Bony anatomy of the cervical spine.
Muscles
The trapezius, rhomboids, and levator scapulae muscles reside posteriorly.
The trapezius runs from the spinous processes of the c- and t-spine to the angle of the scapula and is innervated by the spinal accessory nerve and the C3 and C4 nerve roots.
It assists in lateral flexion, rotation away from the side of contraction, and extension.
The rhomboid major and minor originate at the spinous processes of C7–T5 and insert on the medial border of the scapula.
They are innervated by the dorsal scapular nerve, C4, and C5.
They assist in adduction and elevation of the scapula.
The levator scapula muscle runs from the spinous processes of C1–C4 to the superomedial portion of the scapula.
It assists in lateral flexion and rotation.
The scalene muscles are located laterally.
They run from the transverse processes of the cervical vertebrae to the first rib and are innervated by branches of C3–C8.
They support lateral flexion, rotation, and forward flexion.
The sternocleidomastoid (SCM) muscle runs anterolaterally.
It runs from the manubrium and medial clavicle to the mastoid process.
Nerve supply is C2, C3, and the spinal accessory nerve.
It aids in flexion, rotation away from side of contraction, and lateral flexion.
There are two deep muscles in the neck: the splenius capitis and longus capitis.
The splenius capitis arises from the spinous processes of C7–T3 and inserts on the mastoid process.
It is innervated by the C4–C8 nerve roots.
It helps extend, laterally flex, and rotate the neck.
The longus capitis originates from the spinous processes of C3–C6 and inserts on the base of the occiput.
It is innervated by C1–C4.
It acts as a flexor, lateral flexor, and rotator.
Neurovascular Structures
There are eight cervical nerves (C1–C8), which exit above the vertebral body for which they are named.
The spinal canal is funnel shaped, so the cord occupies relatively little space in the upper c-spine and up to 75 percent in the lower c-spine.
Space available for the spinal cord is normally between 14–23 mm.
Stenosis is defined as a canal of less than 13 mm.
Cord compression typically occurs at diameters of less than 10 mm.
The brachial plexus arises from the C5–T1 nerve roots and exits the neck between the anterior and medial scalene muscles.
It terminates as the median, radius, ulnar, axillary, and musculocutaneous nerves.
Proximal to these branches, it gives rise to several important nerves, including the dorsal scapular nerve and suprascapular nerve.
The internal carotid and vertebral arteries are the two most important arterial structures that traverse the neck.
Both arise from the subclavian artery.
The internal carotid accompanies the internal jugular vein and gives off the external carotid artery at about the C4 level, before passing into the skull via the carotid foramen.
The vertebral artery runs posteriorly, through the transverse foramina of the cervical vertebrae through the foramen magnum.
Embryologic Considerations
A basic understanding of cervical embryology may help explain injuries patterns in children and radiographic findings.
The neural arches of C1 form during the seventh fetal week, but do not fuse until age 3 (posterior arch) and age 7 (anterior arch) on average.
This lack of fusion during early childhood may easily be mistaken for a fracture radiographically.
C2 has two additional ossification centers for the odontoid process.
One is present at birth, and the second develops at the tip of the dens between 3 and 6 years of age, fusing at 12 years.
The rest of the odontoid process fuses to the body between 3 and 6 years.
Remnants of these fusion lines also resemble fractures radiographically.
The subaxial cervical vertebrae have neural arches that fuse between 2 and 3 years of age.
These fuse with the body by age 6.
Secondary ossification centers develop for the transverse and spinous processes.
These centers may remain unfused until the third decade of life and are often mistaken for fractures.
Initial Stabilization
As with any trauma patient, a primary survey and initial stabilization of the c-spine is critical in the prehospital setting for any athlete with a suspected head or neck injury. This management precedes a full history and physical exam.
Universal spine precautions should be observed, with immediate transport to an appropriate ED via emergency medical services (EMS).
A detailed discussion of prehospital management is beyond the scope of this text, with one exception: the helmeted athlete.
Modern American football helmets and pads are designed to provide appropriate alignment of the c-spine. In general, these should be left in place in the athlete with a head, neck, or undifferentiated injury.
This practice is starting to change if there are enough prehospital providers who are trained and able to provide in-line cervical immobilization while removing pads and helmets.
In other sports, and with football players with ill-fitting equipment, helmet and shoulder pads should be removed while simultaneously observing universal spine precautions.
In the unconscious athlete, or when airway compromise is of concern, the facemask alone should be removed.
It is generally accepted that all football players requiring transfer to the ED for a potential head/neck injury have the facemask removed.
When helmet removal is required, careful attention to head and spine alignment is paramount, to avoid worsening of a potentially unstable injury.
There are commercially available devices to assist with removal, but manual removal remains the most common method.
Comparison studies have been performed to assess which method minimizes head/neck movement and movement velocity, with pros and cons for both methods. There is not yet clear consensus on the best technique.22
Hands-on training for helmet and pad removal techniques are highly recommended.
History
After initial stabilization and appropriate transfer, a more detailed history and physical exam may be obtained (secondary survey).
As with most medical conditions, a careful, focused history will provide the majority of the information needed to form and narrow the differential diagnosis.
Understanding the mechanism of injury is an important first step.
The most common sport-related mechanism of cervical spinal trauma involves an axial load or a large compressive force applied to the top of the head.
More severe injuries tend to occur when the neck is in a slightly flexed position, which negates the lordotic curve. This transfers the force of the impact from the soft tissues to the cervical column.
The location and nature of the complaint should then be discussed.
Location of pain, such as radicular vs. axial, should be noted.
Associated upper extremity symptoms such as pain, numbness, paresthesias, or weakness should also be noted.
The evolution of the pain since the time of injury should be discussed.
Note if symptoms are improving, worsening, or staying the same.
As part of the secondary survey, screening for additional or distracting injuries is also an important aspect of the history.
Head injuries, especially concussions, frequently accompany neck injuries, even minor ones.
It is important to ask if the athlete has a headache, vision changes, vomiting, or mental status changes.
As with all trauma patients, NEXUS criteria and the Canadian c-spine rules pertain, and may help determine which patients require radiographic evaluation. (Table 9.1, Table 9.2)
| Midline c-spine tenderness |
| Focal neurologic deficit |
| Altered level of consciousness |
| Intoxication |
| Distracting injury |
| If none of the above findings are present, the patient’s c-spine may be cleared clinically without radiographs. |
1. Any high-risk factor that mandates radiographs? If yes, obtain radiographs. If no, proceed to #2. | a) Age greater than or equal to 65 b) Dangerous mechanism i. Fall from > 3 ft or 5 stairs ii. Axial load to head (e.g., driving) iii. MVC high speed (>100km/h), rollover, ejection iv. Motorized recreational vehicle v. Bicycle crash c) Paresthesias in extremities |
2. Any low-risk factor that allows safe assessment of range of motion? If yes, proceed to #3. If no, obtain radiographs. | a) Simple rear-end MVC with the following exclusions: i. pushed into oncoming traffic ii. hit by large truck or bus iii. rollover iv. hit by high-speed vehicle b) Sitting position in ED c) Ambulatory at any time d) Delay in onset of neck pain e) Absence of midline cervical spine tenderness |
3. Able to actively rotate neck? If yes, no radiographs are necessary. If no, obtain radiographs. | 45° to each side |
These rules are intended for alert (GCS = 15) and stable trauma patients when cervical spine injury is a concern.
Physical Exam
The physical exam of the neck should follow the same general guidelines as all other parts of the musculoskeletal system: inspection, palpation, range of motion, special tests, and neurovascular exam.
Inspection
In the immobilized patient, the exam will start in a supine position.
In all other patients, exam is best performed seated.
Assess the neck for angular or rotational deformities, visual step-offs, and soft tissue injuries.
