FIG. 44.1 Sutured bolster dressing. (From Adams DC, Ramsey ML: Grafts in dermatologic surgery: review and update on full- and split-thickness skin grafts, free cartilage grafts, and composite grafts. Dermatol Surg 31:1055−1067, 2005.)
Flaps
The term flap commonly refers to a skin flap; however, with recent advances in reconstructive surgery, flaps are not limited to skin tissue. Flaps are classified by anatomic composition: skin with muscle fascia or bone or both, skin alone, omentum, or a composite of these tissues. The term flap implies maintenance of vascularity from the original location of harvest, unlike transplantation, which implies complete separation from the original vascular site.
Pedicle flaps are the preferred surgical treatment method for covering wounds having inadequate vascularity to support a skin graft; the reconstruction of full-thickness defects of specialized body parts such as ears, eyelids, nose, and lips; and concealment of gliding tendons. Reconstructions that require tissue bulk, such as decubitus ulcer closure, may also involve skin flap placement.
Microvascular Tissue Transfer and Free Flaps
Microvascular tissue transfer represents an important advancement in the field of reconstructive surgery. This technique requires the use of a high-magnification operative microscope for reestablishment of vasculature. Regardless of the type of flap used, the newly positioned tissue is kept under constant observation by perianesthesia nursing personnel. Postanesthesia nursing management of the patient who has undergone microsurgery is consistent with established care requirements for the specific procedure performed, with emphasis on notation of color changes in the skin at the operative site.
The most serious complication in a microvascular tissue transfer procedure is tissue necrosis. Tissue death occurs when the artery or the vein that supplies the flap develops a thrombus. Arterial thrombosis can result in complete flap failure within 4 hours of onset. Arterial occlusion is characterized by a pale cool flap that does not bleed when stuck with a needle. Hematomas can form at the recipient site and occur more commonly in the patient who preoperatively smokes or uses nonsteroidal antiinflammatory drugs or corticosteroids.9
Venous thrombosis is more commonly encountered but is not an immediate threat. Thrombosis is characterized by a congested warm mottled flap that continuously oozes dark blood. Objective assessment of the flap is possible with fluorometry, transcutaneous oxygen tension, thermometry, laser Doppler scan, temperature monitoring, buried Doppler probe, or photoplethysmograph disk for monitoring of blood flow. Any change in skin color from the normal baseline assessments that indicate imminent occlusion should be reported to the surgeon immediately. A donor site typically generates more painful stimuli than the transplanted skin graft or flap site.10 Pain management should be individualized and based on the patient’s self-reported pain levels. Nursing care should include administration of analgesics and selected nonopioid adjuvants with attention to comfort measures as needed.
Breast Reconstruction Flap Techniques
Breast cancer affects millions of women around the world each year, and reconstruction after mastectomy has become a routine part of breast cancer treatment.2,9,11 Breast reconstruction using autologous grafting produces a more natural appearance,12 is commonly accomplished in several ways, does not adversely affect cancer survival rates, and can serve to enhance the patient’s psychological state.2 The transverse rectus abdominis musculocutaneous (TRAM) flap procedure involves the reconstruction of a breast with autografting of lower abdominal muscle, skin, and adipose tissue. The procedure can be performed using a pedicle TRAM flap or a free TRAM flap (Fig. 44.2). The pedicle TRAM procedure was first developed in the early 1980s. Through improved understanding of flap physiology and surgical techniques, common procedural options have evolved to include the use of a free TRAM flap, muscle-sparing free TRAM flap, and deep inferior epigastric artery perforator (DIEP) flap. Muscle resection has frequently resulted in an abdominal bulge, abdominal hernia, and some degree of permanent loss of the patient’s abdominal strength. Surgeons performing the TRAM technique may choose to implant propylene mesh at the time of resection to better support the abdominal wall.7,13 The DIEP reconstructive procedure involves a rectus abdominis muscle incision but leaves the muscle completely intact while elevating subcutaneous abdominal fat and skin to achieve the breast graft. The untoward abdominal muscle findings previously described occur at a lower incidence rate in the DIEP patient population.7,9
A newer microsurgical procedure, the superficial inferior epigastric artery (SIEA) flap, provides an abdominal muscle-sparing alternative by creating the donor flap without performing rectus muscle dissection or incision.12 Another procedure available for use in autologous breast reconstruction is the latissimus dorsi flap (LD) technique. The LD flap procedure is especially useful in the low body mass index patient who lacks the abdominal tissue reserves needed for flap harvest.13 It is harvested by using a myocutaneous flap or with the use of muscle alone and often reconstructed in combination with an implant.12 As with all postoperative flap procedures, nursing care of the postoperative breast reconstruction patient centers on observation of the graft site in addition to general perianesthetic breast surgery patient care (see Chapter 43).
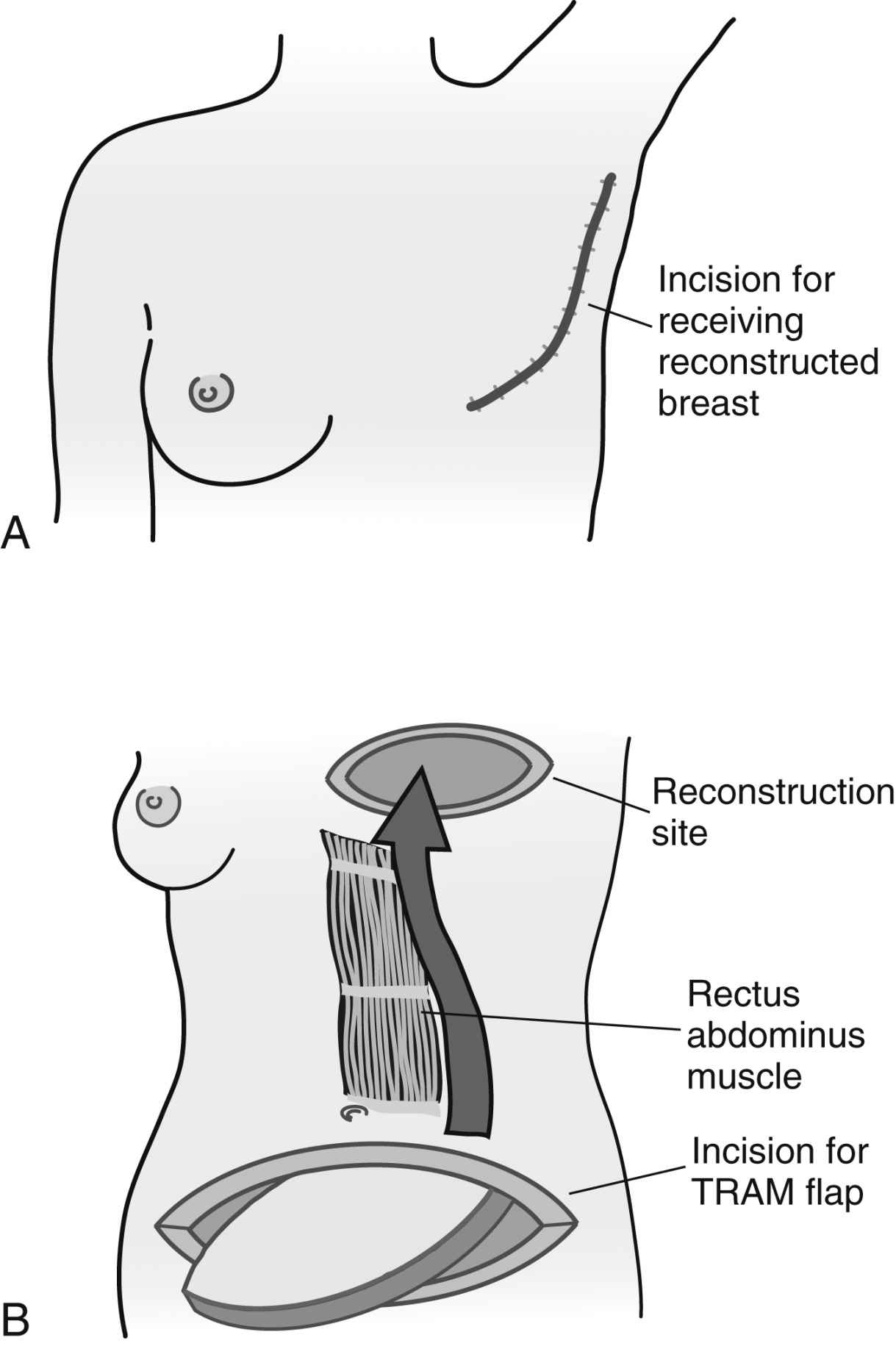
FIG. 44.2 Transverse rectus abdominis myocutaneous (TRAM) flap. A, After mastectomy of the involved breast and, B, a breast is reconstructed using the lower abdominal skin and fatty tissue. In a pedicled TRAM, the tissue’s own blood supply remains attached, and the lower abdominal tissue is rotated into position on the chest. The tissue is tunneled under the skin to the chest area, where it is brought through the mastectomy incision. The reconstructed tissue is shaped to form a matching breast and placed in the mastectomy skin pocket. A free TRAM flap refers to using skin and tissue that are completely disconnected from their blood supply, moved from the abdomen to the new site, and reconnected to different blood vessels. A nipple and areola can be tattooed on later after healing has taken place. (From Goodman CC, Fuller KS: Pathology: implications for the physical therapist, ed 4, St. Louis, MO, 2015, Elsevier.)
Bone Grafts
After bone grafting has been performed, the graft site must be immobilized and excessive movement of the patient should be avoided. The donor site is generally the greater source of postoperative discomfort over the graft site.10 Pain should be anticipated and aggressively managed with opioid analgesics. If split-rib grafts are used, respiratory status should be frequently assessed, and any signs of possible pneumothorax, such as tachycardia and tachypnea, should be reported immediately to the surgeon. Ice often is applied for reduction of swelling and pain management, and the graft site may necessitate elevation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








