Common Mucosal and Luminal Disorders
Kadakkal R. Radhakrishnan
CELIAC DISEASE
Celiac disease, also called gluten-sensitive enteropathy, is a permanent intestinal intolerance to dietary wheat protein gliadin and related proteins. This disorder occurs only in genetically susceptible individuals.
Epidemiology
In the United States, the incidence of celiac disease using persistent IgA transglutaminase positivity is 1 per 104 individuals and 1 per 105 individuals when IgA anti-endomysial antibodies are used to detect this disorder. In Sweden, the incidence ranges from 1 per 77 individuals to 1 per 285 individuals. In Finland the incidence of biopsy proven celiac disease is 1 per 99 individuals. Celiac disease is generally uncommon in Asia and Africa, although the highest incidence of celiac disease by serological methods was reported in sub-Saharan Africa at 1 per 60 individuals.
Pathogenesis
The pathogenesis of celiac disease is thought to be dependent on three components (Fig. 9.1):
Genetic susceptibility (HLA DQ-2 and DQ-8 are seen in over 90% of individuals with celiac disease, but these same genes are also present in 30% of whites who do not have celiac disease).
Exposure to incriminating proteins, especially gliadin
T-cell-mediated inflammatory response in the small bowel, causing inflammation and mucosal change in genetically susceptible individuals
Dietary Factors
The three main cereals that are implicated in celiac disease fall under the tribe Triticeae. They include:
Wheat (Gliadin)
Barley (Hordein)
Rye (Secalin)
Oats, which are considered part of the Avenae tribe, rarely activates celiac disease, playing a role in a small fraction of patients. All these proteins are structurally similar, with the last 33 amino acids being resistant to digestion. This amino acid sequence is believed to be the inflammation-stimulating sequence.
Clinical Manifestations
The classic manifestations of celiac disease include:
Failure to thrive
Loose stools and/or diarrhea
However, a more common presentation of celiac disease is an asymptomatic patient who is incidentally identified by serologic screening. Refractory iron deficiency in adults is a common manifestation of celiac disease. Uncommon presentations of celiac disease include constipation, osteoporosis, fat-soluble vitamin deficiency, elevation in transaminases, depression, and dermatitis herpetiformis.
Diagnosis
Definitive diagnosis is established by endoscopy and small bowel biopsy in the appropriate clinical setting. Changes in the small bowel include subtotal to total villous atrophy and increased round cell infiltration.
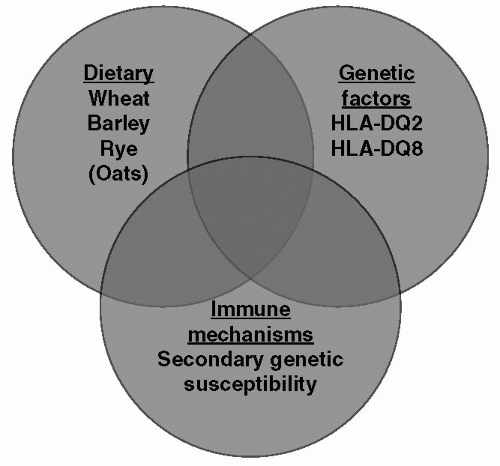 Figure 9.1 Schematic showing the relationship between the three components thought to be important in the pathogenesis of celiac disease. |
Serologic methods of diagnosis include:
Tissue transglutaminase (TTG) IgA: sensitivity >90% and specificity >95%
Anti-endomysial antibody IgA: sensitivity >95% and specificity >98%
Gliadin IgG and IgA antibodies: relatively high false positivity rate (low specificity)
Measurement of total IgA levels is recommended when screening for celiac disease, given the high incidence of IgA deficiency in the general population.
It is important to remember other entities that cause villous atrophy, including:
Severe Crohn disease
Cell-mediated, congenital, and acquired immune deficiency states
Radiation enteritis
Severe cow milk protein allergy
Giardia infection
Treatment
The definitive treatment for celiac disease is complete and lifelong institution of a gluten-free diet. Patients are advised not to share cooking utensils to avoid the risk of contamination. Follow-up serologic studies of endomysial antibody are recommended, preferably every 6 months, to evaluate the response to diet and compliance. Oats may be reintroduced after 6 months of a strict gluten-free diet. Patient with celiac disease should have a complete blood count and metabolic panels an annual basis, and bone densities should be performed every 2 to 3 years after the age of 10 years.
Celiac disease is associated with other disorders, including:
Type 1 diabetes (7% of patients have celiac disease)
Down syndrome (up to 7% have celiac disease)
Hypothyroidism (20% of patients with celiac disease may have hypothyroidism)
T-cell lymphoma of the gut (relative risk is 3 in patients with celiac disease)
CYSTIC FIBROSIS AND GASTROINTESTINAL SYSTEM
Cystic fibrosis (CF) is the most common genetic disease affecting the pancreas. The prevalence of CF is 1 per 2500 whites, 1 per 15,000 African Americans, and 1 per 100,000 Asians.
Pathogenesis
CF is caused by mutations affecting the cystic fibrosis transmembrane regulator (CFTR) gene. Over 1400 mutations have been reported in the CFTR gene but only 10 of these cause 90% of the disease. Homozygous delta 508 is the most common mutation, and this accounts for 70% of the disease. Ninety-nine percent of children with homozygous delta 508 mutations have pancreatic insufficiency by 1 year of age. Seventy percent of compound delta 508 mutations have pancreatic insufficiency by one year of age.
Pancreatic Insufficiency
Patients with untreated CF often have greasy stools because of fat malabsorption. Severe malabsorption may lead to failure to thrive and hypoalbuminemia. Fat-soluble vitamin deficiencies and their consequences in CF include:
Vitamin E: Hemolysis and ataxia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





