CHAPTER 102
Carpal Tunnel Syndrome
Presentation
The patient complains of pain, tingling, or a “pins and needles” sensation in the hand or fingers. Onset may have been abrupt or gradual, but the problem is most noticeable after extended use of the hand or when driving or holding up a newspaper. Symptoms are usually worse at night and commonly awaken the patient. Sports such as racquetball and handball or activities such as assembly-line work and use of vibratory tools (e.g., jackhammers) are frequently associated with carpal tunnel syndrome (CTS). CTS has also been associated with a number of systemic conditions, including rheumatoid arthritis, diabetes, hypothyroidism, acromegaly, gout, renal failure, obesity, pregnancy, and menopause. The sensation may be bilateral, may include pain in the wrist or forearm, and is usually ascribed to the entire hand until specific physical examination localizes it to the median nerve distribution. Strenuous use of the hand almost always aggravates the symptoms. To relieve the symptoms, patients often “flick” their wrist as if shaking down a thermometer (flick sign). More established cases may include weakness of the thumb and atrophy of the thenar eminence. Although one hand typically has more severe symptoms, both hands often are affected.
Physical examination localizes paresthesia and decreased sensation to the median nerve distribution (which may vary) (Figure 102-1). Motor weakness, if present, is localized to intrinsic muscles with median innervation. Innervation varies widely, but the muscles most reliably innervated by the median nerve are the abductors and opponens of the thumb (Figure 102-2). CTS typically occurs after 30 years of age and is 3 times more common in women than in men.
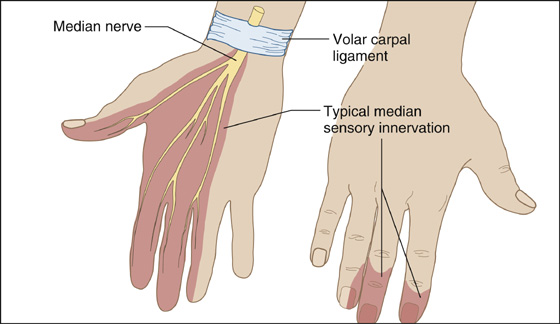
Figure 102-1 Sensory abnormalities are found along the median nerve distribution.
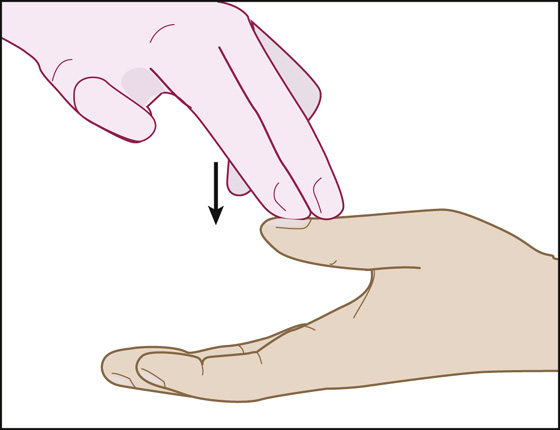
Figure 102-2 Testing thumb abduction.
What To Do:
 Perform and document a complete examination, sketching the area of decreased sensation and grading (on a scale of 1 to 5) the strength of the hand. One clinical finding that best identifies patients with electrodiagnostic studies that are positive for CTS is hypalgesia (diminished perception of painful stimuli) along the palmar aspect of the index finger, compared with the ipsilateral little finger. Another typical finding is weakness of resistance to downward pressure applied to the distal phalanx of the thumb, while the patient rests the dorsal surface of her hand on a hard surface with the thumb raised perpendicular to her palm (see Figure 102-2).
Perform and document a complete examination, sketching the area of decreased sensation and grading (on a scale of 1 to 5) the strength of the hand. One clinical finding that best identifies patients with electrodiagnostic studies that are positive for CTS is hypalgesia (diminished perception of painful stimuli) along the palmar aspect of the index finger, compared with the ipsilateral little finger. Another typical finding is weakness of resistance to downward pressure applied to the distal phalanx of the thumb, while the patient rests the dorsal surface of her hand on a hard surface with the thumb raised perpendicular to her palm (see Figure 102-2).
 Although the Tinel sign and a positive Phalen maneuver are classic clinical signs of CTS, their actual utility in the diagnosis has been less clear.
Although the Tinel sign and a positive Phalen maneuver are classic clinical signs of CTS, their actual utility in the diagnosis has been less clear.
 Have the patient passively drop both wrists to 90 degrees of flexion for 60 seconds to see if this reproduces symptoms. This is known as the Phalen test (Figure 102-3); it is more sensitive than the reverse (hyperextending the wrist), and more specific than tapping over the volar carpal ligament to elicit paresthesia in the distribution of the median nerve (Tinel sign).
Have the patient passively drop both wrists to 90 degrees of flexion for 60 seconds to see if this reproduces symptoms. This is known as the Phalen test (Figure 102-3); it is more sensitive than the reverse (hyperextending the wrist), and more specific than tapping over the volar carpal ligament to elicit paresthesia in the distribution of the median nerve (Tinel sign).
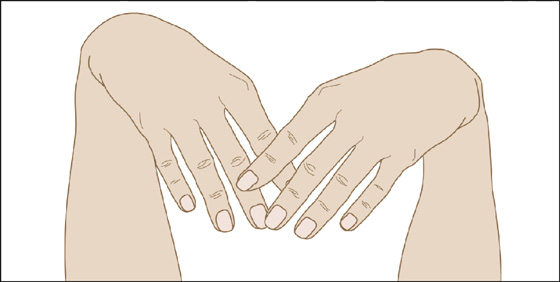
Figure 102-3 The Phalen test.
 The hand elevation test is comparable in accuracy to the Phalen test and only requires the patient to hold her arm over her head as high as comfortably possible. Reproduction of CTS symptoms within 1 minute is considered a positive test.
The hand elevation test is comparable in accuracy to the Phalen test and only requires the patient to hold her arm over her head as high as comfortably possible. Reproduction of CTS symptoms within 1 minute is considered a positive test.
 Patients should be told to avoid repetitive wrist and hand motions that may exacerbate symptoms or make symptom relief difficult to achieve. If possible, they should not use vibratory tools (e.g., jackhammers, floor sanders).
Patients should be told to avoid repetitive wrist and hand motions that may exacerbate symptoms or make symptom relief difficult to achieve. If possible, they should not use vibratory tools (e.g., jackhammers, floor sanders).
 Wrist splints that maintain the wrist in a neutral position may be helpful for patients who engage in repetitive wrist motion often.
Wrist splints that maintain the wrist in a neutral position may be helpful for patients who engage in repetitive wrist motion often.
 A 4-week course of oral prednisone (e.g., 20 mg daily for 2 weeks, then 10 mg qd for another 2 weeks) may offer short-term relief in mild to moderate cases.
A 4-week course of oral prednisone (e.g., 20 mg daily for 2 weeks, then 10 mg qd for another 2 weeks) may offer short-term relief in mild to moderate cases.
 Alternatively, injections of corticosteroids can often dramatically alleviate symptoms and may improve symptoms for a longer period. When combined with a local anesthetic, such injections can be diagnostic as well as therapeutic. Using a 1-inch, 25-gauge needle with 20 mg of methylprednisolone (Depo-Medrol) or 0.5 mL of betamethasone (Celestone Soluspan) along with 5 mL of bupivacaine (Marcaine), 0.25%, with the hand positioned on a rolled towel, inject on the ulnar side of the palmaris longus tendon, which is midway between the flexor carpi radialis and the flexor carpi ulnaris tendons, just proximal (1 cm) to the flexor crease of the wrist, distally into the central portion of the flexor tendon mass (Figure 102-4). The palmaris longus tendon can be identified by having the patient pinch the thumb and fifth fingers together while slightly flexing the wrist. Avoid injecting either the median or ulnar nerve or radial or ulnar artery. If injection produces paresthesia in the distribution of the median or ulnar nerve, withdraw the needle and redirect it to avoid intraneural injection. If the patient gets immediate relief of her symptoms, the diagnosis of CTS is very likely. When the local anesthetic wears off and after 1 day of wrist splinting, the patient can expect symptomatic relief, but the maximum effect may not come until a few days later. Warn the patient that her hand will feel somewhat numb for a few hours, and that a rebound phenomenon or flare may develop within 12 hours after the injection. Nonsteroidal anti-inflammatory drugs (NSAIDs), elevation, and ice packs will help if this rebound pain occurs.
Alternatively, injections of corticosteroids can often dramatically alleviate symptoms and may improve symptoms for a longer period. When combined with a local anesthetic, such injections can be diagnostic as well as therapeutic. Using a 1-inch, 25-gauge needle with 20 mg of methylprednisolone (Depo-Medrol) or 0.5 mL of betamethasone (Celestone Soluspan) along with 5 mL of bupivacaine (Marcaine), 0.25%, with the hand positioned on a rolled towel, inject on the ulnar side of the palmaris longus tendon, which is midway between the flexor carpi radialis and the flexor carpi ulnaris tendons, just proximal (1 cm) to the flexor crease of the wrist, distally into the central portion of the flexor tendon mass (Figure 102-4). The palmaris longus tendon can be identified by having the patient pinch the thumb and fifth fingers together while slightly flexing the wrist. Avoid injecting either the median or ulnar nerve or radial or ulnar artery. If injection produces paresthesia in the distribution of the median or ulnar nerve, withdraw the needle and redirect it to avoid intraneural injection. If the patient gets immediate relief of her symptoms, the diagnosis of CTS is very likely. When the local anesthetic wears off and after 1 day of wrist splinting, the patient can expect symptomatic relief, but the maximum effect may not come until a few days later. Warn the patient that her hand will feel somewhat numb for a few hours, and that a rebound phenomenon or flare may develop within 12 hours after the injection. Nonsteroidal anti-inflammatory drugs (NSAIDs), elevation, and ice packs will help if this rebound pain occurs.
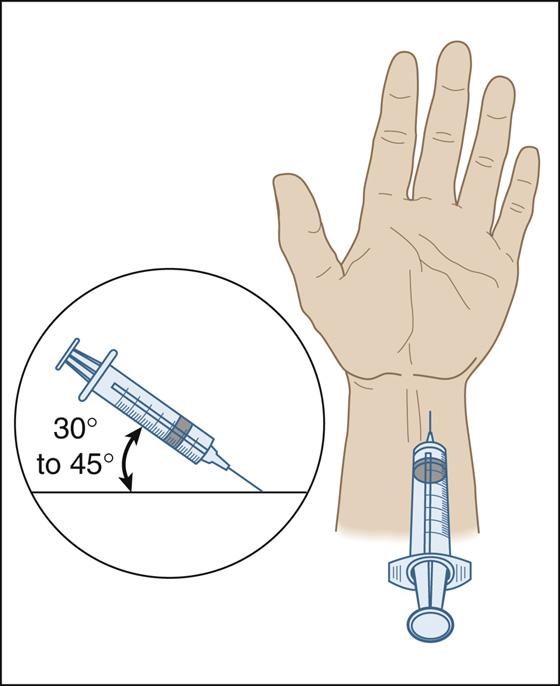
Figure 102-4 Location for needle insertion.
 If the first injection is successful, a repeat injection can be considered after a few months. Surgery should be considered if a patient needs more than two injections.
If the first injection is successful, a repeat injection can be considered after a few months. Surgery should be considered if a patient needs more than two injections.
 Explain the nerve-compression causative factor to the patient and arrange for additional evaluation and follow-up.
Explain the nerve-compression causative factor to the patient and arrange for additional evaluation and follow-up.
 Borderline diagnoses may be established with electrodiagnostic studies (nerve conduction and electromyography [EMG]), but they have significant false-positive and false-negative results. If symptoms are refractory to the above conservative measures or if nerve conduction studies show severe entrapment, surgical referral for open or endoscopic carpal tunnel release may be necessary.
Borderline diagnoses may be established with electrodiagnostic studies (nerve conduction and electromyography [EMG]), but they have significant false-positive and false-negative results. If symptoms are refractory to the above conservative measures or if nerve conduction studies show severe entrapment, surgical referral for open or endoscopic carpal tunnel release may be necessary.
 Carpal tunnel syndrome should be treated conservatively in pregnant women, because spontaneous postpartum resolution is common.
Carpal tunnel syndrome should be treated conservatively in pregnant women, because spontaneous postpartum resolution is common.
What Not To Do:
 Do not rule out thumb weakness just because the thumb can touch the little finger. Thumb flexors may be innervated by the ulnar nerve.
Do not rule out thumb weakness just because the thumb can touch the little finger. Thumb flexors may be innervated by the ulnar nerve.
 Do not diagnose carpal tunnel syndrome solely on the basis of a positive Tinel sign. Paresthesia can be produced in the distribution of any nerve if one taps hard enough.
Do not diagnose carpal tunnel syndrome solely on the basis of a positive Tinel sign. Paresthesia can be produced in the distribution of any nerve if one taps hard enough.
 Do not perform the Phalen test for more than 60 seconds; maintaining a flexed wrist for longer may produce paresthesia in a normal hand.
Do not perform the Phalen test for more than 60 seconds; maintaining a flexed wrist for longer may produce paresthesia in a normal hand.
 Do not prescribe or recommend NSAIDs, pyridoxine (vitamin B6), diuretics, or chiropractic therapy. They have been shown to be no more effective than a placebo in relieving the symptoms of CTS.
Do not prescribe or recommend NSAIDs, pyridoxine (vitamin B6), diuretics, or chiropractic therapy. They have been shown to be no more effective than a placebo in relieving the symptoms of CTS.
Discussion
Carpal tunnel syndrome is one of the most common causes of hand pain, particularly in middle-aged women. There is little space to spare where the median nerve and digit flexors pass beneath the volar carpal ligament, and very little swelling may produce this specific neuropathy. There is no single reference standard for the diagnosis of CTS. Whether carpal tunnel syndrome is a clinical or electrophysiologic diagnosis remains somewhat controversial. Professional consensus committees have recognized nerve conduction studies as the diagnostic standard for CTS. It must still be appreciated that although electrodiagnostic studies may assist in confirming the diagnosis, they unfortunately have significant false-positive and false-negative results.
Although most cases are idiopathic or the result of nonspecific flexor tenosynovitis, CTS is also associated with trauma and a number of systemic conditions previously mentioned. There is also strong evidence of a positive association of CTS with exposure to forceful work and repetition—for example, in meat packers, poultry processors, and automobile assembly workers.
Although the incidence of diagnosed CTS has increased during the past 20 years, and public attention has focused on excessive keyboard use, frequent computer use has not yet been established as a cause of CTS. Although 30% of frequent computer users complain of hand paresthesias, only 10% meet clinical criteria for carpal tunnel syndrome, and nerve conduction studies are abnormal in only 3.5% of these persons.
Usually, the initial diagnosis of CTS is made on clinical grounds. Because about 50% will resolve spontaneously, not all need to be referred for nerve conduction studies or surgical assessment.
Patients with mild symptoms should be offered conservative treatment. In those cases clearly related to occupational job tasks, such as highly repetitive forceful work or work involving hand and wrist vibration, the patient should be advised to modify the activities or movements that caused the CTS.
Splinting is a low-cost option that may provide benefit and certainly warrants an initial trial. Compared with nighttime-only splint use, full-time use has been shown to provide greater improvement of symptoms and electrophysiologic measures; however, compliance with full-time use is more difficult.
Steroid injection and, to a lesser extent, oral corticosteroids provide the most effective nonsurgical treatment.
Surgical referral should be considered in patients with symptoms that are causing persistent sleep disturbance, interfering with their ability to work, or otherwise adversely affecting their lifestyle.
Less often, the median nerve can be entrapped more proximally, where it enters the medial antecubital fossa through the pronator teres. Symptoms of this type of entrapment syndrome may be reproduced with elbow extension and forearm pronation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


