From Kliegman RM, et al.: Nelson’s textbook of pediatrics, ed 20, Philadelphia, PA, 2016, Elsevier.
Neonates have large heads and chest circumferences that mostly equal their body length. They can begin to lift their heads when lying prone and are obligate nose breathers until about the age of 4 months. Neonates have soft palpable fontanels and generally sleep about 18 to 20 hours per day. Although hearing and touch are well developed, their vision is poor. They show preference to their mother’s voice.
Infant: 1 to 12 Months
The first year of life is a time of significant growth and development. Infants are still creating identity through trust with the primary caregiver, and intrinsic reflexes start to disappear by 2 to 3 months.
Infants will double their birth weights by 5 months and triple it by the end of their first year. By 4 months, they are visually tracking, opening their hands, exploring their feet, and putting hand to mouth. The posterior fontanel closes, and they are beginning to hold their head up.2
By 6 months, infants can roll from stomach to back, sit with support, as well as push up with their arms. Six-month-old infants can grasp and release objects and develop the ability to transfer objects from one hand to the other as well as reaching with one hand.3 They are starting to sleep through the night with one to two naps during the daytime.
By 9 months, infants can stand and sit alone without help. They can crawl as well as initiate standing while holding onto furniture.2,3 They can imitate the game of “peek-a-boo” and “pat-a-cake” as well as follow simple commands such as “come here” and “give it to me.” The pincher grasp is more developed, and they try to put everything into their mouths. Some infants transition to solid foods at this time.
By 12 months or 1 year, infants are cruising, standing alone, and attempting to take steps without holding on. They are clapping hands and waving goodbye. Language is beginning to develop with vocalization of primitive words.2
By the end of the first year, there is an amazing transformation as the 1-year-old has mastered many physical tasks such as holding objects, reaching for objects, stepping, and cruising as well as attempting to feed self and hold cups. At this age, children recognize their parents’ voices, familiar faces, and their own names. They smile at people but are developing stranger anxiety and become upset when parents leave their immediate vicinity.4
Toddler: 1 to 3 Years
Toddlers continue to change and develop quickly as they become increasingly independent, preferring to do things on their own. Reflex and repetitive actions are now replaced by imitation actions, and they are starting to understand the concept of cause and effect. However, toddlers have not mastered the idea of sharing—their play is side-by-side or parallel and not actually “with” another child.
Toddlers are gaining more bodily control such as the ability to toilet train but will still use arms to help balance as well as plant feet wide apart to increase stability. At 1 year, toddlers have a head circumference equal to their chest as well as one to eight teeth.4
Toddlers can climb stairs and jump. They are constantly exploring the environment they are in, which can sometimes present a safety concern if the area is not child-proofed or if they are not watched diligently. By 18 months they can walk up and down stairs, feed self, and say 4 to 20 words.2,3 Toddlers want immediate gratification, frequently use the word “no,” and display frequent tantrums when trying to deal with frustration.2
Preschool: 3 to 5 Years
Preschool is a time when children are learning to assert their own power as they begin to engage in social activity and gain a sense of self-confidence. Even though they are beginning to learn and understand rules and appropriate social behavior, they may still use egocentric language such as bragging or boasting as well as show aggression when frustrated.
Physical growth does slow down but continues at a steady pace. Height doubles from birth to 4 years. Preschoolers can dress themselves and show hand dominance as they start to use crayons, pencils, and scissors as well as string beads together.2–4
Preschoolers understand the concept of time such as today or tomorrow and have started to recognize the difference in the sexes as well as identifying with their same-sex parent through imitation. They can identify and name body parts, numbers, colors, and letters and can identify their own sex.3,4 They need caregivers to provide consistency and discipline in the same manner.
School Age: 5 to 13 Years
School age is when children enjoy working in groups with each other, begin to develop social relationships, and learn to follow rules and guidelines. There is a developing sense of competition as well as the beginning of logical thinking, sorting of facts, and problem solving. Physically, long bones are growing faster than muscles and ligaments, which makes them more prone for fractures. Overall growth continues to slow down, but height may increase about 2 inches per year, and weight can double between the ages of 6 to 12 years. Vision matures by age 6 years. Fine motor skills continue to develop as children learn to play sports and musical instruments.2
Attention span increases with age, and the school-age child understands concepts of permanence, cause and effect, partials and wholes, spelling, and reversibility. This is demonstrated with interest in playing cards and/or board games. Most children have mastered having a longer meaningful conversation. Magical thinking diminishes as cause-and-effect relationships are better understood.3
Throughout this time frame, there is an increased ability to listen and follow directions, and they learn to compromise and cooperate as well as play well with other children. It is a time of first friendships and teachers as a major influence in their lives as opposed to just parents.
Adolescent: 13 to 18 Years (Some Define Until Age 21 Years)
Adolescence is also a time of rapid growth and development. There are significant physical and emotional changes as well as major social development. Peer groups become increasingly important as adolescents start to pull away from adults to establish their own identities. Along with identity comes an increase in awareness of bodily changes—how they look and how others will view them. Sexual identity and feelings start to emerge and develop along with a tendency for labile emotions.
Adolescents gain the ability to think in more abstract concepts as well as develop logical conclusions from their own observations. They have an increased ability to analyze and synthesize information and the ability to use logic effectively to problem solve. It is a time to test limits as they test their hypotheses.2
Adolescents experience a rapid period of growth and development of secondary sex characteristics, sweat glands, sebaceous glands, and pubic hair. Menses, breast development, widened hips, and an increase in fatty tissue of the thighs, hips, and breasts occurs in females between the ages of 8 to 16 years. Males start to experience muscle mass enlargement, testicular enlargement, and nocturnal emissions. Masturbation with ejaculation is common.2
Adolescents may frequently daydream as a way to act out various social situations and are increasingly influenced by their peers and new fads. They may engage in high-risk behaviors such as smoking, sexual encounters, drug use, and motor vehicle accidents due to a sense of “invincibility.”2
The steps associated with moving from childhood to adulthood include (1) completing puberty and somatic growth; (2) developing socially, emotionally, and cognitively as they move away from concrete thinking to abstract thinking; (3) establishing an independent identity and separating from family; and (4) preparing for a career or vocation.5
Anatomic and Physiologic Considerations
Respiratory System
Understanding the differences between the adult and pediatric respiratory systems is essential to properly manage the pediatric airway. The leading cause of perioperative morbidity and mortality in children is hypoxemia.6 Pediatric airways have distinctions that make pediatric patients more susceptible to airway obstruction and hypoxemia.7–9 Respiratory distress will occur quickly in the pediatric patient if respiratory complications are not managed quickly and properly.8
Physiologic growth and development of the respiratory system extends from the neonatal period up to the age of 20; however, the majority of changes happen over the first 12 years of life. Much of lung and chest wall development occurs from 2 to 8 years of age. Infants have small nares, a large tongue, a small mandible, a short neck, and a large amount of upper airway lymphoid tissue.8,10 Children have proportionately larger heads in relation to their bodies throughout early childhood. This disproportionate weight distribution can lead to increase in neck flexion, making the child more at risk for airway obstruction when in the supine position.11,12
Newborns are considered obligate or preferential nose breathers until about the age of 4 months.9,10,13 The smaller nasal passages in young children can become easily obstructed by secretions or swelling. Any like situations that impede airflow in the nasal apertures of infants and children such as blood, edema, or specific surgical interventions can increase the work of breathing as well as problems in managing the pediatric airway. The pediatric airway overall has poorly developed cartilaginous integrity, which can lead to unintentional compression and obstruction due to is relaxed nature.12,14
In the newborn, the epiglottis is at the level of the first cervical vertebra (C1); however, the epiglottis usually moves down to the level of C3 by 6 months of age, which makes oral breathing more feasible.15 As children grow, the airway enlarges and moves more caudally as the C-spine elongates. Another important distinction is the narrowest point in the airway in adults is at the cords versus below the cords for children.14
The epiglottis of the infant and young pediatric patient is U-shaped versus the flatter shape in the adult. A straight laryngoscope blade may be more maneuverable in the pediatric airway and is most commonly used for intubation in pediatric patients. The tracheal length is relatively short in children, which makes proper placement and securing of the endotracheal tube critical to avoid bronchial intubation or accidental extubation)16 When the endotracheal tube is secured, and anytime the patient is repositioned, the presence of bilateral breath sounds and end-tidal carbon dioxide (ETCO2) should be reconfirmed.
Children have a more compliant trachea, larynx, and bronchi due to poor cartilaginous integrity. This allows for dynamic airway compression (i.e., a greater negative inspiratory force, which “sucks in” the floppy airway and decreases airway diameter). This in turn increases the work of breathing by increasing the negative inspiratory pressure generated.14
Historically, the shape of the child’s larynx has been thought to resemble that of an inverted cone, with the narrowest portion of the trachea residing at the cricoid cartilage.7,10,13,15 Recent research suggests that the narrowest portion of the pediatric trachea may actually be the glottis.9 No matter where the smallest diameter lies, the diameter of the endotracheal tube that can be used is limited. In addition, because the diameter of the pediatric airway is small, airway edema may lead to significant narrowing and potential occlusion of the airway.
Newborns are diaphragmatic breathers.9,10 The orientation of the ribs is horizontal in the infant; by 10 years of age, the orientation is downward. By the age of 3 years, most children’s ventilatory efforts are almost entirely the result of the movement of the diaphragm. In the pediatric patient, the sternum and anterior rib cage are compliant, and the intercostal and accessory muscles of respiration are poorly developed. The respiratory rates of infants and young children (Table 49.2) are faster than those of adults.9 This faster rate is a result of (1) the lung volumes in infants being extremely small in relation to their body size and (2) the higher metabolic rates in infants (oxygen consumption per unit body weight is double that of adults). This is the main reason that pediatric patients rapidly desaturate during short periods of hypoventilation or apnea.
The control of breathing in infants during the first several weeks of life differs significantly from that of the adult patient. As in the adult, the newborn’s primary drive to ventilation is carbon dioxide; however, hypoxemia depresses rather than stimulates respiration in the newborn.9 This secondary response is potentiated further by hypothermia, a condition that can occur at any point in the perioperative period. The respiratory rate rather than the tidal volume is increased in infants and small children because, ultimately, that strategy is more efficient.10
Table 49.2
Respiratory and Cardiovascular Age-Related Changes in Children
Modified from Davis PJ, et al.: Smith’s anesthesia for infants and children, ed 9, Philadelphia, PA, 2017, Elsevier.
Endotracheal tube and laryngeal mask airways have been used safely in children of all ages (Table 49.3). The advantages of endotracheal intubation include decreased dead space, avoidance of laryngospasm and gastric distention, and prevention of aspiration; however, the incidence rate of postintubation edema from trauma and infection may be increased. If the endotracheal tube is tight-fitting and compresses the tracheal mucosa, inflammation and edema may occur when it is removed, which reduces the luminal diameter and increases airway resistance (e.g., postextubation croup).17 The subglottic region in the infant is smaller than in the adult, so the same level of airway edema results in greater airway resistance in the infant. See Fig. 49.1 for relative effects of airway edema in an infant and an adult.
Upper respiratory tract infections can commonly occur due to several reasons. The respiratory tract is immature and, therefore, cannot produce enough mucus, which assists in warming, humidifying, and filtering inhaled air. Simple viral infections do not resolve for 6 to 8 weeks even if the child shows no signs of illness.18
Cardiovascular System
As the pediatric patient matures, the cardiovascular system undergoes substantial changes. Normally the respiratory rate and heart rate decrease with increasing age.9 Advancing age and increasing body size result in increases in the systolic and diastolic blood pressure. The cardiovascular age-related changes for newborns, infants, and children are summarized in Table 49.2. The newborn heart functions near its peak ventricular function and, therefore, has little cardiac reserve. Thus, in the newborn, heart rate plays a major role in determination of cardiac function.9 The newborn is relatively unable to compensate for suboptimal conditions such as hypoxemia, acidosis, or myocardial depression.9 With the advent of more sophisticated blood pressure monitoring devices, measurements in infants can be taken with greater accuracy. The pediatric patient ordinarily has the usual signs of impending shock or airway obstruction, but physiologic status deteriorates rapidly if the problem is not rectified quickly.7–10 The perianesthesia nurse should closely observe children for subtle changes in cardiovascular status. If abnormalities arise, prompt intervention is essential.