Don’t forget to inspect the anterior aspect of the neck as well, which may require c-collar removal with an assistant providing manual stabilization.
Assess the thoracic area and upper extremities for scapular winging and atrophy (in more chronic injuries).
Palpation
The spinous processes of C2–T1 should be palpated for tenderness.
C2 is felt in the midline directly under the occiput.
C7 and T1 are quite prominent and easily palpable, but often confused.
With active extension C7 will move anteriorly, while T1 remains relatively stable.
In thin patients, the transverse processes may often be palpated, especially at C4, which has the shortest spinous process.
The paraspinal muscles should then be palpated posteriorly, then the scalenes laterally, and sternocleidomastoid muscle anteriorly.
Also palpate the trachea, clavicles, and sternal notch.
Palpation of the brachial plexus laterally is also recommended for pain or to see if it elicits radicular symptoms.
Range of Motion
If the c-spine has been cleared clinically or radiographically, it is safe to assess range of motion. If not, this step should be postponed until appropriate clearance is obtained.
Flexion and extension from neutral.
Normal flexion is 80 to 90° or two finger widths between the chin and chest.
The SCM is the dominant flexor.
Normal extension is approximately 70°.
The trapezius is the dominant extensor.
Rotation
Normal rotation is 60 to 80°. Young healthy patients may usually rotate enough that the chin is nearly in line with the shoulder.
The SCM muscles are the primary rotators.
Lateral flexion
Be sure to tell the patient not to elevate the shoulder.
Normal lateral flexion is between 20 and 45°.
The scalene muscles are the primary lateral flexors.
As with any joint, note symmetry of movement, and which movements bring on or exacerbate symptoms.
Neurovascular Exam
See Table 9.3 for review of spinal nerve function in the c-spine.
Strength should be assessed for all major upper extremity muscle groups (shoulder shrug, shoulder abduction, elbow flexion and extension, wrist flexion and extension, grip strength).
Kumar’s sign (Figure 9.2), is a quick way to assess radial, median, and ulnar nerve function.
This test involves extension of the wrist (radial nerve), finger opposition (ulnar), and the “OK sign” with the thumb and index finger (median nerve).
If a deficit is identified, further strength and sensation assessment for that particular nerve is indicated.
Trying to quantify with the standard 0 to 5 scale is appropriate, but it is most important to document comparison to the opposite upper extremity.
Sensation to light touch should be assessed to both upper extremities, the trunk, and the lower extremities, assessing for deficits that follow a dermatomal distribution.
If deficits are seen in a specific area, cold-hot and sharp-dull differentiation are appropriate follow-up tests to document.
Biceps, triceps, and brachioradialis reflexes should be obtained and compared to the contralateral extremity. The standard 0 to 4+ scale is often used to help quantify reflex strength, with 3+ being brisk, 4+ being clonus, and 0 nonexistent.
Vascular exam may be completed by checking radial and ulnar pulses and capillary refill.
| Nerve | Motor Function | Sensory Function | Reflex |
|---|---|---|---|
| C5 | Deltoid, supraspinatous, infraspinatous | Lateral arm | Biceps |
| C6 | Biceps, wrist extensors | Radial forearm, thumb, index finger | Biceps, brachioradialis |
| C7 | Triceps, wrist flexors, finger extensors | Middle finger | Triceps |
| C8 | Finger flexors | Fourth and fifth fingers | None |
| T1 | Finger abductors | Ulnar forearm | None |
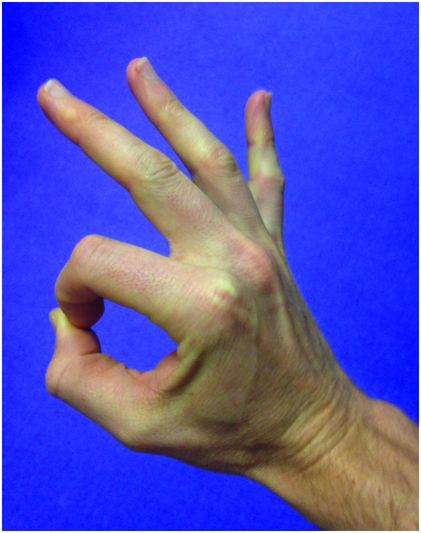
Kumar’s sign.
Special Tests
Spurling’s test
Spurling’s test (Figure 9.3) is perhaps the most useful special test in assessment for a nerve root impingement syndrome.
The examiner passively rotates and extends the neck, then provides a firm, controlled axial load to the patient’s head.
Pain referred to the ipsilateral upper extremity, beyond the shoulder, is considered a positive test, and should increase index of suspicion for nerve root impingement.
The sensitivity of Spurling’s test is 30–50 percent, with a specificity of 74–93 percent.23,24
Hoffman’s sign
Hoffman’s sign is a test for an upper motor neuron injury.
The examiner flicks the tip of the long finger of a relaxed hand. If this elicits flexion of the thumb and index finger in a pincer motion, the test is considered positive.
Trials suggest a sensitivity between 33 and 58 percent, with specificity between 59 and 78 percent, although its reliability as a single test is questionable.25
When used in combination with other tests, however, its utility increases.
Elevated arm stress test (EAST or Roos test) and Adson’s maneuver.
These tests are assessment tools for thoracic outlet syndrome (TOS) which may present with radicular-type upper extremity symptoms.
Elevated arm stress test (Figures 9.4 A and B) is performed with the patient sitting with shoulders abducted to 90° and elbows flexed to 90°. The patient then opens and closes the hands for 3 minutes. If reproduction of symptoms occurs during this time, it is considered a positive test.
Elevated arm stress test (Figures 9.4 A and B) has a sensitivity of 84 percent and sensitivity of 30 percent, based on minimal evidence.26
Adson’s maneuver (Figure 9.5) is performed with the examiner palpating the radial pulse on the affected side. The arm is then passively externally rotated, extended, and abducted slightly. The patient rotates the head toward the affected side. If the pulse disappears, this is considered a positive test and concern for vascular TOS is increased.
One study suggests that Adson’s maneuver has a sensitivity of 79 percent and specificity of 76 percent.27
As with all areas of the body, special tests are best used as adjuncts to help increase or decrease the clinical suspicion for a specific injury. They are not meant to be used in isolation.

Spurling’s test.
Elevated arm stress test.



Adson’s maneuver.
Differential Diagnosis – Emergent and Common Diagnoses
A reasonable differential diagnosis for neck pain and radicular-type arm pain in the athlete is listed in Table 9.4.
As with all medical conditions, the differential changes based on history, physical exam, and imaging studies.
Older patients with nontraumatic or minimally traumatic neck pain may have a broader differential, including cardiac, pulmonary, and even intra-abdominal pathology. These conditions are not included in this text.
| Emergent | Common |
|---|---|
| Catastrophic cervical spine injury | Brachial plexus neuropraxia |
| Cervical spine fracture/dislocation | Cervical disc herniation |
| Cervical cord neuropraxia with persistent neurological deficits | Cervical sprains/strains/contusions |
| Acute, traumatic cervical disc herniation | Neurologic thoracic outlet syndrome |
| Any cervical disc herniation with associated neurologic deficits | |
| Vascular thoracic outlet syndrome | |
| Any injury with persistent neurological deficits |
Catastrophic C-Spine Injury
Description
Sport-related c-spine injuries are typically divided into three groups.
Type 1 injuries are catastrophic spinal cord injuries resulting in permanent neurologic deficits. A catastrophic c-spine injury is defined as “a structural distortion of the cervical spinal column associated with actual or potential damage to the spinal cord.”21 These injuries are discussed in this section.
Type 2 injuries (discussed separately) result in transient neurologic symptoms with normal radiographic studies. Neuropraxias and most traumatic disc herniations are examples of type 2 injuries.
Type 3 injuries (discussed separately) are those with radiographic abnormalities but no neurologic deficit. These include fractures (both stable and some unstable), some fracture-dislocations, and certain disc herniations.
Catastrophic c-spine injuries are categorized into four separate syndromes.
Brown–Sequard syndrome results from hemisection of the spinal cord. It results in ipsilateral loss of motor function, proprioception, and vibratory sensation, with contralateral loss of pain and temperature sensation.
Anterior spinal cord syndrome results in damage to the spinothalamic and corticospinal tracts with preservation of the posterior columns. This is manifested by loss of motor function, pain, and temperature below the lesion with preservation of vibration, proprioception, and crude touch.
Central cord syndrome is caused by damage to the centrally located fibers of the corticospinal and spinothalamic tracts. This results in decreased strength, pain, and sensation predominantly in the upper extremities.
Mixed injuries usually are a combination of Brown–Sequard syndrome and central cord syndrome. They result in crossed motor and sensory deficits predominantly to the upper extremities.
Unstable fractures with or without dislocation are the most common cause of catastrophic c-spine injury.
Mechanism
The most common mechanism of injury in catastrophic c-spine injuries is an axial load to a slightly flexed neck.
In a neutral position, normal cervical lordosis helps dissipate forces to paraspinal muscles and other soft tissues, avoiding injury to the spinal column itself.
Presentation
Descriptions of the four categories of catastrophic c-spine injury are discussed earlier. As mentioned, the majority of patients present with mixed injuries and varying degrees of sensory and motor deficits below the level of injury, predominantly in the upper extremities.
Many patients are comatose or otherwise unable to provide an appropriate history due to head injury or other associated injuries.
The vast majority of athletes are transported to the ED by EMS on a backboard. If appropriate guidelines are followed, football players have pads and helmet on, with facemask removed. If not, the facemask should be removed immediately for necessary airway management.
It should be noted that plain films and CT scans can and should be performed with helmet and pads on, unless there are associated injuries that require removal. Again, helmet and pads should be removed together.
In other athletes with helmet and pads (i.e., hockey, lacrosse), equipment should be removed.
Physical Exam
Athletes with c-spine injuries are, and should be treated as typical trauma patients. Thus, physical exam should always begin with a primary survey, with interruptions for cardiopulmonary interventions when indicated.
The primary survey should include a brief neurologic evaluation, assessing gross motor and sensory function to the trunk and extremities.
A secondary survey should follow, including a more detailed neurologic exam in the awake patient who is able to speak and protect their airway.
This exam should include sensation to light touch, sharp-dull discrimination, two-point touch discrimination, and basic assessment of extremity proprioception (toe/thumb up, toe/thumb down test).
It is critical to document as much of a neurologic exam as possible prior to sedation, paralysis, and intubation.
Full spine precautions should be observed throughout the examination.
Range of motion testing and the special tests described earlier, with the exception of Hoffman’s sign, should not be performed in this population.
Essential diagnostics
Plain c-spine radiographs and/or CT scan should be obtained immediately in patients with suspected catastrophic c-spine injury.
In those with neurologic deficits on exam, emergent MRI should be performed even if the CT scan is unremarkable.
ED Treatment
The primary goal of ED management of patients with potentially catastrophic c-spine injury is to prevent secondary neurologic injury due to improper handling of the injured athlete in the ED.
Unstable injuries without neurologic compromise may be converted to those with permanent deficits if appropriate precautions are not observed.
A proper fitting cervical collar in the non-helmeted athlete or manual c-spine stabilization in the helmeted athlete is essential.
Log rolling with at least four people is recommended during the secondary survey.
Full thoracic and lumbar spine precautions should continue until an unstable cervical injury is excluded.
The second goal is a prompt and accurate diagnosis using history, physical exam, and diagnostic imaging.
The third priority is timely stabilization of unstable injuries. Spine consultants (neurosurgery and/or orthopedics) should be contacted early.
Consultation is indicated in any athlete with neurologic symptoms with or without radiographic findings, or those with radiographic findings (fracture, cord edema, ligamentous instability) without neurologic symptoms.
Supportive care, pain control, management of associated injuries, and communication with family are also important tasks that often fall to the emergency physician.
The use of high-dose steroids in SCI is controversial, and has been a hotly debated topic for the past several decades.
The initial adoption of the practice occurred after the NASCIS (National Acute Spinal Cord Injury Study) II and III trials in 1990 and 1997 respectively.28,29 These trials concluded that administration of high-dose methylprednisolone within eight hours of injury was beneficial to the patient’s neurologic outcome.
Subsequent studies brought into question the validity of NASCIS II and III, with more recent studies suggesting ineffectiveness and potential harm from high-dose methylprednisolone.30
Thus, high-dose steroids are currently not recommended in patients with SCI.
The use of hypothermia is also controversial.
Currently, there is not sufficient evidence to recommend the use of local or systemic hypothermia for these patients.31
However, several clinical studies have demonstrated encouraging evidence over the last several years, without large, multi-center trials.32
Thus, recommendations may change in the near future.
Consultation with a spine specialist regarding the use of steroids and hypothermia is recommended.
Disposition
Patients who present with neurologic compromise or unstable injuries should be admitted to an intensive care unit due to the risk of respiratory failure and hemodynamic instability (spinal shock).
Athletes with stable injuries without neurologic symptoms may often be discharged after consultation with a spine specialist. Follow-up with neurosurgery/orthopedics should be arranged prior to discharge.
Those with no radiographic abnormalities and no neurologic symptoms may be discharged with follow-up with sports medicine, orthopedics or the PCP in five to seven days.
Return to play is only considered in athletes with no radiographic abnormalities, no evidence of neurologic compromise, and improving pain.
These athletes may gradually return after: (1) resolution of pain, (2) they obtain full range of motion of extremities, and (3) they obtain full strength of extremities.
The physician should encourage a stepwise return to sport supervised by an athletic trainer or coach.
Athletes with permanent neurologic deficits or injuries requiring surgical stabilization are disqualified from contact sports.
Those with stable injuries without neurologic compromise may eventually return to sport.
The emergency physician should not play a role in clearing these athletes.
Complications
Improper handling of a patient with an unstable spine injury may lead to, or worsen, permanent neurologic deficits.
In high cervical lesions, usual above C5, respiratory compromise is likely. This occurs due to damage to the roots of the phrenic nerve, which innervates the diaphragm.
It is recommended that these patients be intubated immediately after diagnosis.
Patients with severe c-spine injury are also at risk for hemodynamic instability, or “spinal shock.”
If left untreated, this may lead to cardiovascular collapse and death.
Thus, close monitoring and supportive care is of utmost importance.
Pediatric Considerations
Spinal cord injury without radiographic abnormality (SCIWORA).
SCIWORA is a well-described phenomenon occurring predominantly in children.
It involves clinical evidence of SCI without findings on plain radiographs or CT scan.
In the vast majority of cases, abnormalities are found on MRI, however these findings may be subtle.
Thus, in any pediatric patient with neurologic complaints or findings, an MRI should be obtained when plain x-ray and CT scans are negative.
The mechanism is not well understood, but it is thought to be due to transient deformity of the c-spine due to ligamentous laxity.
Spinal cord ischemia may also play a role.
Deficits may include partial or complete paralysis.
There are reports of SCIWORA that manifests as Brown–Sequard syndrome, central cord syndrome, and anterior cord syndrome.
Onset of deficits may be immediate, but may be delayed for hours, and in rare cases up to a few days.
Thus, appropriate education for the athlete and their family regarding the possibility of delayed neurologic sequelae is appropriate.
There is a wide range of symptoms, and the prognosis depends on the severity of deficits.
Management is the same as for all catastrophic spinal cord injuries.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








