CP122, 7211 200 mg (52)
O 4 mg + CP122, 721 200 mg (53)
96
98
6
4
Vomiting:
CP122, 721 = O + CP122, 721 > O
O 4 mg IV + C 50 mg PO (235)
10.3
68.7
O + C > O
O 4 mg IV + C 50 mg PO (135)
O 4 mg IV + C 100 mg PO (130)
O 4 mg IV + C 150 mg PO (128)
C 150 mg PO (126)
70
63.6
66.4
72.5
9.3
4.3
7.1
7
59.3
62.1
60.7
50
Vomiting and CR:
all O + C groups > O
O 4 mg IV + A 80 mg PO (28)
O 4 mg IV + A 125 mg PO (24)
82.1
96.1
O 4 mg IV + A 80 mg PO (64)
3.1
42.2
CR: NS
O 4 mg IV + A 40 mg PO (75)
9.3
34.7
CR: NS
R 0.3 mg IV + A 80 mg PO (42)
50
4.7
19.1
Dex 8 mg IV + A 80 mg PO (30)
3
Dex + A > Dex
A 40 mg PO + TDS 1.5 mg (58)
45
8.6
57
A, aprepitant; C, casopitant; CR, complete response; Dex, dexamethasone; IV, intravenous; NS, no statistically significant differences; O, ondansetron; PO, oral; R, ramosetron; TDS, transdermal scopolamine; >, statistically significant difference. Data are 24-h data unless studies reported data at other time points not including 24 h.
Other combinations
Lee et al. evaluated the combination of TDS with intravenous dexamethasone in patients receiving patient-controlled epidural analgesia after major orthopedic surgery, and reported that the combination was more effective in preventing PONV than dexamethasone alone or dexamethasone plus ramosetron[42]. The combination of cyclizine 50 mg and ondansetron 4 mg was more effective than ondansetron alone in preventing PONV in women undergoing ambulatory gynecologic surgery[43]. Khalil et al. compared the combination of ondansetron 2 mg and promethazine 12.5 mg with ondansetron 4 mg, promethazine 25 mg or placebo in 87 patients scheduled for middle ear surgery[44]. During the 24-h postoperative period, the incidence of PONV was lower in the combination (29%) and promethazine (39%) groups compared with the placebo group (74%). Whilst the incidence of PONV in the ondansetron group (48%) was higher than the combination group, the difference was not statistically significant since the study was not powered to detect differences between the combination group and single agent group, which is also the case in many other published studies comparing combination therapy versus the two active agents and placebo. Gan et al. compared the combination of promethazine 6.25 mg with granisetron 0.1 mg versus each agent alone in women undergoing outpatient laparoscopy[45]. Prophylaxis with oral promethazine 12.5 mg, granisetron 1 mg or both was started in the respective groups 12 h after the end of surgery and continued every 12 h until postoperative day 3. Patients in the combination group had a higher total response rate (no PONV and no rescue) at 6, 24, 48 and 72 h after surgery compared with those who received promethazine alone (at 24 h combination 69.6%, promethazine 36.2%, granisetron 53.3%; P = 0.0079). The maximum nausea scores were also lower in the combination group compared to both single-agent groups.
Combination of more than two antiemetics and the multimodal approach for PONV prophylaxis
The concept of the multimodal approach involves the use of strategies to minimize the baseline risk of PONV in addition to using combination antiemetic therapy. Scuderi et al. investigated a multimodal approach to the management of PONV in female patients undergoing outpatient laparoscopy[46]. Their multimodal algorithm consisted of total intravenous anesthesia (TIVA) with propofol and remifentanil, no nitrous oxide, no neuromuscular blockade, aggressive intravenous hydration, triple prophylactic antiemetics (ondansetron 1 mg, droperidol 0.625 mg and dexamethasone 10 mg) and ketorolac 30 mg. Control groups included inhaled anesthetic, nitrous oxide, fentanyl and muscle relaxation with neostigmine reversal with or without 4 mg ondansetron prophylaxis. Complete response rate (no PONV and no rescue) in the postanesthesia care unit occurred in 98% of patients in the multimodal group compared with 76% in the ondansetron group and 59% in the placebo group (P < 0.0001). Readiness to discharge was also sooner in the multimodal group (P < 0.001). Habib et al. also found that a multimodal approach incorporating TIVA with propofol combined with ondansetron 4 mg and droperidol 0.625 mg, together with ketorolac and local anesthetic infiltration, was more effective than the combination of the two antiemetics alone or TIVA alone in achieving a complete response (no PONV and no rescue) at 24 h following laparoscopic cholecystectomy (80%, 63% and 43%, respectively)[47]. The contribution of each component to the antiemetic effect, however, was not assessed in those studies. In a multicenter study of factorial design involving 5,161 patients with at least two of the four Apfel risk factors, a multimodal approach was assessed involving three antiemetic interventions (ondansetron 4 mg, droperidol 1.25 mg and dexamethasone 4 mg) and three anesthetic interventions (TIVA with propofol, omission of nitrous oxide and use of remifentanil for intraoperative analgesia); the antiemetic efficacy of various combinations of those interventions was evaluated[5]. The incidence of PONV was 17% in patients who received all six interventions compared to 59% in those who did not receive any of those interventions. The progressive reduction in the risk of PONV with each added intervention is shown in Figure 11.1[5]. Each antiemetic reduced the incidence of PONV by 26%, TIVA with propofol reduced it by 19% and omission of nitrous oxide reduced it by 12%. The use of remifentanil intraoperatively instead of fentanyl did not confer any additional benefit. The interaction between those interventions was additive and not synergistic.
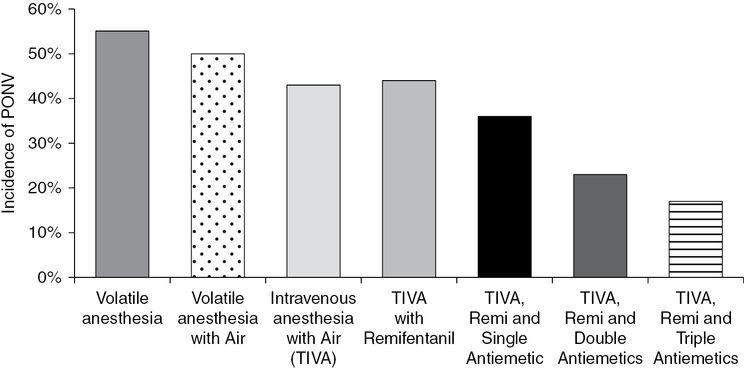
Incidence of postoperative nausea and vomiting (PONV) with various combinations of anesthetic –omission of nitrous oxide (air), use of total intravenous anesthesia (TIVA) with propofol and use of remifentanil (remi) – and antiemetic interventions (single, double or triple antiemetics of the following: ondansetron 4 mg, droperidol 1.25 mg and dexamethasone 4 mg).
Comparison between different antiemetic combinations
There are relatively few studies comparing the efficacy of different antiemetic combinations. This is partly due to the fact that a large sample size is needed to demonstrate differences between different antiemetic combinations. In a meta-analysis involving 3,447 patients, Habib et al. reported no difference in antiemetic efficacy between the combination of 5-HT3receptor antagonists with droperidol and their combination with dexamethasone[16]. Similarly, Apfel et al. reported no difference in antiemetic efficacy between three combinations: ondansetron 4 mg with dexamethasone 4 mg, ondansetron 4 mg with droperidol 1.25 mg and dexamethasone 4 mg with droperidol 1.25 mg[5]. Gan et al. reported that low-dose granisetron 0.1 mg plus dexamethasone 8 mg was as effective as ondansetron 4 mg plus dexamethasone 8 mg IV in women undergoing abdominal hysterectomy[48].
Side effects of combination antiemetic therapy
Studies have reported no increased risk of side effects when using combination antiemetic therapy compared with single-agent prophylaxis. A meta-analysis involving 3440 patients reported no increase in side effects with the combination of 5-HT3 receptor antagonists with dexamethasone or droperidol compared to monotherapy, except for an increased risk of headache with the combination of 5-HT3 receptor antagonists with dexamethasone compared to dexamethasone alone (odds ratio (OR), 1.75; 95% confidence interval (CI), 1.01–3.03)[49]. The combination of 5-HT3 receptor antagonists with droperidol was associated with fewer headaches than 5-HT3 receptor antagonists alone (OR, 0.35; 95% CI, 0.18–0.69). Whilst 5-HT3 antagonists and droperidol have been associated with prolongation of the QT interval, there is no significant increase in QT-interval prolongation when these medications are used in combination compared to each agent alone[50,51].
Efficacy of combination therapy for PDNV
In 2003, Gupta et al. performed a meta-analysis assessing the efficacy of monotherapy and combination therapy for the prophylaxis against PDNV. They reported that, compared with placebo, ondansetron reduced the risk of PDNV with an NNT of 14, while the NNT for the combination of ondansetron with another antiemetic was 5[52]. Pan et al. compared single-agent prophylaxis with ondansetron 4 mg versus the combination of ondansetron 4 mg and dexamethasone 8 mg with postdischarge 8 mg ondansetron oral disintegrating tablet administered on the morning of postoperative days 1 and 2[53]. The combination group had a lower incidence of postdischarge nausea (57% versus 20%), and postdischarge vomiting (20% versus 3%) compared with the ondansetron monotherapy group. Quality of recovery scores were also higher in the combination group. Studies on combination antiemetic therapy involving longer-acting antiemetics in the context of PDNV are lacking.
Combination therapy for the treatment of established PONV
Whilst most studies evaluate the efficacy of different antiemetics for PONV prophylaxis, there are few data on the efficacy of these drugs for the treatment of established PONV, particularly with regards to the use of combination therapy. Rusch et al. evaluated the recurrence of PONV over 24 h in 228 patients with established PONV who received rescue with a single agent (dolasetron or haloperidol) alone or with added dexamethasone 8 mg[54]. The addition of dexamethasone significantly reduced PONV recurrence from 51 to 33% (P = 0.005). Ormel et al. evaluated 80 gynecologic day surgery patients with established PONV who were randomized to treatment with triple therapy consisting of ondansetron, droperidol and dexamethasone versus ondansetron and droperidol[55]. There was a significant reduction in PONV in the first 6 h with triple therapy (81.4%) compared with dual therapy regimen (65%, P = 0.04).
Summary
Combination therapy is more effective than single-agent prophylaxis, with no increase in side effects associated with its use. Patients at moderate-to-high risk for PONV benefit most from combination antiemetic prophylaxis and the multimodal approach. Studies of combinations involving newer, longer-acting antiemetics and focusing on PDNV are needed.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





