Chapter 14 Complications of Facet Joint Injections and Medial Branch Blocks
 Appropriate Accreditation Council for Graduate Medical Education mentored subspecialty training in interventional pain management is vital to ensure patient-centered care.
Appropriate Accreditation Council for Graduate Medical Education mentored subspecialty training in interventional pain management is vital to ensure patient-centered care. A thorough understanding of the spinal anatomy is vital to procedural success. Extrapolation of three-dimensional needle placement using two-dimensional ultrasound and fluoroscopic guidance is crucial for accurate needle placement.
A thorough understanding of the spinal anatomy is vital to procedural success. Extrapolation of three-dimensional needle placement using two-dimensional ultrasound and fluoroscopic guidance is crucial for accurate needle placement. Although uncommon, devastating complications from facetogenic intraarticular or median branch injections have been reported.
Although uncommon, devastating complications from facetogenic intraarticular or median branch injections have been reported. Infectious complications can be severe, and diagnosis centers on a high index of suspicion, initiation of intravenous antibiotic therapy, and prompt neurosurgical consultation for neurologic deterioration for decompression.
Infectious complications can be severe, and diagnosis centers on a high index of suspicion, initiation of intravenous antibiotic therapy, and prompt neurosurgical consultation for neurologic deterioration for decompression.Introduction
Facetogenic sources of pain are common, accounting for approximately 40% of thoracic and cervical complaints and 30% of lumbar pain.1–7 These are disorders of older adults; 89.2% of people 60 to 69 years of age have facet joint arthropathy,8 but there is little correlation in the cervical and thoracic regions. Predicatively, facetogenic interventions are the second most commonly used and gratifying procedures performed by pain management physicians in the United States because they are relatively easy to perform with reliable radiographic landmarks, very good outcomes, and reported complications described to occur very rarely.
In a recent guideline statement, the American Society of Interventional Pain Physicians did not recommend intraarticular injections for either diagnostic or therapeutic benefit (level III evidence).9 The International Spine Intervention Society described thoracic intraarticular injections as emerging procedures and did not provide any comments on the cervical or lumbar level.10 The American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia (ASRA) and Pain Medicine reported that randomized placebo controlled trials demonstrated equivocal evidence supporting intraarticular injections, and although observational studies provided evidence for short-term pain relief, they summarily described the evidence as “may be used for symptomatic relief of facet-mediated pain.”11 Both guidelines suggest better evidence (level I or II) with median branch injections for diagnostic and therapeutic benefit using 80% pain reduction with two comparative controlled diagnostic blocks, and based on Guyatt et al’s12 criteria, IB recommendations for radiofrequency (RF) neurotomy.9
Despite appropriate care, significant and devastating complications have been described as scattered case reports, including radicular artery injury and epidural abscesses (Box 14-1).
Selected Complications
Vascular Injury
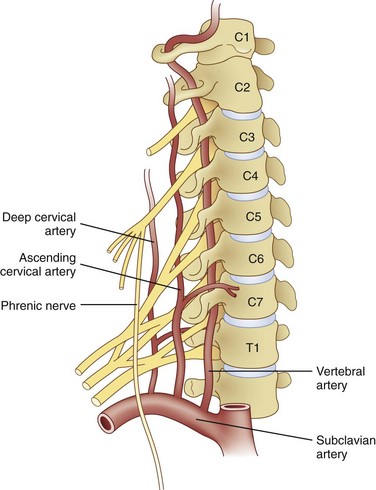
Huntoon13 investigated cervical blood flow in a cadaveric study and noted that the ascending and deep cervical arterial branches may contribute significantly to the anterior segmental arteries, and anterior spinal artery flow may be susceptible to injury during interventional procedures (Fig. 14-1). There have been unpublished reports of quadriplegia from vascular occlusion by particulate steroid after attempted cervical zygapophyseal interventions. Despite well-described lateral and prone approaches for cervical median branch blocks and rhizotomies, the prone technique hypothetically may be safer because there are more reliable osteal landmarks during needle placement; however, comparative studies are lacking.
Image guidance is required. Tetraplegia was reported in a case using only landmarks to guide needle placement14 and is not advocated. Image guidance, by either ultrasound or fluoroscopic means, is essential.
The most publicized and largest segmental spinal artery is the artery of Adamkiewicz. It is vitally important to reinforce the American Society of Anesthesiologists in the thoracolumbar region. It has a variable anatomic course. The Adamkiewicz artery is typically located between T8 and L3, but it is at T9 or T10 in 50% of people and comes from the left side in 75% of cases. Additional radiculomedullary arteries were found in 43% of patients.15,16
These important reinforcing segmental spinal arteries have variable location segmentally (Fig. 14-2) but consistent intraforaminal anatomy as they course in the superior anterior location of the foramen beneath the pedicle.17 Obviously, inadvertent needle placement can result in injury. Despite well-described lateral and prone approaches for cervical median branch blocks and rhizotomies, the prone technique hypothetically may be safer because there are more reliable osteal landmarks during needle placement; however, comparative studies are lacking.
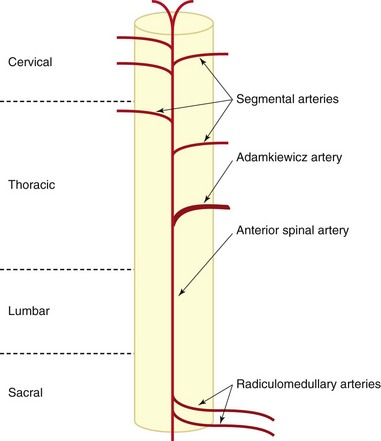
Fig. 14-2 Diagram of spinal cord blood supply.
(Modified from Charles YP, Barbe B Beaujeux R, et al: Relevance of the anatomical location of the Adamkiewicz artery in the spine, Surg Radiol Anat 33(1):3-9, 2010.)
Huntoon13 investigated cervical blood flow in a cadaveric study and noted that the ascending and deep cervical arterial branches may contribute significantly to the anterior segmental arteries. Consequently, the anterior spinal artery flow may be susceptible to injury during interventional procedures. Steroids for spinal interventional procedures are not created equal because homogenicity and potency are variable. Derby et al18 investigated particle size and aggregation frequency of commonly used spinal corticosteroids (Table 14-1). The larger the particle size and the higher the aggregation, the more likely ischemic injury can result from embolic phenomena.
Table 14-1 Particle Size and Aggregation Potential for Commonly Used Corticosteroids for Spinal Injections
| Steroid | Particle Size | Aggregation |
|---|---|---|
| Dexamethasone | 5–10× smaller than RBCs (Fig. 14-3) | None |
| Triamcinolone | Varied in size, often >RBCs (Fig. 14-4) | High aggregation |
| Betamethasone | Varied in size, often >RBCs | High aggregation |
| Methylprednisolone | Uniform size, smaller than RBC | Few aggregations |
RBC, red blood cell.
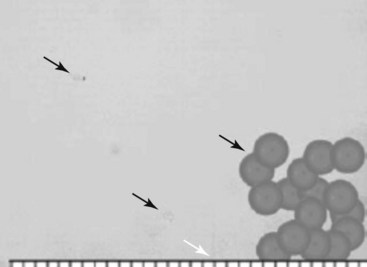
Fig. 14-3 Dexamethasone compared to red blood cells.
(From Derby R, Lee SH, Date ES, et al: Size and aggregation of corticosteroids used for epidural injections, Pain Med 9(2):227-234, 2008.)
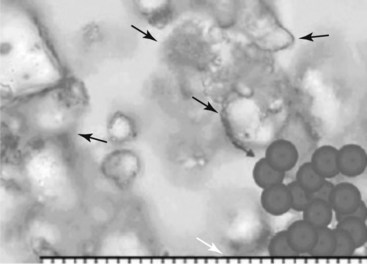
Fig. 14-4 Triamcinolone aggregates compared to red blood cells.
(From Derby R, Lee SH, Date ES, et al: Size and aggregation of corticosteroids used for epidural injections, Pain Med 9(2):227-234, 2008.)
Inadvertent vascular ischemic injury after steroid particulate injection or vascular injury during cervical transforaminal injections.19,20 has become increasingly common, and corollaries should be drawn to facetogenic interventions. There have been unpublished reports of quadriplegia from vascular occlusion by particulate steroid after attempted cervical zygapophyseal interventions.
Furthermore, studies for facet and epidural interventions comparing particulate versus nonparticulate steroids found no statistical difference in efficacy.21 Injection under live fluoroscopy with or without digital subtraction may help elucidate intravascular needle placement.
Local tenderness has been reported in many investigations. Dobrogowsi et al22 investigated strategies to reduce the inflammatory pain associated with the lesioning. In a randomized prospective trial, patients were randomized to intraoperative methylprednisolone (10 mg), pentoxifylline (10 mg), or saline (1 mL). No “severe local tenderness” was reported in either the methylprednisolone group or the pentoxifylline group, with minor tenderness resolving within 1 month, as compared with the saline group, which had four of 15 patients with severe pain at 1 week and one patient for longer than 1 month. Other authors report a 3-day dosage of diclofenac to be effective in reducing procedural pain after conventional RF neurotomy of lumbar median branches.23
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree