syndrome
 Appropriate Accreditation Council for Graduate Medical Education mentored subspecialty training in interventional pain management is vital to ensure patient-centered care.
Appropriate Accreditation Council for Graduate Medical Education mentored subspecialty training in interventional pain management is vital to ensure patient-centered care. Common complications, regardless of the RF modality used, include transient increased localized pain and usually self-limiting neuritis.
Common complications, regardless of the RF modality used, include transient increased localized pain and usually self-limiting neuritis. Infectious complications are less common than in the diagnostic or therapeutic steroid injections, potentially related to the thermal injury created.
Infectious complications are less common than in the diagnostic or therapeutic steroid injections, potentially related to the thermal injury created. Injection of steroid or enteral antiinflammatory medications may help with postprocedural pain and neuritis.
Injection of steroid or enteral antiinflammatory medications may help with postprocedural pain and neuritis.Introduction
Rhizotomy techniques have revolutionized treatment for many pain states and are commonly used to treat facetogenic pain after appropriate controlled diagnostic injections. Relatively recent reviews approximated lumbar, thoracic, and cervical zygapophyseal pain to be 31%, 40%, and 39%, respectively, using dual controlled diagnostic injections (Table 15-1).1–3
Table 15-1 Prevalence and Diagnostic Accuracy of Zygapophyseal Joint Pain
| Prevalence (%)* | Diagnostic Accuracy: False Positive Rate* (%) | |
|---|---|---|
| Cervical | 39 (23–45) | 45 (37–52) |
| Thoracic | 40 (33–48) | 42 (33–51) |
| Lumbar | 31 (28–33) | 30 (27–33) |
* 95% confidence interval using 80% pain reduction.
Data from Manchukonda R, Manchikanti KN, Cash KA, et al: Facet joint pain in chronic spinal pain: An evaluation of prevalence and false-positive rate of diagnostic blocks, J Spinal Disord Tech 20:539-545, 2007.
Facetogenic injections are required to make diagnosis because no physical, historical, or radiographic examination feature are unreliable,4 but attempts at noninvasive diagnostic strategies are ongoing.5 Interestingly, later Cohen et al6 looked at the cost effectiveness of one, two, or no controlled diagnostic injection before facet radiofrequency (RF) treatment and summarized that from a cost analysis perspective, proceeding to RF denervation before diagnostic injection was superior, and although efficacy determination was not a study endpoint, the treatment outcome related to duration and magnitude of pain relief was greater for the dual diagnostic blockade group.
Regardless of the diagnostic treatment algorithm used, RF techniques are a safe and effective means to treat zygapophyseal pain.7 However, RF techniques are not created equal, and an understanding of the different modalities is crucial to understand the potential pitfalls and safety concerns.
Background
Thermal (Traditional, Conventional, or Continuous) Radiofrequency
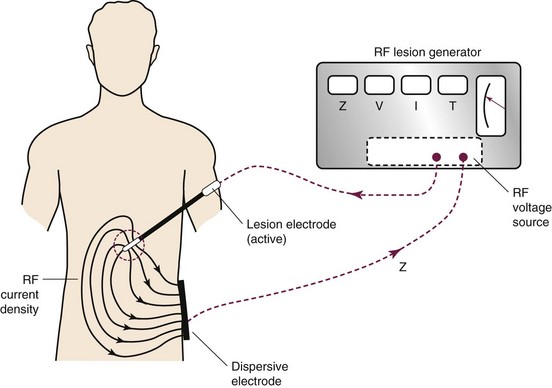
Thermal RF was first introduced in the 1930s. The thermal lesion is created by the introduction of an insulated electrode with an active tip of (2 to 10 mm), a dispersal plate, and a power source to complete the circuit (Fig. 15-1).
High-frequency electrical current is then applied adjacent to the structure of the nerve that is intended to ablate; such current leads to ionic oscillation and frictional dissipation of the ions and electrolytes, which produce heat. The heat produced is directly related to the amplitude of the applied current and electrode size and indirectly related to distance from the electrode. The tip of the electrode measures the tissue temperature. Larger lesions are created by increased temperature, size of the electrode, and duration of applied current. Monopolar lesioning is performed when one electrode is used. Bipolar lesioning occurs when two electrodes are used in close proximity to one another. Laboratory evidence suggests that cellular damage occurs at temperatures of 60° to 65°C. As suggested by the aforementioned isotherm mapping from the electrode tip, 80° to 85°C is required at the needle tip, where the desired 60° to 65°C is achieved in the surrounding tissue, producing a prolate ovoid-shaped lesion (Fig. 15-2). Therefore, because the lesion created does not extend distal to the electrode, proper electrode position is parallel to the target nerve.

Fig. 15-2 Traditional thermal radiofrequency lesion.
(Courtesy of Dr. Nagy Mekhail, MD, PhD, Cleveland Clinic.)
The neurotomy created by the thermal technique is dependent on proximity to the targeted nerve, size of electrode, the temperature (or amplitude of current) applied, and the duration of lesioning. When applied immediately adjacent to the dorsal root ganglion, temperatures of 45°, 55°, 65°, 75°, and 85°C produce complete destruction of unmyelinated and near complete destruction of myelinated fibers.8
Pulsed Radiofrequency
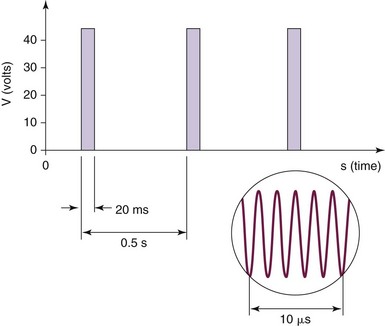
Pulsed RF was first introduced in 1998, and the aforementioned circuit is used. Interestingly, there is no creation of a histologic lesion, and no nerve degeneration occurs (no Wallerian degeneration). The treatment is produced by providing current of 50,000 Hz in 20-msec pulses at a frequency of 2 per second. The temperature is maintained to be below 42°C or 45 V (Fig. 15-3). The greatest current density delivered is at the tip of the electrode; so ideal placement is perpendicular to the target nerve.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree