3 Cervical Spine ! +++ R1–2 times a week MM, Auto, BFB, Chiro, TENS !++ R once a week MM, Orthotech, Med, Auto
 Complex Pain
Complex Pain
Nonspecific Neck Pain
Indications
 Pain in the area of the posterior cervical spine without point of maximal intensity, not related to specific muscles, frequently including hyper-pathia of the skin
Pain in the area of the posterior cervical spine without point of maximal intensity, not related to specific muscles, frequently including hyper-pathia of the skin
 Pain when actively flexing the neck, increasing against resistance
Pain when actively flexing the neck, increasing against resistance
 Increased pain with passive flexion
Increased pain with passive flexion
Differential Diagnoses
 Arthrosis of the cervical facet joints
Arthrosis of the cervical facet joints
 Myalgia of the deep neck extensors
Myalgia of the deep neck extensors
 Interspinous neoarthrosis (pain is absent during passive flexion)
Interspinous neoarthrosis (pain is absent during passive flexion)
Material
 Local anesthetic: 10 mL
Local anesthetic: 10 mL
 Needle: 0.4 × 20 mm
Needle: 0.4 × 20 mm
Technique
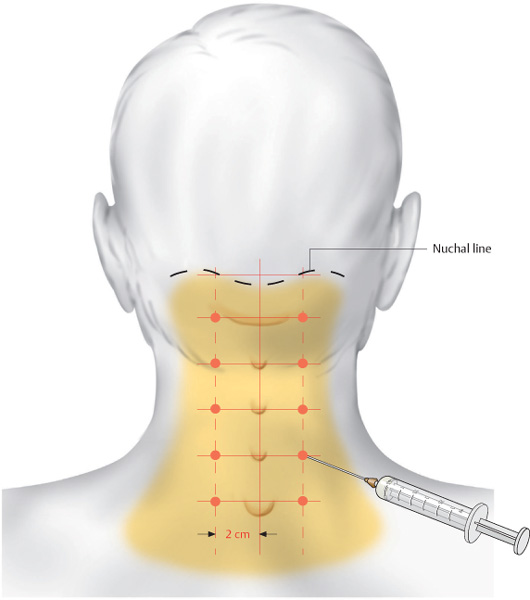
 The tips of the spinous processes are marked. The injections sites are located 2 cm paramedially to the right and to the left, at the level of the tips of the spinous processes. The needle is inserted vertically.
The tips of the spinous processes are marked. The injections sites are located 2 cm paramedially to the right and to the left, at the level of the tips of the spinous processes. The needle is inserted vertically.
 The depth of insertion is 1–2 cm and each injection site receives 0.5 mL of a local anesthetic.
The depth of insertion is 1–2 cm and each injection site receives 0.5 mL of a local anesthetic.
Risks
 None
None
Concomitant Therapies
 Stretching of the posterior cervical muscles
Stretching of the posterior cervical muscles
 Glisson traction
Glisson traction
 Local heat application
Local heat application
 Neck compress
Neck compress
 Progressive muscle relaxation
Progressive muscle relaxation
Interspinous Neoarthrosis/Irritation of the Interspinales
Indications
 Distinct segmental pain in the posterior neck, increasing during active and passive neck flexion and remaining unchanged during neck extension
Distinct segmental pain in the posterior neck, increasing during active and passive neck flexion and remaining unchanged during neck extension
Differential Diagnoses
 Tendinosis at the insertion of the deep neck muscles
Tendinosis at the insertion of the deep neck muscles
 Irritation of the vertebral joints
Irritation of the vertebral joints
Material
 Local anesthetic: 2 mL
Local anesthetic: 2 mL
 Needle: 0.4 × 20 mm
Needle: 0.4 × 20 mm
Technique
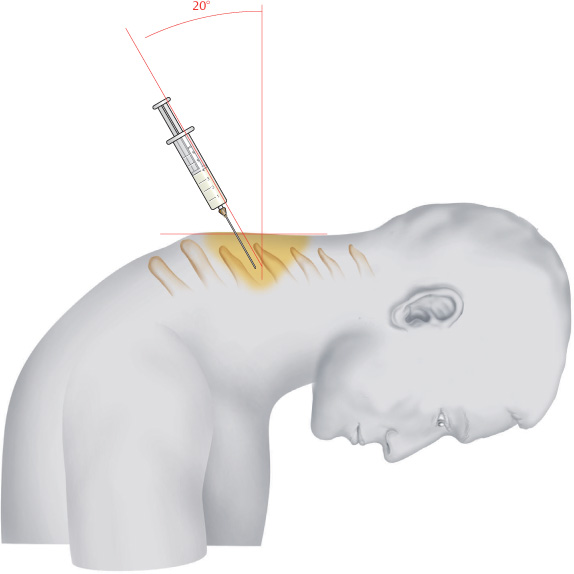
 The patient is seated, shoulders are relaxed, and the cervical spine is extended. The spinous process of C 7 is palpated; from there palpation moves upward until the painful segment is identified. To confirm the finding, the neck is passively extended, which must produce the characteristic pain.
The patient is seated, shoulders are relaxed, and the cervical spine is extended. The spinous process of C 7 is palpated; from there palpation moves upward until the painful segment is identified. To confirm the finding, the neck is passively extended, which must produce the characteristic pain.
 The injection site is located between the palpable tips of the spinous processes. The needle is inserted at a 20° angle cranially. The depth of insertion is 1.5–2 cm. Distinct resistance is felt when the nuchal ligament is penetrated.
The injection site is located between the palpable tips of the spinous processes. The needle is inserted at a 20° angle cranially. The depth of insertion is 1.5–2 cm. Distinct resistance is felt when the nuchal ligament is penetrated.
Risks
 Injections into the nuchal ligament frequently produce intense pain; therefore, injection is discontinued in cases of high resistance.
Injections into the nuchal ligament frequently produce intense pain; therefore, injection is discontinued in cases of high resistance.
 Advancing the needle excessively creates the risk of an epidural injection. The extended position of the neck allows the interlaminar gap to widen. Therefore, longer needles must not be used.
Advancing the needle excessively creates the risk of an epidural injection. The extended position of the neck allows the interlaminar gap to widen. Therefore, longer needles must not be used.
Concomitant Therapies
 Passive traction of the cervical spine
Passive traction of the cervical spine
 Orthopedic brace extending the cervical spine
Orthopedic brace extending the cervical spine
 Administration of NSAIDs with systemic effect
Administration of NSAIDs with systemic effect
 Treatment through Muscles, Tendons, and Ligaments
Treatment through Muscles, Tendons, and Ligaments
Levator Scapulae
Indications
 Pain in the posterior shoulder, frequently non-specific and dull, cannot be exactly localized by the patient
Pain in the posterior shoulder, frequently non-specific and dull, cannot be exactly localized by the patient
 Characteristic trigger point in the area of the muscle’s superior border at the tip of the medial scapula, frequently radiating across the superior border of the trapezius
Characteristic trigger point in the area of the muscle’s superior border at the tip of the medial scapula, frequently radiating across the superior border of the trapezius
Differential Diagnoses
 Facet irritation in the C 5/C 6 segment
Facet irritation in the C 5/C 6 segment
 Irritation of the suprascapular nerve with compression in the area of the suprascapular notch caused by the transverse scapular ligament
Irritation of the suprascapular nerve with compression in the area of the suprascapular notch caused by the transverse scapular ligament
 Costovertebral joint block at the level of T 3
Costovertebral joint block at the level of T 3
Material
 Local anesthetic: 3 mL
Local anesthetic: 3 mL
 Needle: 0.4 × 20 mm
Needle: 0.4 × 20 mm
Technique
 The tip of the medial scapula is located and is usually very sensitive to pressure. The most important injection site is in the center of this painful area. Two additional injection sites are located on a transverse line in the craniomedial direction, each 3 cm apart.
The tip of the medial scapula is located and is usually very sensitive to pressure. The most important injection site is in the center of this painful area. Two additional injection sites are located on a transverse line in the craniomedial direction, each 3 cm apart.
 Each site receives 1 mL of a local anesthetic injected 2 cm deep.
Each site receives 1 mL of a local anesthetic injected 2 cm deep.
Risks
 None
None
Concomitant Therapies
 Cryogenic friction massage at the insertion site of the levator scapulae
Cryogenic friction massage at the insertion site of the levator scapulae
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree