Introduction
The use of complementary and alternative therapies in the management of pain pre-dates many of the more conventional therapies described in this book. Nevertheless, their use within health services remains relatively limited due both to some scepticism regarding their effectiveness and to limited availability of healthcare resources. Space is too limited to debate the efficacy of these treatments. Therefore, this chapter concentrates on a brief overview of the aims, techniques and availability of three treatments–acupuncture, hypnotherapy and aromatherapy.
Who Should Deliver the Treatment?
A variety of healthcare professionals may deliver these treatments and in some areas volunteers may also be involved. Regulation of those delivering complementary and alternative therapies remains rather problematic. There are guidelines from different healthcare providers on the delivery of complementary and alternative therapies and these should be consulted where they exist. Clearly, healthcare professionals must adhere to all requirements set out by their own statutory regulatory bodies and, in addition, must receive appropriate training in their particular therapy and must abide by the standards and guidelines of the association or regulatory body that oversees that therapy. Websites (with extensive additional information for both professionals and patients) for some of the relevant professional associations and the disciplines they represent are in Box 19.1.
As with any other medical intervention, patients receiving any complementary or alternative therapy must receive a full explanation of what is involved and give formal consent. The therapist must keep an accurate record of all treatments and outcomes. Within the pain clinic context these notes are usually kept as part of the multidisciplinary record.
Acupuncture
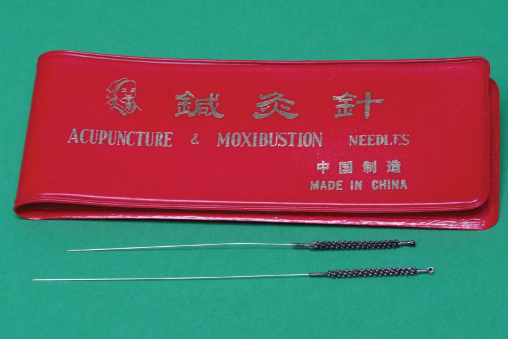
In pain management services most acupuncture treatment is delivered by healthcare professionals (usually doctors, nurses or physiotherapists) who have additional training in acupuncture techniques but who work within the diagnostic and management parameters of conventional Western medicine, using needling techniques based on conventional understanding of the neurophysiology of pain. This contrasts with practitioners of Traditional Chinese Medicine, who use acupuncture techniques based on an ancient complex Chinese philosophical system that envisages ‘Qi’ or energy running through meridians and a requirement to balance Yin and Yang (Figure 19.1).
Acupuncture is probably the commonest complementary therapy offered in chronic pain clinics. In addition, it is widely available from physiotherapists for the management of more acute musculoskeletal pains, usually to allow the patient to engage more fully with other physiotherapy interventions. On a more intermittent basis, acupuncture is also provided in primary care by a small number of enthusiastic general practitioners and some nurses.
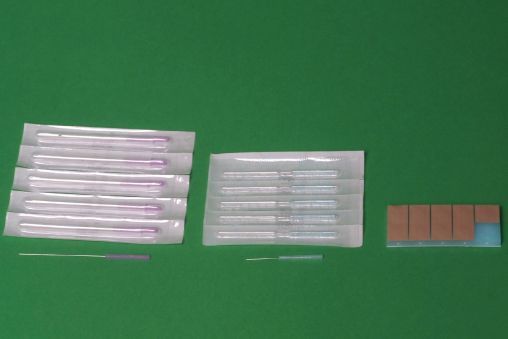
As with any other therapeutic intervention, acupuncture for pain management should be delivered after appropriate investigations have been carried out and a diagnosis made (even if this is simply a diagnosis of exclusion). Patients are typically offered a trial block of 3 to 6 weekly treatments in the first instance. Side effects are usually minimal and may include fatigue, bruising, rarely allergy to the needles and occasionally a worsening of symptomatology. Modern acupuncture needles are single use and pre-sterilised, as with any other medical needle (Figure 19.2). Needles are ‘stimulated’ either by manual rotation by the therapist or by electro-acupuncture. Depth of insertion depends on both the type of needling chosen and, more importantly, the anatomy of the area to be treated. Serious adverse events reported after acupuncture are rare but include cardiac tamponade and pneumothorax.
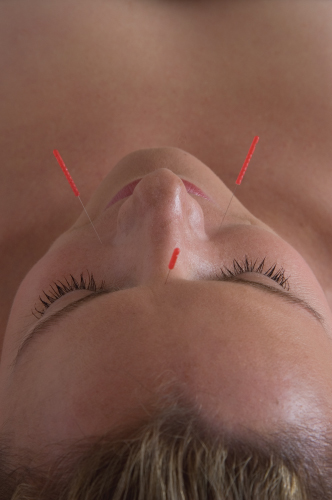
Patients with a variety of musculoskeletal pains, including low back pain, neck pain and osteo-arthritic knee pain, are all suitable candidates for a trial of acupuncture. Patients with chronic headache and facial pain may also respond well (Figure 19.3). Significant needle phobia, known allergy to needles and infection in the area to be treated are all contraindications to treatment. Anticoagulant therapy is not an absolute contraindication as long as extra consideration is given to anatomical considerations and depth of needling.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree