Chronic Kidney Disease, Dialysis, and Renal Transplantation
Vinai Modem
Robert P. Woroniecki
Fangming Lin
Chronic kidney disease (CKD) is a chronic, debilitating condition and has a significant impact on morbidity and mortality (1). The prevalence of and the costs for treating CKD in and out of the pediatric ICU have increased steadily over the past few decades. In this chapter, we will focus on the diagnosis and basic management of CKD for critically ill children in the ICU.
DEFINITION AND RISK FACTORS FOR DEVELOPING CKD
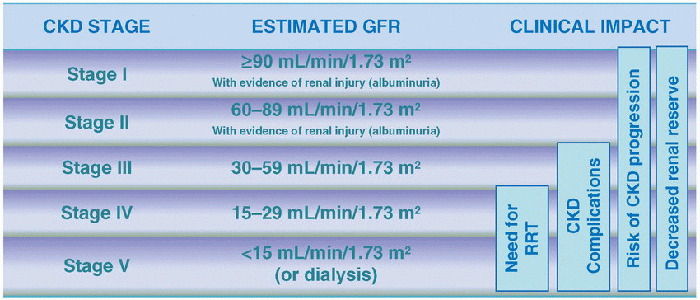
CKD can be diagnosed when there are pathologic abnormalities or markers of kidney damage such as persistent albuminuria (an indicator of ongoing renal injury), or reduced glomerular filtration rate (GFR) <60 mL/min/1.73 m2 for  ≥3 months (2). Chronic kidney condition is classified into five stages on the basis of the estimated GFR (Table 111.1). End-stage renal disease (ESRD) typically refers to stages IV and V, which require renal replacement therapy (RRT) in the form of either chronic dialysis or renal transplantation. Acute kidney injury (AKI) can become CKD when renal injury and dysfunction persist for >3 months. CKD staging can be used for adults and children at 2 years of age or older.
≥3 months (2). Chronic kidney condition is classified into five stages on the basis of the estimated GFR (Table 111.1). End-stage renal disease (ESRD) typically refers to stages IV and V, which require renal replacement therapy (RRT) in the form of either chronic dialysis or renal transplantation. Acute kidney injury (AKI) can become CKD when renal injury and dysfunction persist for >3 months. CKD staging can be used for adults and children at 2 years of age or older.
 ≥3 months (2). Chronic kidney condition is classified into five stages on the basis of the estimated GFR (Table 111.1). End-stage renal disease (ESRD) typically refers to stages IV and V, which require renal replacement therapy (RRT) in the form of either chronic dialysis or renal transplantation. Acute kidney injury (AKI) can become CKD when renal injury and dysfunction persist for >3 months. CKD staging can be used for adults and children at 2 years of age or older.
≥3 months (2). Chronic kidney condition is classified into five stages on the basis of the estimated GFR (Table 111.1). End-stage renal disease (ESRD) typically refers to stages IV and V, which require renal replacement therapy (RRT) in the form of either chronic dialysis or renal transplantation. Acute kidney injury (AKI) can become CKD when renal injury and dysfunction persist for >3 months. CKD staging can be used for adults and children at 2 years of age or older.The prevalence of all stages of CKD has been increasing worldwide (3). In particular, the prevalence of pediatric (0-19 years) ESRD has increased by 32% since 1990. CKD is associated with various comorbidities which could affect ICU outcomes (4). Children with oncologic disease, hematopoietic stem cell transplantation, solid organ transplantation, congenital heart disease, and rheumatologic diseases are at a greater risk for developing CKD. Additional factors contribute to CKD and include repeated insults to the kidney from septic episodes, low cardiac output, and the use of nephrotoxic medications (antibiotics, chemotherapy, and immunosuppressive agents) (5). Patients can also have primary renal disease that progresses to CKD. Common causes of primary renal disease in children include congenital anomalies of the kidney and urinary tract such as aplastic or hypodysplastic kidneys, obstructive uropathy (e.g., posterior urethral valves), and reflux nephropathy. Tubular disease (e.g., nephronophthisis and polycystic kidney disease), glomerular disease due to focal segmental glomerulosclerosis (FSGS), and vasculitis (e.g., lupus nephritis) also contribute to the development of CKD.
CHRONIC KIDNEY DISEASE IN PATIENTS WITH CRITICAL ILLNESS
 Renal dysfunction affects multiple organ systems (Fig. 111.1). The extent and severity of involvement depends on the etiology and stage of CKD (6). CKD stages I and II usually show evidence of renal injury and may have clinical manifestations of proteinuria and hypertension. The primary goal of CKD management for these stages is to prevent the progression by reducing proteinuria and controlling hypertension typically with angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs), which offer renal protection. As renal function deteriorates to stages III, IV, and V, patients will have multiple manifestations involving various organ systems (Fig. 111.1). In addition to slowing down renal disease progression, it is imperative to address these complications. Management focuses on the treatment of electrolyte and acid-base disturbances, anemia, hyperparathyroidism, malnutrition, and behavioral and psychological disorders.
Renal dysfunction affects multiple organ systems (Fig. 111.1). The extent and severity of involvement depends on the etiology and stage of CKD (6). CKD stages I and II usually show evidence of renal injury and may have clinical manifestations of proteinuria and hypertension. The primary goal of CKD management for these stages is to prevent the progression by reducing proteinuria and controlling hypertension typically with angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs), which offer renal protection. As renal function deteriorates to stages III, IV, and V, patients will have multiple manifestations involving various organ systems (Fig. 111.1). In addition to slowing down renal disease progression, it is imperative to address these complications. Management focuses on the treatment of electrolyte and acid-base disturbances, anemia, hyperparathyroidism, malnutrition, and behavioral and psychological disorders.AKI on CKD
Normal kidneys have a significant functional reserve (Fig. 111.2). This reserve is primarily due to hyperfiltration at the level of individual nephrons. If the number of functional nephrons is reduced, this reserve is decreased. The reduction in the functional reserve is proportional to the severity of CKD (7,8). Chronic hyperfiltration can be associated with
hypertension and diabetes and can result in glomerular sclerosis and further loss of nephrons. The CKD kidneys may already be functioning at their maximal capacity. As a result, even mild insults to the kidneys can cause significant deterioration in GFR. Hence, these patients need special attention toward renal protective and supportive care during critical illness (9,10). Frequency and severity of AKI (i.e., need for RRT) increase the risk of CKD progression.
hypertension and diabetes and can result in glomerular sclerosis and further loss of nephrons. The CKD kidneys may already be functioning at their maximal capacity. As a result, even mild insults to the kidneys can cause significant deterioration in GFR. Hence, these patients need special attention toward renal protective and supportive care during critical illness (9,10). Frequency and severity of AKI (i.e., need for RRT) increase the risk of CKD progression.
TABLE 111.1 CHRONIC KIDNEY DISEASE STAGING | |
|---|---|
|
Impact of CKD on the Cardiovascular System
CKD can lead to cardiovascular pathology, including hypertension, vascular wall stiffness, cardiomyopathy, and valvular heart disease (11). These conditions increase the risk of developing congestive heart failure and other cardiac events (dysrhythmias). Vascular complications of hypertension such as posterior-reversible encephalopathy syndrome (PRES) (also called reversible posterior leukoencephalopathy syndrome—RPLS) can occur. In addition to hypertension, uremia, vasculitis, immunosuppressant use, and organ transplant are risk factors for PRES/RPLS that may be seen with CKD or AKI (see also Chapter 64). Rigorous attention to fluid and blood pressure management is essential in children with cardiovascular involvement. Fluid requirements depend on the etiology and severity of CKD




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree