CHAPTER 105
Clavicle (Collarbone) Fracture
Presentation
The patient has fallen onto his shoulder or, less commonly, an outstretched arm, or has received a direct blow to the clavicle and now presents with anterior shoulder pain. With distal clavicle fractures, patients may complain of pain on the top of the shoulder. There may be deformity of the bone with swelling, abrasion, and/or ecchymosis. This is usually seen in the midclavicle and is exquisitely tender if palpated. The deformity may appear similar to an acromioclavicular (AC) joint separation with distal clavicle fractures, but the tenderness is usually more medial along the clavicle than with AC injuries (see Chapter 96). The affected shoulder may appear slumped inward and downward compared with the contralateral shoulder, and the patient is usually supporting the injured side by holding his arm close to his body. Paresthesias in the distribution of the supraclavicular nerves can occur.
An infant or small child might present not moving the arm after a fall, but examination of the arm will be normal, and only further examination of the clavicle will reveal the actual site of the injury.
What To Do:
 Perform a detailed history and physical examination. A high-energy mechanism of injury should raise the suspicion of associated injuries. A motorcycle collision or fall from a great height should lead to suspicion of ipsilateral rib fractures and/or pulmonary injury. All patients with suspected clavicle fractures should be questioned with respect to any neck pain, numbness or paresthesias, chest pain, or shortness of breath. Palpation of the ribs and assessment of chest excursion are essential. Cervical motion should be full and pain free.
Perform a detailed history and physical examination. A high-energy mechanism of injury should raise the suspicion of associated injuries. A motorcycle collision or fall from a great height should lead to suspicion of ipsilateral rib fractures and/or pulmonary injury. All patients with suspected clavicle fractures should be questioned with respect to any neck pain, numbness or paresthesias, chest pain, or shortness of breath. Palpation of the ribs and assessment of chest excursion are essential. Cervical motion should be full and pain free.
 After completing a musculoskeletal examination, including gentle palpation along the entire length of the clavicle and proximal humerus, evaluate the neurovascular status of the arm.
After completing a musculoskeletal examination, including gentle palpation along the entire length of the clavicle and proximal humerus, evaluate the neurovascular status of the arm.
 Obtain radiographs to rule out or accurately define a suspected clavicle fracture. A simple anteroposterior (AP) view of the clavicle will demonstrate most midclavicle fractures. An acromioclavicular (Zanca) view, which is a 20-degree cephalad view, is normally included. If there is suspicion of glenohumeral joint injury, shoulder radiographs should be added. If there is any shortness of breath, a chest radiograph should be performed. Occasionally, a CT scan can be useful for evaluation of comminution, position of fracture fragments, and, most important, evaluation of a suspected sternoclavicular (SC) joint injury. Fractures or dislocations at the sternal end of the clavicle are often difficult to see on plain radiographs but are well visualized on CT scans.
Obtain radiographs to rule out or accurately define a suspected clavicle fracture. A simple anteroposterior (AP) view of the clavicle will demonstrate most midclavicle fractures. An acromioclavicular (Zanca) view, which is a 20-degree cephalad view, is normally included. If there is suspicion of glenohumeral joint injury, shoulder radiographs should be added. If there is any shortness of breath, a chest radiograph should be performed. Occasionally, a CT scan can be useful for evaluation of comminution, position of fracture fragments, and, most important, evaluation of a suspected sternoclavicular (SC) joint injury. Fractures or dislocations at the sternal end of the clavicle are often difficult to see on plain radiographs but are well visualized on CT scans.
 Obtain orthopedic consultation if there is any evidence of neurovascular compromise. Consultation should also be obtained with open fractures or if there is significant displacement (> 2 cm) between fracture fragments or if the overlying skin is tented and appears to be under tension. Fractures of the distal third of the clavicle medial to the acromioclavicular joint, where the proximal fragment is detached from the coracoclavicular ligaments and is unstable (type II; Figure 105-1), also require orthopedic consultation to consider surgical reduction. Additionally, fractures with complete displacement (displacement greater than one bone width) also need orthopedic consultation.
Obtain orthopedic consultation if there is any evidence of neurovascular compromise. Consultation should also be obtained with open fractures or if there is significant displacement (> 2 cm) between fracture fragments or if the overlying skin is tented and appears to be under tension. Fractures of the distal third of the clavicle medial to the acromioclavicular joint, where the proximal fragment is detached from the coracoclavicular ligaments and is unstable (type II; Figure 105-1), also require orthopedic consultation to consider surgical reduction. Additionally, fractures with complete displacement (displacement greater than one bone width) also need orthopedic consultation.
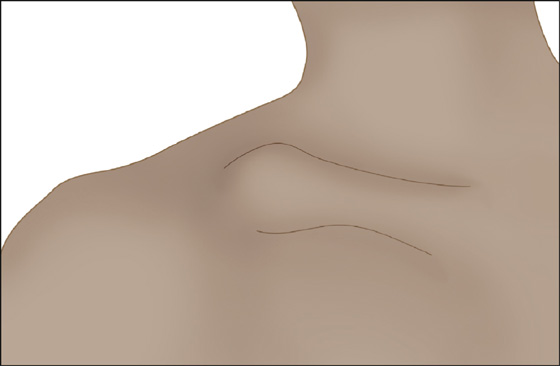
Figure 105-1 Clinical appearance of a type II distal clavicle fracture.
 All uncomplicated fractures can simply be treated with a sling to provide comfort and appropriate immobilization. Rotation at the glenohumeral joint should be encouraged. The sling can be discontinued when the pain is resolved. Passive and active range-of-motion exercises can begin as soon as the patient’s comfort allows.
