Chapter 8 Complications of Lumbar Spine Fusion Surgery
 Many patients have back and leg pain arising from lumbar spinal stenosis with or without instability.
Many patients have back and leg pain arising from lumbar spinal stenosis with or without instability. Conservative treatment in the form of physical therapy, chiropractic care, medications, and injections should be the first line of care. However, when conservative modalities fail and there is obvious instability or potential for instability, as well as acute neurologic changes, spinal surgery must be considered.
Conservative treatment in the form of physical therapy, chiropractic care, medications, and injections should be the first line of care. However, when conservative modalities fail and there is obvious instability or potential for instability, as well as acute neurologic changes, spinal surgery must be considered. Lumbar surgery often includes decompression of the soft and bony tissues contributing to central and neuroforaminal stenosis that may be compressing the spinal cord or nerve roots. This can reliably relieve pain, numbness, and weakness.
Lumbar surgery often includes decompression of the soft and bony tissues contributing to central and neuroforaminal stenosis that may be compressing the spinal cord or nerve roots. This can reliably relieve pain, numbness, and weakness. It is crucial to understand the specific complications related to lumbar spinal fusion and to recognize and treat them immediately if they occur.
It is crucial to understand the specific complications related to lumbar spinal fusion and to recognize and treat them immediately if they occur. The most commonly discussed complications directly related to lumbar spinal fusion include infection, dural tears, pseudoarthrosis, and adjacent segment degeneration.
The most commonly discussed complications directly related to lumbar spinal fusion include infection, dural tears, pseudoarthrosis, and adjacent segment degeneration. Rarer, more serious complications associated with lumbar spinal fusion include nerve root injury, paralysis, massive blood loss, blindness, heart attack, stroke, and death.
Rarer, more serious complications associated with lumbar spinal fusion include nerve root injury, paralysis, massive blood loss, blindness, heart attack, stroke, and death. Careful patient selection, meticulous surgical technique, expert intraoperative anesthetic monitoring and care, and extensive postoperative monitoring can significantly decrease many of these complications.
Careful patient selection, meticulous surgical technique, expert intraoperative anesthetic monitoring and care, and extensive postoperative monitoring can significantly decrease many of these complications.Introduction
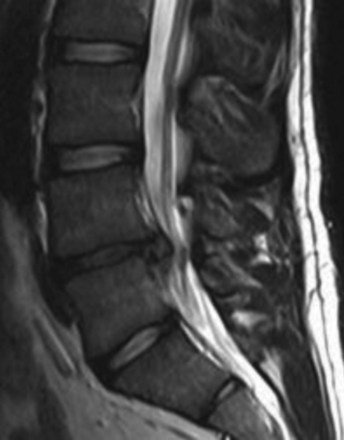
Most lumbar spine surgery involves decompressing the soft tissue, which often includes a herniated disc (Fig. 8-1) or hypertrophied ligamentum flavum. Lumbar spine surgery also involves decompressing the bony elements, which can include hypertrophied facet joints, spinous processes, and lamina that make up the spinal canal. By decompressing both soft and bony tissue, spine surgery can often make patent both central and neuroforaminal narrowing that may be impinging on the spinal cord or nerve roots. Thoroughly decompressing the stenosis and nerve roots can reliably relieve leg pain and its associated symptoms of numbness and weakness. However, there are instances wherein there is obvious instability, spinal spondylolisthesis (Fig. 8-2), or the potential for instability. In this situation, a surgeon must consider both decompressing the stenosis along with stabilizing the affected spinal segments.
Selected Complications
Infection
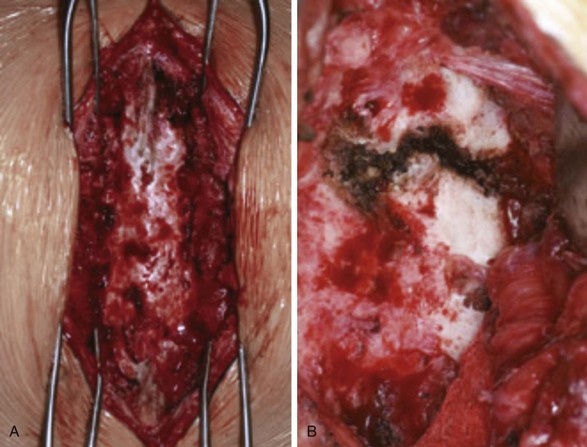
Patients undergoing lumbar spinal fusion typically receive prophylactic intravenous (IV) antibiotics within 1 hour of surgery and postoperatively in several doses. This perioperative regimen, along with proper intraoperative sterility, has decreased infection rates dramatically. However, postoperative spinal wound infection is not an uncommon complication (Fig. 8-3). If not properly recognized and treated, a wound infection can be devastating and affect the ultimate desired surgical outcome.
A review of the literature shows that postoperative wound infections are common and range from 1% to 6% after lumbar spine fusions.1 Staphylococcus aureus was the most common pathogen cultured, but some patients have multiple organisms causing an infection. Multiple studies have assessed risk factors for postoperative wound infections (Table 8-1).
Table 8-1 Patient and Surgical Risk Factors for Postoperative Wound Infections
| Patient Risk Factors for Postoperative Wound Infections | Surgical Risk Factors for Postoperative Wound Infections |
|---|---|
| >60 years of age | Complex spine procedures |
| Smoking | Fusing multiple levels |
| Diabetes | Spinal revisions |
| History of previous surgical infections | Anterior or posterior reconstruction |
| Obesity and increased body mass index | Increased operative times |
| Alcohol abuse |
Age greater than 60 years, smoking, diabetes, previous surgical infection, increased body mass index, and alcohol abuse were statistically significant risk factors. In addition to these factors, more complex spine procedures that involved multiple levels being fused, tumors, surgical revisions, and anterior or posterior reconstructions, also increased the rates of postoperative infections and complications.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree