CHAPTER 16 COMMON PREHOSPITAL COMPLICATIONS AND PITFALLS IN THE TRAUMA PATIENT
The evolution of prehospital care in this country has an interesting and continually evolving record. Although there is recorded history of wagons and carts being used to transport the sick and injured as early as 900 ACE, the term “ambulance” was not used until introduced by Queen Isabella of Spain in the early 15th century. Even at that time, it referred more to military field hospitals and tents for the wounded than to a means of transporting wounded and dead from battlefields. Not until the time of Baron Larrey would the term “ambulance” take up its more current meaning of “a specially equipped motor vehicle, airplane, or ship for carrying sick or injured people, usually to a hospital.”1
One of the prime factors identified as contributing to the continued reduction in battlefield casualties from 8% in World War I to less than 2% in the Vietnam War was reducing the time from injury to initiation of medical care. On this backdrop, the mid-1960s and early 1970s sought to improve prehospital care, education, equipment, and processes. The early 1960s called for an extension of basic and advanced first aid training to greater numbers of the lay population, and preparation of nationally accepted texts, training aids, and courses of instruction for rescue squad personnel, policemen, firefighters, and ambulance attendants.2 Ambulance services in the 1960s was very piecemeal and adequate at best. In a few major cities, there were specially equipped ambulances prepared to care for the injured and sick, and trained professional prehospital personnel were available. However, approximately 50% of the country’s ambulance services at that time were provided by over 12,000 morticians mainly because their vehicles were able to accommodate transportation of patients on gurneys or stretchers.
In the mid-1960s, the National Traffic and Motor Safety Act and the Highway Safety Act3 provided for the establishment of national standards for used motor vehicles, motor vehicle inspections, and emergency services. Communications were also problematic. At a time when the United States had just placed a man on the moon, it was easier in most instances to communicate with that extraterrestrial individual than it was for prehospital providers to communicate with the emergency department where they were headed.
Over the next several decades, the education and provision of specifically equipped vehicles progressed until the mid-1980s when Injury in America: a Continuing Public Health Problem was published.4 Although the report found that there had been significant progress in the credentialing and education of prehospital care providers, more than 2.5 million Americans died from injuries in the 1966–1985 period. This prompted the expenditure of more federal dollars to study the continuing public health problem, as the report noted and called for the institution of more systems of communication and transportation of the injured to facilities specially equipped for managing critically injured patients.
In 1992, the Model of Trauma Care Systems Plan, developed by Health Resources and Services Administration under the Authority of the Trauma Systems Planning and Development Act of 1990,5 marked the next major step in the evolution of health policy related to trauma care. This plan emphasized the need for a fully inclusive trauma care system that involved not only trauma centers, but also all health care facilities according to availability of trauma resources, including prehospital providers. As a result, the numbers of dedicated trauma centers and state trauma systems developed, although at a still less-than-adequate pace. Trauma centers were charged with becoming resource facilities for emergency medical response agencies. Educational programs such as Prehospital Trauma Life Support (PHTLS), Basic Trauma Life Support (BTLS), and others were developed with states being empowered to license and credential prehospital providers at various levels.
INCIDENCE
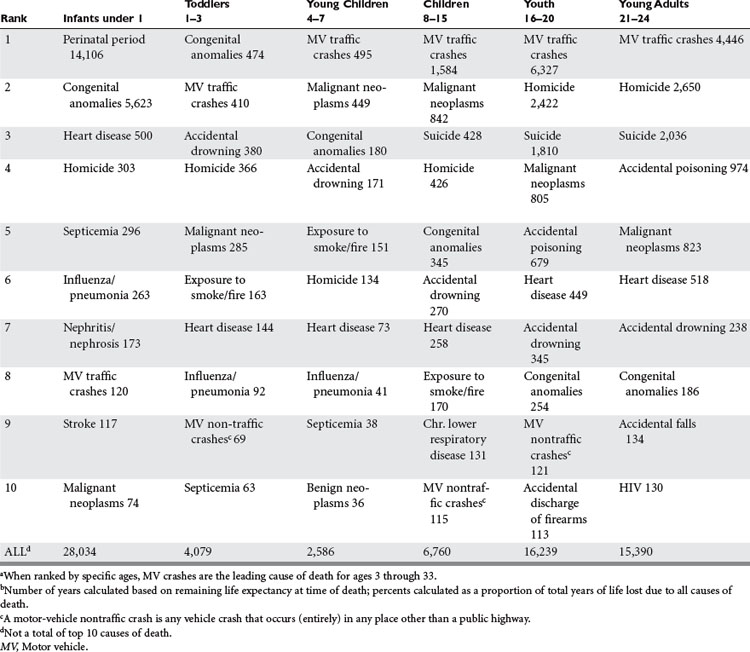
According to the National Highway Traffic Safety Administration, the leading cause of death in the United States in 2002 for people aged 4–34 is overwhelmingly motor vehicle traffic crashes (Table 1). In terms of years of life lost, motor vehicle crashes ranks third, after malignant neoplasms and heart disease, at 5% of total years of life lost for the entire population.
The foundation of Advanced Trauma Life Support® of the American College of Surgeons6 stresses an ABC (airway, breathing, and circulation) approach. Much of the emphasis on prehospital care and subsequent care involves appropriate management of the airway, providing for ventilation by breathing for the patient, and control of circulation consisting of hemorrhage control and restoration of intravascular volume. Not surprisingly, the most common prehospital complications occur in these three areas.
AIRWAY
Ensuring that the trauma victim has a patent airway is the highest management priority.7 If manual maneuvers (clearing the airway of foreign bodies, jaw thrust, or chin lift) or basic adjuncts (oropharyngeal or nasopharyngeal airways) are not adequate to maintain the airway, then alternate, more invasive methods are required.