Cross section of cervical epidural space. 1. Ligamentum flavum, 2. epidural space with venous plexus, 3. spinal ganglion, 4. spinous process, 5. body of vertebra, 6. dorsal branch of spinal nerve, 7. ventral branch of spinal nerve. (Reprinted with permission from Dr. Danilo Jankovic)

The left diagram demonstrated the ascending cervical and deep cervical arteries anastomosing with the vertebral artery posterior to the spinal nerves. Note that the ascending cervical artery enters the foramen at C3-4 or C4-5, whereas the deep cervical artery enters the more distal C5-6, C6-7, or C7-T1 foramina. The right diagram showed a cervical transforaminal needle cannulating a segmental artery contributed by the ascending cervical artery. Steroid particles (purple) are shown coalescing in the anterior spinal artery. (Reprinted with permission of Mayo Foundation for Medical Education and Research)
The cervical spinal nerve occupies the lower part of the foramen with the epiradicular veins in the upper part (Figs. 12.1 and 12.2). The radicular arteries arising from the vertebral, ascending cervical and deep cervical arteries lie in close approximation to the spinal nerve.
In a cadaver study, Huntoon showed that the ascending and deep cervical arteries may contribute to the anterior spinal artery along with the vertebral artery (Fig. 12.2). In 20% of the foramina dissected, the ascending cervical artery or deep cervical artery branches within 2 mm of the needle path for a cervical transforaminal procedure. One-third of these vessels entered the foramen posteriorly potentially forming a radicular or a segmental feeder vessel to the spinal cord, making it vulnerable to inadvertent injury or injection even during correct needle placement.
In another cadaver study, Hoeft et al. showed that radicular artery branches from the vertebral artery lie over the most anteromedial aspect of the foramen, while those that arise from the ascending or deep cervical arteries are of greatest clinical significance as they must course medially throughout the entire length of the foramen.
Patient Selection
Cervical nerve root block/transforaminal epidural injections are indicated in cervical radicular pain not responsive to conservative therapy. Cervical epidural injections can be performed using an interlaminar or a transforaminal approach. As cervical radicular pain is frequently caused by foraminal stenosis, transforaminal approach can maximize the concentration of steroid delivered to the affected nerve roots while reducing the volume of injectate required and was shown to be effective in relieving radicular symptoms.
Ultrasound Scan
Patient position: Lateral decubitus position with injection side up.
Probe: Linear, high resolution 6–18 MHz
Scan 1: Identification of the cervical spine level
The ultrasound probe is placed in the short axis of the spine at the level of cricoid. At this level, the probe is moved in cephalad and caudal direction until the cervical tubercles are identified. The character of fifth to seventh cervical spine is illustrated below (Figs. 12.3, 12.4 and 12.5).

Cervical 5th nerve root. Note the anterior and posterior tubercles are similar in size and give the impression of the double camel hump. (Reprinted with permission from Philip Peng Education Series)

Cervical 6th nerve root. Note the prominent anterior tubercle (Chassaignac’s tubercle). (Reprinted with permission from Philip Peng Education Series)

Cervical 7th nerve root. Note the presence of posterior tubercle while the anterior is either absent or vestigial. The vertebral artery is in close proximity to the nerve root. (Reprinted with permission from Philip Peng Education Series)

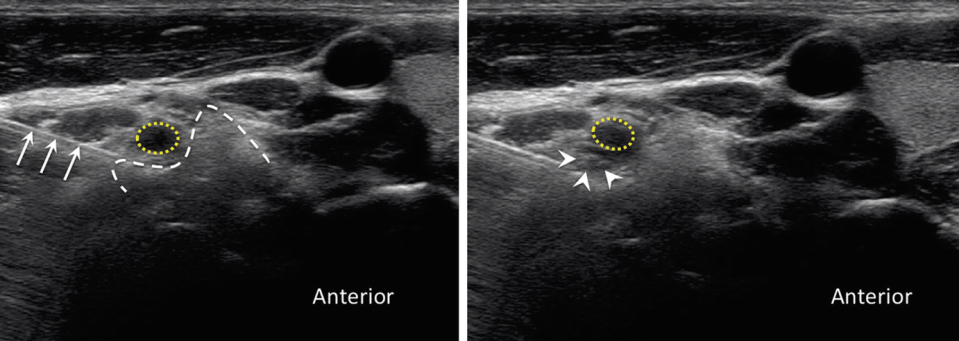
The left sonogram showed the typical location of the vessel in the ventral aspect of the C6 nerve root. The right sonogram showed the rich presence of the vessel in both the ventral and dorsal aspect of the nerve root. (Reprinted with permission from Philip Peng Education Series)
Once the level is counted, the probe is tilted to optimize the visualization of nerve root. The clinician should minimize the use of pressure to reveal the pulsation of the vessel in the vicinity of the nerve root (Fig. 12.6).
Procedure
Needles: 22G blunt-tip needle if available
Drug: 1–2 ml Bupivacaine 0.25% for diagnostic blocks; 1–2 ml Bupivacaine 0.25% and 4 mg Dexamethasone for therapeutic injections