Definition of terms
In the past complementary therapies were described as “unconventional therapies” rarely used by orthodox medical professionals. Now, with increased use and understanding of these therapies, the term “complementary” has been adopted to indicate therapies that can work alongside and in conjunction with orthodox medical treatment. The term “integrated health care” is also used to describe the provision of orthodox and complementary treatments side by side as a package of care.
The term “alternative therapies” indicates therapies used instead of orthodox medical treatments (BMA, 1993). In the US, the former office of alternative medicine of the National Institutes of Health coined the term “complementary and alternative medicine,” or CAM, to encompass both approaches. This term includes a much broader spectrum of medical and therapeutic approaches to those used in palliative care.
In the context of palliative care, we have used the term “complementary” to refer to those therapies that are used alongside conventional health care.
Classification
Therapies can be classified in various ways. They may be grouped by whether they have a direct physical application (such as massage), a primarily psychological effect (such as visualisation), or whether they purport to have a pharmacological basis (such as dietary supplements). They can also be classified by application— that is, they can be thought of as a complete system of care (such as homoeopathy), as useful techniques (such as aromatherapy), or as approaches to self help (such as meditation). More recently, the House of Lords select committee report provided a classification, grouping therapies according to their professional regulation and evidence base.
In palliative care, patterns of provision vary widely. Therapies may be offered by individual practitioners based in the hospital or community or in a designated setting where several practitioners offer a wider range of therapies with a more comprehensive package of care. This may be within a hospital or hospice or in a separate location often set up by voluntary organisations or self help and support groups.
Patterns of use
The use of complementary therapies in palliative care is considerable and growing. Use by adults with cancer has been estimated as between 7% and 64%. Users are likely to be younger, female, and have higher education levels, income, and social class. Use is also associated with progression of the disease, attendance at support groups, and previous use.
Provision of therapies is mainly in hospices and hospitals. Those most commonly on offer to patients are:
- Touch therapies, such as aromatherapy, reflexology, and massage
- Mind-body therapies such as relaxation and visualisation
- Acupuncture
- Healing and energy work, such as reiki, spiritual healing, and therapeutic touch
- Nutritional and medicinal therapies, such as vitamins and dietary supplements, homoeopathy, and herbal remedies.
Disciplines in complementary and alternative medicine (as grouped by the House of Lords Science and Technology Select Committee 6th Report, November 2000)
| Group 1— professionally organised alternative therapies | Group 2— complementary therapies | Group 3—alternative disciplines |
| Acupuncture* | Alexander technique | 3a: Long established |
| Chiropractic | Aromatherapy* | traditional systems of |
| Herbal medicine | Bach and other flower | health care |
| (includes essiac*) | remedies | Anthroposophical |
| Homoeopathy* | Bodywork therapies | medicine (includes |
| Osteopathy | including massage* | iscador*) |
| Counselling stress | Ayurvedic medicine | |
| therapy* | Chinese herbal medicine* | |
| Hypnotherapy* | Eastern medicine | |
| Reflexology* | Traditional Chinese medicine | |
| Meditation* | Naturopathy medicine | |
| Shiatsu* | ||
| Healing* | 3b: Other alternative | |
| Marharishi ayurvedic | disciplines | |
| medicine | Crystal therapy | |
| Nutritional medicine* | Dowsing | |
| Yoga* | Iridology Kinesiology |
*Therapies commonly used in palliative care.
The Lynda Jackson Macmillan Centre at the Mount Vernon Cancer Centre provides a drop-in information and support service. Appointments can be made for complementary therapies, counselling, relaxation sessions, educational sessions, and advice on benefits (photo reproduced with permission)

These services are often extended to both carers and staff and, encouragingly, most are free of charge.
The role of complementary therapies
The role of complementary therapies in palliative care is presently undefined. Three basic models of how therapies might be used have been proposed. These are the
- Humanistic model, where the aim is to provide a supportive role by relieving symptoms, side effects of treatment, and improving quality of life
- Holistic model, where the aim is to empower the user by giving patients greater control over their health and quality of life
- Radical holistic model, where self healing is the proposed aim and patients seek increased survival and possible cure.
Considerable overlap may exist between the models—for example, patients may be given a treatment as a support and find it empowering. The radical model is usually advocated outside the NHS setting as an alternative to orthodox treatment.
Why do patients seek complementary therapies?
Knowing why patients seek therapies is fundamental in evaluating their use. Possible factors “pushing” patients away from orthodox medicine and those “pulling” them towards complementary therapies can be identified. The provision of “touch, talk, and time” and a “healing” environment seem to be particularly important.
In 2002 the Department of Health commissioned further research into the use of therapies from diagnosis through to palliative and terminal care. Drivers for use, perceived benefits, and comparisons with orthodox medical care are also being evaluated.
Referral and assessment
Referral
Patients and carers should be able to self refer or have a family member or health professional refer them for assessment for complementary therapies.
All healthcare professionals working in palliative care are advised to be familiar with complementary therapies and, when appropriate, refer patients to further sources of information and services. Referral criteria are useful if health professionals are making referrals. They may also help to guide patients when they are self referring. When possible, it is recommended that there is a designated facilitator or coordinator to ensure continuity of care and to offer patients information to make their own informed choice of treatment.
Assessment
The assessment
Assessment ranges in different settings from screening for contraindications to a full assessment of physical, psychological, emotional, and spiritual factors affecting the patient. Contraindications and precautions for use of individual therapies should also be discussed.
Contraindications and precautions
Many questions arise in the treatment of patients with serious illness and widespread disease. For example, a question often asked, and an issue where confusion arises, is whether massage spreads cancer. Based on current evidence, cancer is not a contraindication to receiving gentle massage, though massage therapists are advised to be cautious over tumour sites.
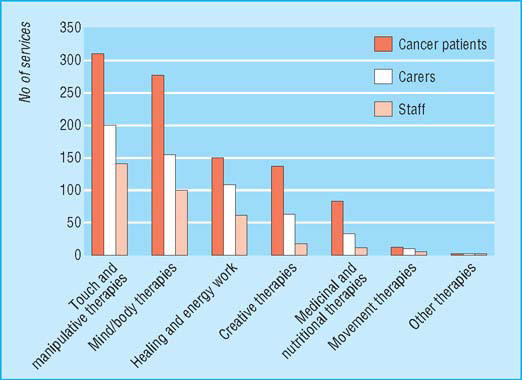
Number of services in the UK offering various complementary therapies to patients with cancer, their carers, and staff (Macmillan Directory 2002)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








