Chest Trauma: Introduction
Immediate Management of Life-Threatening Problems
The ABCs should be addressed as previously outlined in Chapters 9 and 10. There are specific considerations in evaluating the ABCs in the patient with blunt or penetrating chest trauma. The airway can be obstructed at any level from the pharynx to the trachea. Abnormalities in breathing can be caused by one or more of the following mechanisms: (1) impairments in the chest wall or musculature, eg, secondary to pain or because the chest wall motion is not coordinated; (2) impairments in gas exchange, secondary to atelectasis, contusion, or disruption of the respiratory tract; and (3) CNS impairments secondary to drugs or head trauma. Hypoxia is the most important feature of chest injury. Early interventions should attempt to insure that an adequate amount of oxygen is delivered to the portions of the lung capable of normal ventilation and perfusion. Abnormalities in circulation can be caused by blood loss, increased intrapleural pressure, blood in the pericardial sac, vascular disruption, or myocardial dysfunction. Since shock will most often be caused by blood loss, the first step should be to ensure adequate fluid resuscitation.
Immediately Life-Threatening Thoracic Injuries Identified on the Primary Survey
Several entities need to be considered in the patient with chest trauma. They can cause severe hypoxia and/or shock. The diagnoses are made clinically and need to be addressed without waiting for any diagnostic testing. Any patient presenting with any one of these entities should be treated as outlined and admitted to the hospital for further care.
Tension pneumothorax develops when a one-way valve air leak occurs from either the lung or chest wall. Air enters the pleural space but cannot escape, leading to increased intrapleural pressure, collapse of the lung, and shift of the mediastinal contents to the opposite side. Tension pneumothorax can result from blunt chest injury with resultant parenchymal lung injury, but can also be secondary to positive-pressure ventilation. Occasionally a small penetrating wound can cause a valve-like effect that allows air to enter the pleural space on inspiration but not exit on expiration. The collapse of the lung leads to right to left pulmonary shunting and resultant hypoxia. In addition, increased intrathoracic pressure and pressure on the vena cava can reduce venous return to the heart and lead to decreased cardiac output and shock.
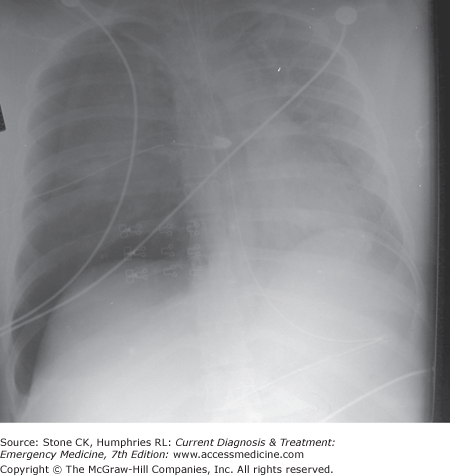
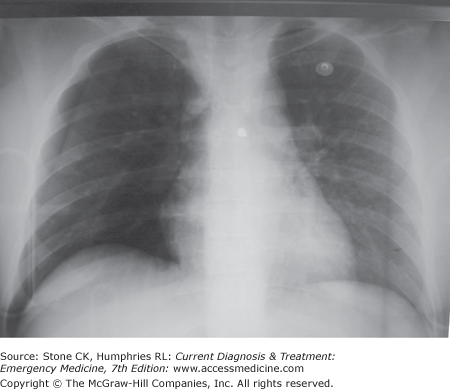
Pneumothorax is characterized by respiratory distress, tachypnea, and hypoxia. There will be hyperresonance to percussion and decreased or absent breath sounds on the affected side. With tension pneumothorax, the trachea will be deviated away from the affected side. Neck veins may be distended, but this may be absent if the patient is hypovolemic. The diagnosis of tension pneumothorax is made clinically. Patients with a tension pneumothorax need immediate treatment and should not wait for X-ray. Figure 24–1 shows the chest X-ray (CXR) of a patient whose physical examination findings should have lead the physician to perform a needle decompression instead of an X-ray (not the mistake of the authors). For stable patients, in whom a pneumothorax is suspected, diagnosis is confirmed with CXR (Figure 24–2). Besides ultrasonography is quickly becoming an alternative to X-ray for rapid identification of pneumothorax. Reported sensitivity for detection of pneumothorax of 86–98% for ultrasound versus 28–75% for supine CXR makes it a potentially attractive alternative.
The treatment for a tension pneumothorax is immediate tube thoracostomy (Chapter 6). If a chest tube is not immediately available, needle thoracostomy with a large-bore (16-gauge or less) needle in the second intercostal space in the midclavicular line will convert the tension pneumothorax into a simple pneumothorax until a tube can be placed. In this instance, the needle should be left in until a definitive chest tube can be placed. Opening the wound further with a gloved finger or a clamp can relieve a tension pneumothorax associated with a penetrating injury. For patients with a simple pneumothoraces secondary to trauma, traditional teaching has been to drain through a tube thoracostomy and admit the patient for observation. However, it has been shown that those with small pneumothoraces detected on CT scan appear at low risk for complications and may not require drainage. In addition, serial observations or simple aspiration have been shown to be safe in patients presenting later or with small simple pneumothoraces.
Large penetrating wounds of the thorax result in an immediate pneumothorax. There is equilibration between intrathoracic and atmospheric pressure and so negative intrathoracic pressure cannot be generated. Effective ventilation is thus impaired since air goes through the chest wall rather than into the lung resulting in severe hypoxia. The diagnosis is obvious and therapy should be instituted immediately.
Management of an open pneumothorax should begin with assessment of the patients ABC’s. All patients with a pneumothorax should be placed on 100% oxygen via nonrebreather. An occlusive dressing should be placed over the wound immediately followed by the placement of a chest tube. The occlusive dressing should be large enough to cover the wounds edges. The dressing should be taped on three side allowing air to escape from the pleural cavity but not reenter. Definitive treatment involves chest tube placement and wound closure.
Injury to the chest wall, great vessels, or lung can result in intrapleural bleeding or hemothorax. By definition, a massive hemothorax is defined by the rapid accumulation of greater than 1000–1500 ml of blood or one-third or more of the patient’s blood volume in the chest cavity. Most commonly, a massive hemothorax is secondary to penetrating injury disrupting pulmonary or systemic blood vessels. In hemothorax associated with great vessel injury, 50% die immediately, 25% live 5–10 minutes, and 25% live 30 minutes or longer. Respiratory insufficiency is dependent on how much blood is lost. In massive injury, the affected lung is collapsed producing a right to left shunt. The loss of blood also leads to circulatory compromise.
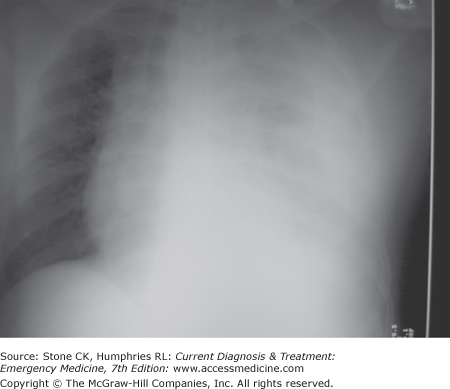
Respiratory distress, tachypnea, and variable degree of hypoxia will be present. There will be dullness to percussion and decreased breath sounds on the affected side. Depending on the degree of blood loss, hypotension and flat neck veins may be present. Pulse pressure will be narrow. Small hemothoraces may be difficult to detect on supine patients. Diagnosis is confirmed by CXR (Figure 24–3). Small hemothoraces (<350 mL) are usually visible only as a small effusion on an upright CXR. Moderate effusions (350–1500 mL) will be seen as diffuse increase in opacity on the affected side. Large (>1500 mL) effusions will have a ground glass appearance on the supine film.
For the patients presenting with signs of massive hemothorax, tube thoracostomy should be performed immediately without waiting for diagnostic tests. For those with smaller hemothoraces, diagnosis can be confirmed before instituting therapy. Tube thoracostomy using one or two large-bore chest tubes allows for accurate assessment of current and ongoing blood loss. Autotransfusion should be considered for the patients with large bleeds (>1 L). Initial blood loss of more than 1.0–1.5 L or ongoing continuing loss of >200 mL/h for 2–4 hours requires surgery.
Cardiac tamponade occurs when arterial, ventricular, or atrial injury causes blood to leak into the pericardium. True tamponade is rare and most often associated with penetrating injuries. The pericardium is acutely not very distensible and tamponade can occur even with a small amount (200 mL) of blood. The increased intrapericardial pressure compresses the heart and decreases cardiac output. In addition, venous return and cardiac filling are decreased. Increased pressure may also lead to a decrease in myocardial perfusion. These factors together lead to a decrease in cardiac output. Hypotension and shock then can result.
Signs and symptoms of tamponade are nonspecific. Tachycardia and narrow pulse pressure are usually present. Beck’s triad of hypotension, muffled heart tones, and distended neck veins is present in a minority of patients with tamponade from blunt trauma. Jugular venous distension may be absent because of coexisting hypovolemia. There are no specific findings on CXR that will confirm the diagnosis. Since tamponade can occur with a small effusion, heart size may not be significantly increased. Bedside focused assessment with sonography for trauma (FAST) examinations (Chapters 6 and 25) are performed in many emergency departments to quickly identify pericardial effusions in blunt and penetrating trauma patients. FAST examinations allow rapid detection of pericardial fluid, with high sensitivity and specificity. An emergency pericardiocentesis or thoracotomy can be lifesaving in an unstable patient with a pericardial effusion. In a stable patient, the diagnosis of pericardial effusion can be confirmed with transthoracic or transesophageal echocardiogram and define the hemodynamic impact. When ultrasound or echocardiography is not available, for the stable patient, CT scan is sensitive for detection of pericardial fluid. Cardiac dynamics are not assessable however.
Pericardiocentesis has been advocated in the past as both a diagnostic and therapeutic modality. However there are serious limitations. Pericardiocentesis has been reported to have up to 80% false negatives and 35% false positives. In acute injury, a large part of the pericardial blood may be clotted and therefore not aspirated through even a large-bore needle. Pericardiocentesis may injure the heart or other organs and may cause delays in getting definitive care. With these caveats, in a stable patient, ultrasound-guided pericardiocentesis has been shown to be safe and reliable. In patients who are unstable or in severe shock with signs and symptoms consistent with cardiac tamponade, immediate thoracotomy allows relief of the tamponade and control of myocardial injury.
Flail chest occurs when a segment of the chest does not have bony contiguity with the rest of the thoracic cage. When negative intrathoracic pressure is generated on inspiration, the flail segment moves inward, thus reducing tidal volume. Usually a significant blunt force is required, eg, motor vehicle collision (MVC) or a fall from a height. The major problem is respiratory failure due to the underlying pulmonary injury.
The two major symptoms of flail chest are pain and respiratory distress. Tachypnea with shallow respirations secondary to pain will be seen. Paradoxical chest wall movement may not be seen in a conscious patient due to splinting of the chest wall. Crepitus is often present. Even with marked flail chest, the patient may be able to compensate initially for the reduced tidal volume by hyperventilating. When fatigue or underlying pulmonary injury develops, frank respiratory failure may supervene.
Supplemental oxygen is the first-line treatment. Pain control with intravenous morphine or fentanyl should be instituted early. Patient controlled administration (PCA) of an opiod infusion is often effective for cooperative patients. Epidural infusion of a local anaesthetic agent provides near complete analgesia allowing the patient to resume normal inspiration and cough without the risk of respiratory depression. The addition of a nonsteroidal may provide adequate relief, but should be withheld until other injuries have been excluded. Consider early intubation and mechanical ventilation in any patient with ongoing hypoxia or significant increased work of breathing. Approximately 50% of patients will need immediate intubation. Indications for early intubation include marked hypoxia, hypercapnea, or inadequate breathing. External chest wall supports (taping, sandbags) reduce pain with movement of the flail segment, but they also reduce vital capacity and may worsen respiratory function and are therefore not indicated. Surgical fixation should only be considered in cases where thoracotomy is being performed for other injuries.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree