Chest Tube Insertion and Care
Gustavo G. Angaramo
I. GENERAL PRINCIPLES. Chest tube insertion involves the placement of a sterile tube into the pleural space to evacuate air or fluid into a closed collection system to restore negative intrathoracic pressure, promote lung expansion, and prevent lethal levels of pressure from developing in the thorax.
II. ANATOMY AND PHYSIOLOGY OF THE PLEURAL SPACE
A. The pleural space is a closed, serous sac surrounded by two separate layers capped by mesothelial cells, the parietal and visceral pleura. Normally there is a negative intrapleural pressure of 2 to 5 cm of water.
B. The pleural layers are in close apposition and, under normal physiologic conditions, allow free expansion of the lung in a lubricated environment.
III. INDICATIONS
A. Pneumothorax.
1. Accumulation of air in the pleural space is the most common indication for chest tube placement.
2. Diagnosis is often confirmed by chest radiography.
3. The risk of a recurrent ipsilateral spontaneous pneumothorax is as high as 50%, and the risk of recurrence after a second episode is 60% to 80%.
B. Hemothorax.
1. Accumulation of blood in the pleural space can be classified as spontaneous, iatrogenic, neoplastic, infectious, related to thromboembolism, or traumatic.
C. Empyema.
1. Empyemas are pyogenic infections of the pleural space that may result from
a. Necrotizing pneumonia.
b. Septic pulmonary emboli.
c. Spread of intra-abdominal infections.
d. Inadequate drainage of a traumatic hemothorax.
D. Pleural effusion.
1. Treatment of transudative pleural effusions is aimed at controlling the underlying cause. Tube thoracostomy is uncommonly indicated.
2. Exudative effusions, however, often require tube drainage depending on whether the fluid is free or loculated.
IV. CONTRAINDICATIONS
A. There are no absolute contraindications to chest tube insertion.
B. There are many relative contraindications.
1. Anticoagulation.
2. Prior ipsilateral thoracic surgery due to potential adhesions between the lung and the chest wall.
3. Extensive bullous lung disease.
V. PROCEDURE
A. Preparation.
1. Obtain a detailed informed consent.
2. Follow the universal precautions protocol.
3. Sterile technique including maximum barrier precautions is mandatory whether the procedure is performed in the operating room, the intensive care unit, or the emergency room.
4. Careful titration of analgesics or sedatives and injection of local anesthetic to provide optimal pain prevention and management.
5. Standard large-bore drainage tubes are made of either Silastic® or rubber.
a. Rubber tubes elicit more pleural inflammation, have fewer drainage holes, and are not easily identified on chest radiograph.
b. Silastic® chest tubes are either right angled or straight, have multiple holes, and contain a radiopaque stripe with a gap to mark the most proximal drainage holes.
c. Sizes are available from 6 to 40 Fr, with size selection dependent on the type of collection being drained.
B. Technique.
1. To properly insert a chest tube, the following steps are suggested:
a. Examine the chest imaging studies carefully.
b. Gather the necessary equipment.
i. Scalpel.
ii. Kelly clamps.
iii. Suture.
iv. Local anesthesia.
v. Needles.
vi. Syringes, dressings, tape, and a filled drainage apparatus (Pleurevac).
c. Prepare the patient.
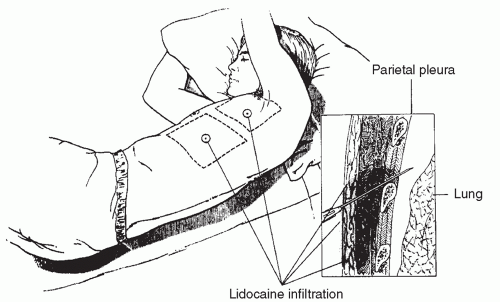
i. Follow the universal precautions protocol. Position the patient with the operative side up, in the lateral decubitus position.
ii. Mark the fourth or fifth intercostal space in the anterior axillary line by landmarks (chest tubes are occasionally inserted anteriorly in the second intercostal space for pneumothoraces only!) (Fig. 7-1).
d. Prepare and drape the surgical site.
i. The area is prepared under sterile conditions with 4% chlorhexidine gluconate.
ii. The area is draped to include the ipsilateral nipple as a landmark.
 Get Clinical Tree app for offline access 
|




