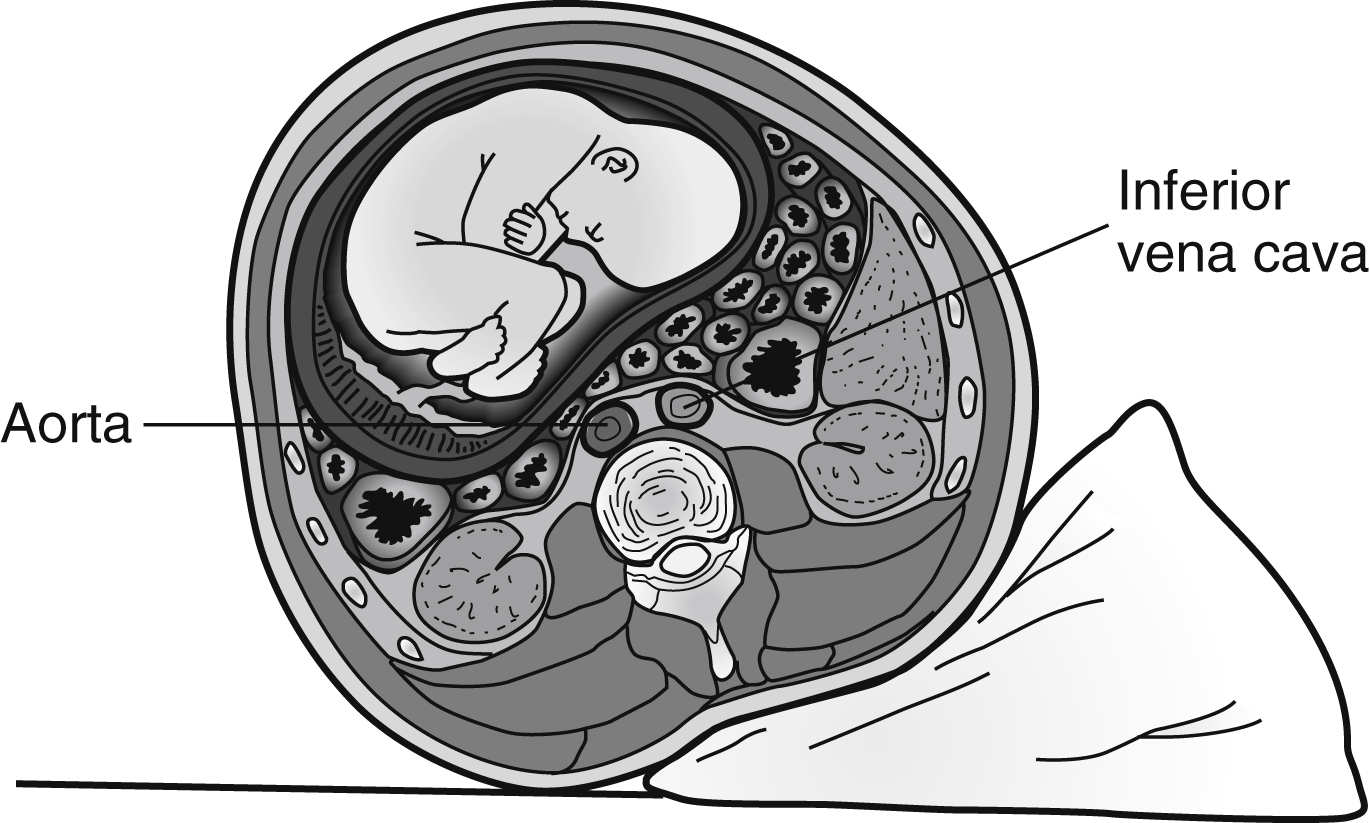
FIG. 51.1 Cross section of lower abdomen (nonpregnant). (From Lampignano JP, Kendrick L: Bontrager’s textbook of radiographic positioning and related anatomy, ed 9, St. Louis, MO, 2018, Elsevier.)
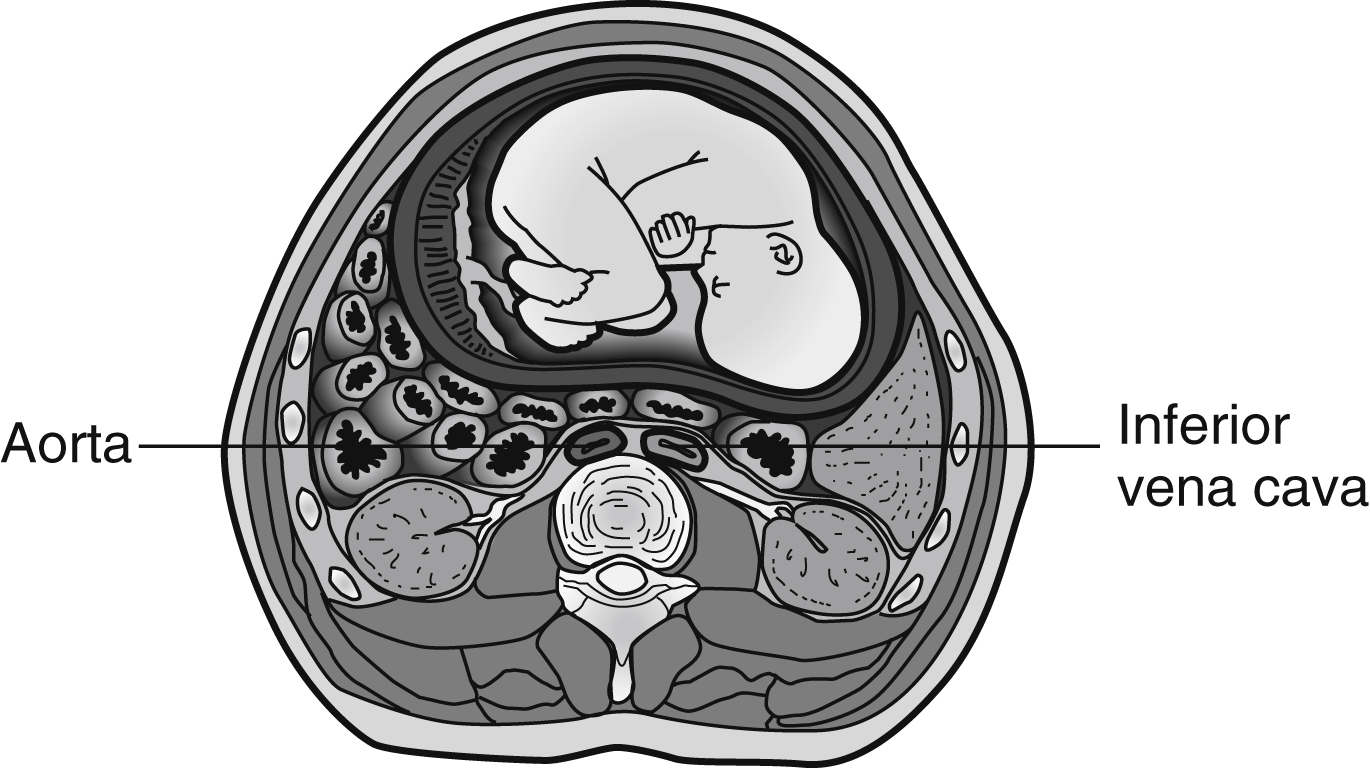
FIG. 51.2 Pregnant uterus compressing aorta and inferior vena cava (aortocaval compression). Patient is in supine position. (From Lowdermilk DL, Perry SE, Cashion K, et al.: Maternity and women’s health care, ed 11, St. Louis, MO, 2016, Elsevier.)
Collateral circulation for venous return develops through the intervertebral venous plexus and the azygos vein. This condition reduces the volume of the epidural and subarachnoid spaces; therefore, the amount of drug during regional anesthesia should be decreased. With this in mind, the perianesthesia nurse should assess the patient upon admission for a high block and monitor dermatome levels frequently thereafter (see Chapter 25).6
In the nonpregnant patient, the sympathetic nervous system plays a role in promoting venous return to the heart from the lower extremities. This sympathetic stimulation of vasomotor tone is enhanced during pregnancy in an effort to counteract the negative effects of uterine compression of the vena cava. Clinically, this protective mechanism is abolished with spinal or epidural anesthesia because it acts as a pharmacologic sympathectomy. Without an appropriate preload of fluids (500 to 1000 mL IV lactated Ringer solution), the pregnant patient could have a 30% to 50% decrease in blood pressure during the anesthesia. The pregnant patient must receive an appropriate preload of fluids before epidural or spinal anesthesia. Hemodynamic stability can be secured with the infusion of 15 mL/kg of colloid solution or 30 mL/kg of crystalloid solution. If the patient is to receive an inhalation anesthetic agent such as isoflurane or sevoflurane, similar fluid preloading is given because the inhalation anesthetic agents produce peripheral vasodilation.7
This increased fluid requirement has significant implications for the perianesthesia care of the pregnant patient. Consequently, the patient’s cardiac and hydration status must be monitored closely throughout the emergence phase of regional anesthesia (see Chapter 25).7,8
Hematologic Alterations
Blood volume, along with the number of platelets, fibrinogen levels, and the level of activity of several clotting factors (VII, VIII, IX, X, and XII), increases by 15% during the first trimester, rises rapidly during the second trimester to 50% above the pregnant levels, and changes little during the remainder of the pregnancy and suggests that pregnancy is a hypercoagulable state.7,8 However, a smaller rise in the number of circulating red blood cells occurs. This difference results in lower hematocrit and hemoglobin levels (see Box 51.1), although red blood cell mass actually increases. This condition is known as physiologic anemia of pregnancy.7,8
The plasma concentration of the enzyme cholinesterase is decreased during pregnancy. Due to the changes in coagulation and fibrinolytic activity, the perianesthesia nurse should monitor the pregnant patient for thromboembolism and use bilateral lower extremity compression devices. Plasma cholinesterase is also involved in the destruction of the depolarizing muscle relaxant succinylcholine. The recovery time from succinylcholine is unaltered and in fact may be somewhat faster in pregnant women, which is explained by the fact that the volume distribution of succinylcholine increases during pregnancy because of an elevation in the plasma volume. In the immediate postpartum period, the plasma cholinesterase concentration and the plasma volume distribution are further reduced.7–10
Respiratory Changes
Upper Airway Anatomy
During pregnancy, capillary engorgement of the upper respiratory tract includes the nasal and oropharyngeal mucosa and larynx, and pregnant women may have nasal stuffiness. In addition, nose breathing is difficult and nosebleeds can occur. This capillary engorgement of the respiratory mucosa during pregnancy predisposes the upper airways to trauma, bleeding, and obstruction. Gentle laryngoscopy and small endotracheal tubes (6 to 6.5 mm) should be used during general anesthesia.7–10
Lung Mechanics and Ventilation
The diaphragm elevates and the rib cage flares; therefore, at term, 85% of respiratory effort is intercostal and 15% diaphragmatic (normally, approximately 70% is intercostal and 30% is diaphragmatic). Because of the mechanical changes in the lungs and chest wall, the lung volumes and capacities change during pregnancy. Overall, the inspiratory lung volumes and capacities moderately increase, and the expiratory lung volumes and capacities decrease. The inspiratory reserve volume and the inspiratory capacity increase by 5% to 15%. The functional residual capacity (FRC) decreases by approximately 20% to 60%. The residual volume and expiratory reserve volume, which compose the FRC, are decreased. The combination of decreased FRC and increased oxygen consumption promotes rapid oxygen desaturation during periods of apnea.7–10
The tidal volume also increases 20% to 45%, and the respiratory rate does not change, which leads to a 30% to 45% increase in the alveolar ventilation and the minute ventilation. Therefore, during pregnancy, the arterial oxygen level ranges from 95 to 105 mm Hg, and the arterial carbon dioxide level is approximately 30 mm Hg, with an arterial pH of 7.44. Consequently, the pregnant patient has some respiratory alkalosis for which the renal excretion of bicarbonate compensates. As a result, the normal bicarbonate level during pregnancy is approximately 19 mEq/L, and the base excess is reduced by 2 mEq/L.7–10
Limited information exists regarding the effects of pregnancy on characteristics of the central chemoreflex control of breathing. Some studies suggest that the increased circulation of hormones, particularly progesterone and estradiol, significantly lowers the threshold and increases the sensitivity of the central ventilatory chemoreflex response to CO2. With regard to flow rate changes, the forced expiratory volume in 1 second and the flow-volume loop remain unchanged. In addition, the closing capacity (see Chapter 12) does not change during gestation.7–10 Consequently, the conductance and resistance of the small and large airways do not change during pregnancy.
Gastrointestinal Changes
Motility and Secretions
Gastric emptying slows during pregnancy because the stomach is displaced as the uterus enlarges, which leads to gastroesophageal reflux and esophagitis during pregnancy. All parturients have a gastric pH less than 2.5, and more than 60% have gastric volumes greater than 25 mL. The gastric volume also increases during hours 1 to 8 in the postpartum period; therefore, the perianesthesia nurse must be cognizant of the potential for vomiting and aspiration, particularly in patients who have had general anesthesia. Muscle relaxants may have been used and can result in the patient’s normal protective mechanisms being obtunded. Again, the side-lying position becomes of significant importance.7–10
Hepatic System
Renal Changes
Early in pregnancy, the kidneys receive an increased blood flow because of renal vasodilation, and glomerular filtration and urine formation rates increase. This increase is necessary to handle the increased amount of waste products produced. Monitoring of output should reflect this expected increase in volume. Intervention may be necessary for hypovolemia even though the urine output is within ranges acceptable in a nonpregnant patient.7–10
Loss of glucose in the urine is not uncommon or necessarily pathogenic during pregnancy but is merely a reflection of the kidney’s inability to reabsorb all of the glucose filtered by the glomeruli. This observation, combined with anatomic changes leading to ureteral atonia and stasis of urine in the ureters, increases the risk for urinary tract infection in the pregnant patient.
Care of the Obstetric Patient
Because the effects of anesthesia have such a profound effect on the emergence of the pregnant patient, a complete review of the techniques and procedures of general and regional anesthesia is presented.
Positioning
The supine position causes a reduction in uterine blood flow in the pregnant patient; therefore, the semi-Fowler position is used when possible. To prevent aortocaval compression, the patient is placed in the lateral decubitus position and the right hip is elevated with a pillow, or the uterus is displaced to the left with devices on the operating table.11,12
Gastrointestinal Considerations
The pregnant patient has a reduced gastric emptying time and a reduced gastric pH. Research has shown that gastric volume and acidity in the pregnant patient do not differ significantly from those in the nonpregnant patient. However, many anesthesia clinicians strongly believe that the pregnant patient, especially the patient with pyrosis (heartburn), is at risk of developing aspiration pneumonitis. Consequently, preoperative pharmacologic interventions are usually taken. Drugs that can be administered include a nonparticulate antacid such as 30 mL of 0.3 mmol/L sodium citrate (Bicitra) to increase the gastric pH; famotidine or 50 mg ranitidine (Zantac), which are histamine-2 receptor blockers that reduce gastric acid secretion; and 10 mg metoclopramide (Reglan), which accelerates gastric emptying time and elevates lower esophageal tone. 5HT3 antagonists (e.g., ondansetron) treat nausea and vomiting by blocking serotonin, a natural substance produced by the body that cause nausea and vomiting.13–15
General Anesthesia
Induction
Because of the strong full-stomach considerations, the pregnant patient is intubated with a rapid-sequence endotracheal intubation technique (see Chapter 30) that includes IV propofol, etomidate, or ketamine followed by succinylcholine. A defasciculation dose of a nondepolarizing muscle relaxant can be given before the administration of the succinylcholine to avoid the increase in intragastric pressure. Some clinicians do not administer a defasciculating dose of a nondepolarizing muscle relaxant because most pregnant patients do not have fasciculation after succinylcholine. Cricoid pressure (Sellick maneuver) is applied with an assistant’s thumb and index fingers exerting downward pressure on the cricoid cartilage to displace the cartilaginous cricothyroid ring posteriorly and thus compress the underlying esophagus against the cervical vertebrae.16–19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree