Complications of Procedures
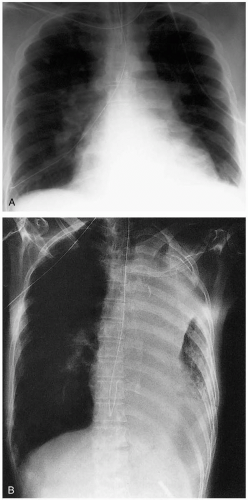
31-1 Nasogastric Tube Complications
Mark Silverberg
Indications
Nasogastric tubes (NGTs) can be used to decompress the upper gastrointestinal tract if enteric obstruction exists. In the past, NGTs were used to remove stomach contents after an overdose, but this procedure has fallen into disuse. If a patient cannot tolerate oral intake, NGTs can serve as a route of delivery for medications, oral contrast media, or enteral nutrition.1
Predisposing Factors
Older age and the existence of comorbid conditions increase the risk of complications in general.2 Patients who are anticoagulated are at high risk for bleeding from nasal trauma during tube placement. Altered mental status, prolonged supine position, neuromuscular disease, and structural abnormalities make aspiration and tube malposition more likely.1,2
Complications
Complications may be traumatic in nature and include injury to or bleeding from the nasopharyngeal structures and the apparatus of phonation.1,2 Hemorrhage may be severe enough to critically compromise the airway.1 Necrosis of nasal cartilage may occur if the tube is not properly secured in place.1 Malpositioning of the NGT intracranially, into false passages, or into the trachea is common.1 Inadvertent entry into the respiratory tract can result in pulmonary injury, hydrothorax, pneumothorax, empyema or pulmonary abscess formation, or potentially lethal installation of fluid into the lungs.2 After the tube is in place, it can become clogged, cracked, kinked, knotted, or dislodged.2 Sinusitis and esophageal stricture can occur from prolonged NGT use.2
Complication Prevention
Nasal trauma can be avoided and NGT passage facilitated by administration of intranasal viscous lidocaine and use of adequate amounts of lubricant for comfort, and/or use of lidocaine with epinephrine for comfort and vasoconstriction.1 To prevent NGT dislodgement, the proximal end of the tube can be secured with tape or a nasal bridle.2 However, use of the bridle may be associated with erosion of the nasal septum.2 Deep placement of the NGT into the small bowel significantly reduces the frequency of aspiration pneumonia compared with intragastric feeding, as does keeping the head of the bed elevated and adding a prokinetic agent.2 Verification of tube position by plain radiography is always advisable.
Complication Treatment
Procedure-related epistaxis is usually self-limited and rarely requires nasopharyngeal packing.2 Aspiration pneumonia should be treated in the usual fashion with systemic antibiotics. If the position of an NGT is questionable, the tube should be removed and replaced.
REFERENCES
1. Gallacher BP. An atraumatic nasogastric tube guide probe. Am J Emerg Med 1995;13:252-253.
2. McClave SA, Chang WK. Complications of enteral access. Gastrointest Endosc 2003;58:739-751.
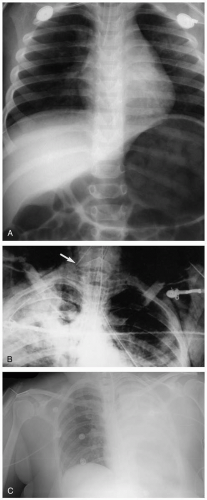
31-2 Endotracheal Intubation Complications
Mark Silverberg
Indications
Endotracheal intubation (ETI) is indicated for definitive airway control in patients with respiratory failure, hypoxemia, inability to maintain an airway themselves, or high risk of aspiration, in addition to patients undergoing operative procedures. Occasionally, ETI is indicated if the behavior of the patient presents a risk to his or her well-being.
Predisposing Factors
Preexisting poor dentition or a “difficult airway” predisposes the patient to potential laryngoscopic dental trauma.1 Facial trauma with or without basilar skull fractures increases the risk of misplacement of the endotracheal tube (ETT).1 Anticoagulation or coagulopathy increases the risk of oropharyngeal bleeding, which may make cord visualization difficult. Preexisting temporomandibular joint disease may predispose to jaw dislocations or decreased mouth aperture, increasing the likelihood of ETT misplacement.1 Concomitant use of a nasogastric tube may increase the risk for aspiration.1
Complications
Acute complications of ETI include local trauma from the laryngoscope, ETT, or cuff that leads to injury to the teeth, tongue, uvula, buccal mucosa, epiglottis, arytenoids, trachea, esophagus, or lingual nerve.1 The ETT can cause trauma as it is passed, leading to vocal cord injury or paralysis, and it can even be lost into the esophagus or trachea.1 It can be misplaced into any number of sites, including the esophagus, cranium, and neck soft tissues.1 Aspiration of vomit or foreign bodies (e.g., teeth, the laryngoscope bulb, other instrumentation) may occur during the intubation procedure.1 Chronically, subglottic stenosis can develop secondary to granuloma formation if the ETT must remain in place for a long period or as a result of cuff inflation.1
Complication Prevention
To prevent blade trauma, the laryngoscopist should pay careful attention to the proximal portion of the blade during the intubation procedure. Proton-pump inhibitors or histamine type 2 (H2) receptor blockers may be administered before intubation to decrease the risk of damage caused by aspiration, but this remains controversial.1 A fluid-filled cuff may be used when working with nitrous oxide to prevent diffusion of the gas into an air-filled cuff and to stop overinflation.1
Complication Treatment
Oral trauma may be treated in the usual fashion, and the patient’s tetanus status should be checked and updated if necessary. Tube placement should be confirmed in the usual manor, and the tube should be adjusted or removed if it is in the wrong place. Vocal cord paralysis usually recovers spontaneously.1
REFERENCES
1. Weber S. Traumatic complications of airway management. Anesthesiol Clin North Am 2002;20:503-512.
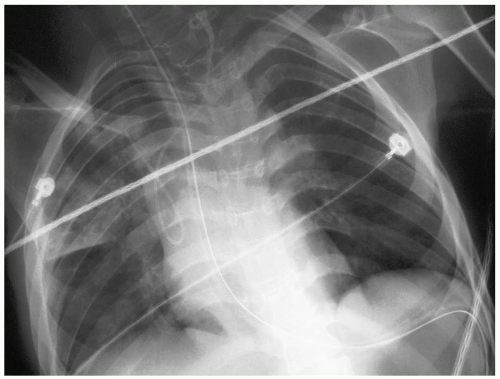
31-3 Internal Jugular and Subclavian Central Line Complications
Mark Silverberg
Indications
Common indications for central venous catheter (CVC) placement are hemodialysis, hemodynamic monitoring, fluid resuscitation when peripheral access is difficult or inadequate, and centrally administered medications such as catecholamines or parenteral nutrition.1
Predisposing Factors
Many factors predispose certain patient populations to complications of CVC placement. Asthmatics and patients with chronic obstructive pulmonary disease have hyperinflated lungs, making pneumothorax more likely. Cancer patients may be hypercoagulable and have been reported to have rates of catheter-related thrombosis greater than 50% in some instances.1
Complications
Many complications have been documented in association with CVC placement, with an overall complication rate of 1% to 10%.1 Complications can be vascular, infectious, or physical in nature. According to the meta-analysis of Ruesch and colleagues,1 vascular complications such as arterial punctures were most common and were seen more frequently when a line was placed via the internal jugular approach rather than the subclavian route. In contrast, the physical complication of catheter malpositioning (subcutaneous, arterial, or erroneous venous location) was less likely when attaining internal jugular access, compared with subclavian cannulation. No statistical difference was noticed between the two approaches when comparing the incidence of vessel thrombosis/stenosis or hemothorax/pneumothorax.1 Catheter-related infection remains an important cause of nosocomial infection; bacteremia and insertion-site infections were found to be more common with internal jugular lines, but the data were not statistically significant. Other, less common complications include vessel or cardiac perforation, cardiac tamponade, air or solid emboli (including guidewires), and injuries to the thoracic duct, esophagus, trachea, or nerves.
Complication Prevention
Ultrasound guidance is an effective method for decreasing the incidence of arterial puncture or pneumothorax formation.1 Infection rates can be reduced by following strict aseptic techniques and conscientious hand-washing protocols.
Complication Treatment
Treatment depends on the nature of the particular complication. Hematoma formation may be treated traditionally with warm packs and direct pressure if the puncture site is accessible. Large vascular injuries may require surgical repair. Pneumothoraces should be treated with chest tube placement. In cases of centralline infection, the catheter should be removed and the tip cultured for pathogen identification and sensitivity. Vessel thrombosis should be treated as any other venous thrombus.1
REFERENCES
1. Ruesch S, Walder B, Tramèr M. Complications of central venous catheters: internal jugular versus subclavian access—a systematic review. Crit Care Med 2002;30:454-460.
31-4 Femoral Line Complications
Mark Silverberg
Indications
Common indications for central venous catheter (CVC) placement include hemodialysis, hemodynamic monitoring, fluid resuscitation when peripheral access is difficult or inadequate, and centrally administered medications or parenteral nutrition.
Predisposing Factors
The inguinal region of the leg should be free of preexisting infection during the insertion process; otherwise, line sepsis is more likely.1 Patients who are anticoagulated are at increased risk for excessive bleeding and hematoma formation during catheter insertion.1 In contrast, patients are at increased risk for deep vein thrombosis (DVT) if they are in a hypercoagulable state (e.g., protein C or S deficiency, presence of the lupus anticoagulant).1 Other risk factors for DVT include recent surgery, pelvic fracture, and lower-extremity ischemia.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree