Central Venous Catheters
Antonio Aponte-Feliciano
Alan Orquiola
Theofilos P. Matheos
Stephen O. Heard
I. GENERAL PRINCIPLES
A. Catheter types.
1. Single lumen.
2. Multilumen (double, triple, or quad).
3. Introducer.
4. Double-lumen dialysis catheters.
B. Site selection.
1. Major sites.
a. Internal jugular vein (IJV).
b. Subclavian vein (SCV).
c. External jugular vein (EJV).
d. Femoral vein.
e. Antecubital vein (peripherally inserted central catheters).
2. Depends on skill of operator: greater risk of pneumothorax with subclavian approach.
3. Risk of infection: femoral > internal jugular > subclavian.
4. Avoid sites involving infection, burns, or other dermatologic processes.
C. Methods to reduce risk of catheter infection.
1. Education program with safety checklist.
2. Empowering nursing to stop procedure if sterile technique is violated.
3. Dedicated catheter cart stocked with all necessary supplies.
4. Use chlorhexidine preparatory solution.
5. Use subclavian site preferably.
6. Use maximum barrier precautions: cap, mask, sterile gloves and gown, and sterile drape that entirely covers patient.
7. Remove catheters when no longer needed.
8. Avoid guidewire exchanges as possible.
9. Use antimicrobial impregnated catheters if infection rates remain high despite institution of infection control measures.
10. Avoid use of femoral site and move catheter from femoral site to another as soon as possible.
D. Use of ultrasonographic guidance.
1. Certain patient characteristics that carry higher risk of complications when using the anatomic approach.
a. Anatomy: morbid obesity; local scarring; radiation therapy; short, thick neck; transplant patients; edema.
b. Comorbidities: coagulopathy, bullous emphysema, maximal ventilator support.
2. Allows better visualization of the anatomy, skin to vessel distance. Color flow Doppler allows one to identify flow direction (red toward and blue away from ultrasound probe) and avoidance of preexisting thrombus. The vein should be compressible.
3. The center of the screen will match the center of the probe. A mark on one side of the screen will match a mark or light on the ultrasound probe; this will allow orientation.
4. Decreases failure rate, multiple attempts at cannulation, mechanical failure rates, and infection rates.
5. Disadvantages: steep learning curve.
6. There are two ways to cannulate a vessel with ultrasound guidance.
a. Transverse view: provides complete visualization of the surroundings of the vessel. The needle should be inserted parallel to the probe; deviation could cause arterial puncture or structural damage.
b. Longitudinal plane: allows visualization of the path of the vessel and the needle entrance point. Ensure probe is maintained over the vein; sliding the probe laterally or medially could lead to an arterial puncture.
II. INDICATIONS
A. Monitoring of fluid status.
B. Administration of irritant medications or vasoactive substances.
C. Total parenteral nutrition.
D. Hemodialysis.
E. Placement of a temporary transvenous pacing wire.
F. Procurement of venous access when peripheral vein cannulation is not possible.
G. Aspiration of air in surgical procedures considered high risk for venous air embolism (e.g., posterior fossa craniotomy with the patient in the sitting position).
H. Venous access during cardiopulmonary resuscitation.
III. PROCEDURES
A. Universal protocol with a time-out must be followed.
B. IJV approach.
1. Approaches to IJV cannulation are the anterior, central, and posterior (Fig. 2-1).
2. Central (Fig. 2-1C).
a. The patient is placed in a 15-degree Trendelenburg position, and the head is turned to the contralateral side.
b. Using maximal barrier precautions, after infiltration of local anesthetic, the operator punctures the skin with a 22-gauge “finder” needle with an attached syringe at the apex of the triangle formed by the sternal and clavicular heads of the sternocleidomastoid muscle (SCM) and the clavicle (base). The internal carotid artery pulsation is usually felt 1 to 2 cm medial to this point.
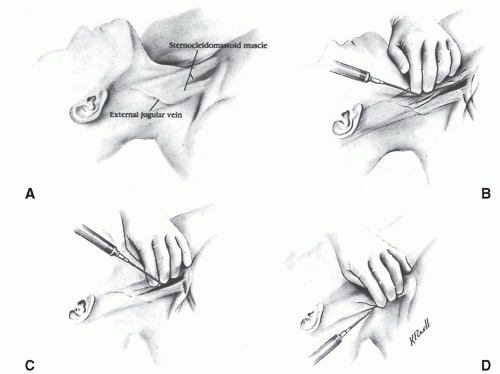 Figure 2-1. A:
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|