All uncomplicated fractures can simply be treated with a sling to provide comfort and appropriate immobilization. Rotation at the glenohumeral joint should be encouraged. The sling can be discontinued when the pain is resolved. Passive and active range-of-motion exercises can begin as soon as the patient’s comfort allows.
 Prescribe analgesics, usually acetaminophen or anti-inflammatories such as ibuprofen or naproxen, but generously add narcotics when significant pain is present or anticipated.
Prescribe analgesics, usually acetaminophen or anti-inflammatories such as ibuprofen or naproxen, but generously add narcotics when significant pain is present or anticipated.
 Inform the patient that he may be more comfortable sleeping in a semiupright position, with a sling.
Inform the patient that he may be more comfortable sleeping in a semiupright position, with a sling.
 Arrange for orthopedic follow-up in 1 week to evaluate healing and begin pendulum exercises of the shoulder. Resistive strengthening can commence when the fracture site is nontender and full pain-free motion exists.
Arrange for orthopedic follow-up in 1 week to evaluate healing and begin pendulum exercises of the shoulder. Resistive strengthening can commence when the fracture site is nontender and full pain-free motion exists.
 Contact sports are to be avoided until the fracture appears clinically and radiographically to be healed.
Contact sports are to be avoided until the fracture appears clinically and radiographically to be healed.
 Inform the patient that the bone will likely heal with a noticeable callus (visible lump).
Inform the patient that the bone will likely heal with a noticeable callus (visible lump).
What Not To Do:
 Do not apply a figure-of-eight dressing or a Kenny-Howard–type splint. They are not necessary and often cause greater patient discomfort.
Do not apply a figure-of-eight dressing or a Kenny-Howard–type splint. They are not necessary and often cause greater patient discomfort.
 Do not leave an arm fully immobilized in a sling for more than 7 to 10 days. This can result in loss of range of motion or “frozen shoulder.”
Do not leave an arm fully immobilized in a sling for more than 7 to 10 days. This can result in loss of range of motion or “frozen shoulder.”
Discussion
The clavicle connects the shoulder girdle to the axial skeleton and articulates with the acromion laterally and the sternum medially. Clavicle fractures are classified by the location of the fracture, with the clavicle divided into thirds. Most fractures involve the middle segment of the clavicle (approximately 69%). The distal third of the clavicle is fractured roughly 28% of the time, and the proximal third is the least common site of fracture (about 5%, but in some studies, up to 22%).
Distal clavicle fractures are classified into five categories. A type I distal clavicle fracture is minimally displaced and occurs lateral to the coracoclavicular (CC) ligaments. Type II fractures may be medial to the CC ligaments (IIa) or lateral to the CC ligaments with CC ligament disruption from the proximal fragment (IIb) (Figure 105-2), which in both cases results in the proximal segment being detached from the CC ligaments and, therefore, more prone to distraction of the fracture fragments. Type III distal clavicle fractures extend into the AC joint, type IV involves periosteal sleeve disruption (seen in younger patients), and type V involves an avulsion fracture that leaves only an inferior cortical fragment attached to the CC ligaments and is functionally similar to type II. Only the type II and type V distal clavicle fractures are considered unstable and warrant early orthopedic consultation.
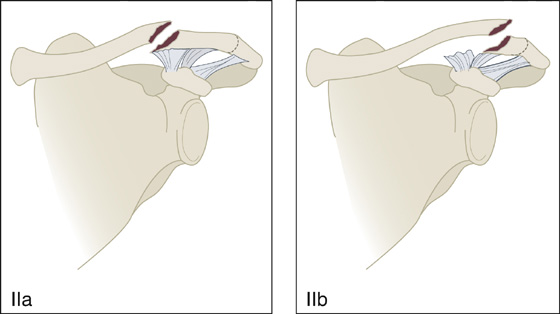
Figure 105-2 Type IIa and IIb clavicle fractures.
The management of type II distal clavicle fractures is controversial. Although many authors advocate a surgical approach, because of the relatively high risk of nonunion (approximately 30%), only a small minority of those nonunions have significant functional limitation.
One approach to surgical intervention in both midclavicular and distal clavicular fractures is to treat marked displacement, high-energy injuries, and potential skin compromise with acute surgical fixation. Otherwise, nonsurgical treatment is selected. With distal clavicle fracture, the patient is counseled about the anticipated 20% to 30% nonunion rate but is also informed of the expectation that the chance for persistent pain or functional loss is low.
Proximal clavicle fractures are the least common but are associated with subluxation or dislocation of the corresponding sternoclavicular (SC) joint. CT scans are far superior to plain radiographs in determining the extent of these injuries. In general, most isolated, minimally displaced, proximal fractures are treated in the same manner as midclavicular fractures. Significant displacement and SC dislocation require rapid orthopedic consultation. Fractures of the proximal clavicle should always prompt a thorough examination to look for other injuries, because approximately 90% have an associated injury.
In children, fracture of the clavicle requires very little force and usually heals rapidly and without complication. In adults, however, this fracture usually results from a greater force and is associated with other injuries and complications. Clavicle fractures are sometimes associated with a hematoma from the subclavian vein. However, other nearby structures, including the carotid artery, brachial plexus, and lung, are usually protected by the underlying anterior scalene muscle as well as the tendency of the sternocleidomastoid muscle to pull up the medial fragment of bone.
A great deal of angulation deformity and distraction on radiographs of midshaft fractures are usually acceptable, because the clavicle mends and reforms itself so well and does not have to support the body in the meantime. As with rib fractures, respiration prevents full immobilization, and therefore the relief that comes with callus formation may be delayed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