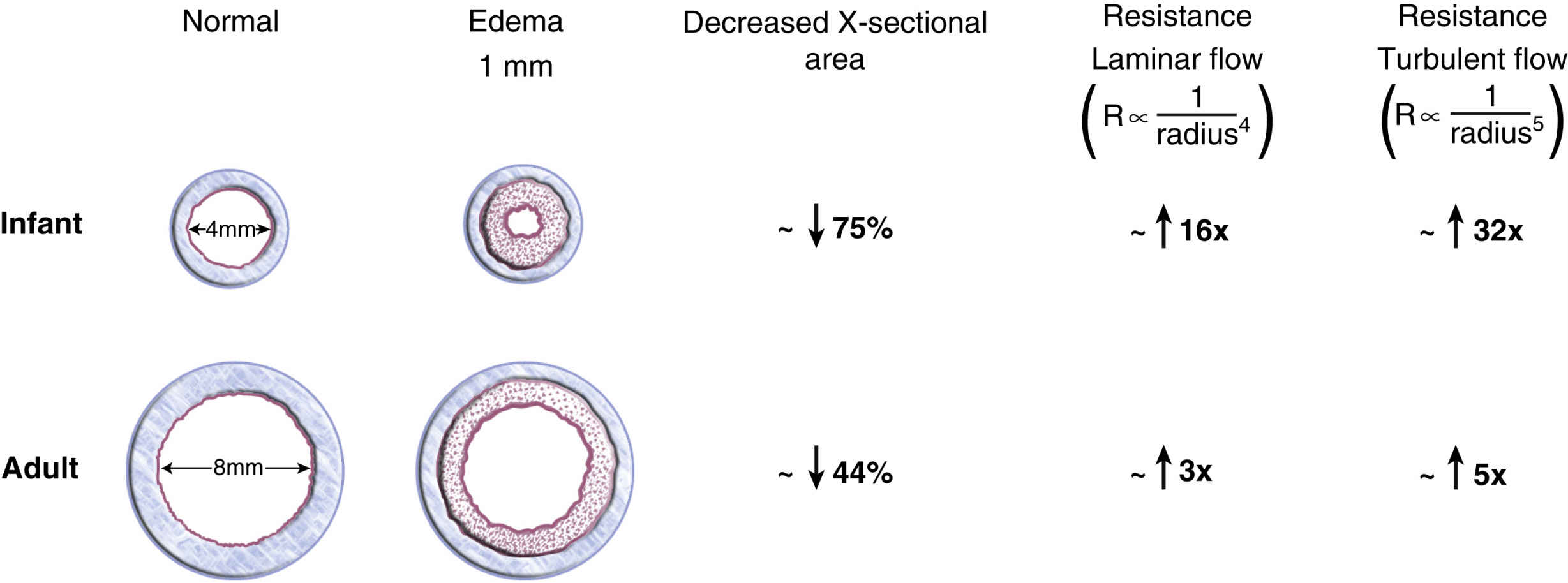
FIG. 49.1 Airway resistance. (From Cote CJ, Lerman J, Anderson B: A practice of anesthesia for infants and children, ed 5, St. Louis, MO, 2013, Elsevier.)
Table 49.4
Equivalent Hemoglobin Values for Adults, Infants, and Neonates
From Davis PJ, et al.: Smith’s anesthesia for infants and children, ed 8, Philadelphia, PA, 2011, Elsevier.
At birth, fetal hemoglobin levels are high compared with those in the adult patient; however, the fetal hemoglobin does not readily release the oxygen it carries to tissues. Hemoglobin values decrease progressively and reach their lowest values by 2 to 3 months of age.9 By 4 to 6 months of age, the amount of oxygen available to tissues begins to increase and reaches the highest value usually by 10 months of age. This increase remains steady during the first decade of life. Research regarding the physiologic anemia of childhood suggests that, although children’s hemoglobin levels are lower than adults’, oxygen unloading at the tissue level is increased in children.9 This allows a lower level of hemoglobin in infants and children to be as efficient in tissue oxygenation as a higher hemoglobin in adult patients (Table 49.4).
Composition and Regulation of Body Fluids
Maturation of the kidneys in newborns occurs rapidly. In the neonate, renal function is characterized with obligate salt loss, slow clearance of fluid overload, and an inability to conserve fluid.19 Consequently, newborns are intolerant of both dehydration and fluid overload. The newborn can conserve sodium to some degree despite a low glomerular filtration rate and limited tubular function.9 However, premature infants are prone to hyponatremia and water overloading. Dehydration in the neonate of any gestational age has harmful effects on renal function.19 Moreover, decreased renal function can delay the excretion of drugs primarily eliminated by renal clearance. At 20 weeks after birth, maturation of glomerular filtration and tubular function is nearly complete.9,13
The blood volume of the newborn younger than 1 month of age is approximately 80 to 90 mL/kg15; however, the blood volume of the premature newborn is as high as 100 mL/kg. The estimated blood volume of an infant from 3 months until 3 years of age is 75 to 80 mL/kg. In children older than 6 years, the estimated blood volume approximates that of an adult (65 mL/kg in the adult female; 70 mL/kg in the adult male).15
Water distribution in the various body compartments is markedly different among the premature newborn, the full-term newborn, the child, and the adult. Water distribution is significant because body water composition affects the volume of distribution of drugs. Fluid requirements are greater on a mass basis for infants and children because of their caloric requirements and intravascular volume relative to their body mass. This high metabolic demand stands in sharp contrast to a functionally and anatomically immature kidney.10 Complete maturation of renal function occurs when the child reaches 2 to 3 years of age.
Table 49.5
Assessment and Evaluation of Dehydration in Children
From Davis PJ, et al.: Smith’s anesthesia for infants and children, ed 9, Philadelphia, PA, 2017, Elsevier.
It is important to assess the hydration status of the pediatric patient to formulate an appropriate therapeutic strategy. Guidelines for assessing dehydration in children are provided in Table 49.5. Laboratory data, history and physical, and assessment of fluid input and output should be used to aid in the diagnosis of dehydration and guide therapy.
Evaluation of fluid deficits and replacement is an important part of anesthesia care and hand-off in the postanesthesia care unit (PACU). The most common method of maintenance fluid calculation for the pediatric patient is based on the weight in kilograms (kg) of the child.15 For the first 10 kg of weight, the calculation is 4 mL of fluid/kg/h. An example for an 8-kg infant would then be determined as 4 × 8 = 32 mL/h. Children weighing from 10 kg to 20 kg should receive an additional 2 mL/kg for every kg over 10 kg. So, for example, a 15-kg child would receive (10 × 4) + (5 × 2) to equal 50 mL of fluid/h. Children weighing more than 20 kg would receive an additional 1 mL of fluid for each kg over 20 kg. For example, a child weighing 32 kg would receive (10 × 4) + (10 × 2) + (12 × 1) to equal 72 mL/h of fluid. This is considered the 4:2:1 method of calculating maintenance fluid for the pediatric population. Fluid deficits related to an NPO status for surgical procedures lasting over 1 hour are generally replaced as one half of the deficit over the first intraoperative hour followed by the remainder of the deficit divided over the next 2 hours of surgery. This deficit fluid replacement is in addition to the necessary maintenance fluid.15 The fluid requirements for infants and children are reviewed in Table 49.4. Routine use of glucose administration is no longer advised for healthy children, and lactated Ringer solution is tolerated well. Intravenous therapy can be adjusted with use of glucose solutions when necessary. Premature infants are more disposed to hypoglycemia and may receive an infusion of dextrose 10% in 0.2% normal saline.15 The fluid requirements for infants and children are reviewed in Table 49.6.
Table 49.6
Formula for Hourly Maintenance Fluid Requirements in Infants and Children
| Body Weight (Kg) | Hourly Fluid Requirement∗ |
| 0–10 | 4 mL/kg/h for each 1 kg body weight |
| 10–20 | 40 mL + 2 mL/kg/h for each 1 kg >10 kg |
| >20 | 60 mL + 1 mL/kg/h for each 1 kg >20 kg |
Thermal Regulation
Newborns and infants are sensitive to heat loss because they have a relatively large body surface area, a relatively small amount of subcutaneous fat, poor vasomotor control, and a decreased ability to produce heat.20 The primary mechanism of heat production in a neonate is nonshivering thermogenesis mediated by brown fat.7,9,21 Shivering is of little significance to thermal regulation. When ambient temperature falls (<33°C), epinephrine is released by the sympathetic nervous system to activate thermogenesis. The preterm newborn needs a higher ambient temperature (at least 35°C) to minimize oxygen consumption.20 Ordinarily, to maintain a body temperature within normal limits, infants metabolize brown fat, cry, and move about vigorously. Newborns and infants respond to a cold environment by increasing their metabolism, which ultimately leads to an increase in oxygen consumption and the production of organic acids.
Prematurity
A premature newborn is defined as birth before 37 weeks’ gestation.9,10,15,19 The often-labile condition of a premature neonate demands meticulous and vigilant perianesthesia care. Most premature newborns are cared for in neonatal intensive care units (NICUs).
Careful attention must be given to airway maintenance, medication dosage, fluid management, and temperature regulation. Premature infants and infants younger than 6 months are prone to airway obstruction and apneic episodes.9,15 Most infants in whom postanesthesia apnea develops are less than 46 weeks of postconceptual age; however, apnea has been reported in infants up to 60 weeks of postconceptual age.8 In the sick premature neonate, the likelihood of blood transfusions, artificial ventilation, and the need for parenteral nutrition is greater.8
The risk of apnea in the PACU may be decreased with intravenous (IV) administration of caffeine (10 mg/kg).9 However, it would be important to note if the infant was already undergoing treatment with a regimen of intravenous (IV) caffeine for previously diagnosed central apnea. In neonates, the half-life of caffeine is 37 to 231 hours.9 By 4 months of age, the half-life of caffeine decreases dramatically to approximately 6 hours and is similar to that in an adult. In addition, several authors cite the initial discovery of xanthine derivatives such as theophylline or aminophylline as a respiratory stimulant that can be used to decrease the frequency of apneic episodes in the newborn. 8,9,19
Pediatric Perianesthesia Considerations and Techniques
Preoperative Period
The preoperative meeting with the pediatric patient and his or her guardians begins the foundation of the perioperative care for this child. The concept of family-centered care (i.e., the family is involved in the decision making along with the medical team) is imperative to a successful process as the family truly knows and understands the specific needs of their child. This is a team effort with the family at the center with knowledge of the intricacies of their child including how to best assist the child to cope with the hospital, surgical, or procedural experience. Typically, children who present for surgery are in excellent health. However, many have complex medical and sometimes psychological issues that require assessment, evaluation, and careful planning by the team. Comorbidities in pediatric patients are generally genetic, congenital, or developmental.22 A thorough preoperative examination of the pediatric patient and the child’s medical record enable the nurse to assess the patient’s general state of health and identify chronic or acute disease processes. The preoperative evaluation should include (1) reviewing the patient’s chart; (2) reviewing current and past medical history of the patient with the patient and guardian(s), especially any recent upper respiratory tract infections; (3) determining medication, latex, and food allergies; (4) determining the fasting (NPO) status of the patient; (5) formulating a list of the patient’s current medications including herbal medications; (6) determining any significant risk factors for postoperative nausea and vomiting (PONV); and (7) evaluating the patient for the potential of obstructive sleep apnea (OSA) or sleep-disordered breathing (SDB). Some institutions are using the STBUR scoring system to determine OSA or SDB in the pediatric population, and then titrating postoperative opioids as indicated. Routine laboratory work is not generally part of the preoperative screening process for the pediatric population. Laboratory work is done if there is a targeted question to answer or there are previous health issues being treated.
As a special note, it is very important to have a time to separate the older child or adolescent from the parents to inquire about sexual activity or orientation, if they feel safe at home, and if they are currently using recreational drugs. It is no longer unusual for some teenagers to use marijuana to help decrease their anxiety before coming to the hospital, which can significantly affect their anesthesia and immediate postoperative course.
Before initiating any preoperative interventions, the NPO status of the patient must be confirmed. NPO guidelines have been formulated to help prevent the aspiration of stomach contents into the lungs during surgery. The American Society of Anesthesiologists (ASA) recommends fasting from clear fluids for 2 hours before anesthesia for children. Clear liquids consist of water, nonparticulate juices (e.g., apple, white grape), Pedialyte, and popsicles. Fasting from breast milk for 4 hours and formula for 6 hours is recommended. The suggested fasting period for solid food is 8 hours in all children.10
Preoperative education is key to helping children cope with the stress of having a surgical procedure. Parents and children want detailed information before the procedure.22 Many facilities provide a preoperative handout explaining what to expect that day as well as providing tours of the area with the child before the day of surgery. Younger children may benefit from time used to play with some of the hospital equipment such as masks, OR caps, and even syringes without the needle attached. Many pediatric facilities have child life specialists who work with highly anxious children the day of surgery. Children may need to act out some of this through play to assist with coping with stress. Many children benefit from storybooks specifically about going to the hospital. This process can increase their understanding about what might happen so their imagination doesn’t create an unrealistic anticipated experience.
Older children and teenagers have questions about the type of pain to expect after the operation, what their scar might look like, as well as what will be done to maintain their privacy and exposure throughout the time they are asleep. Adolescents need time to speak with the anesthesia provider and have concerns to address such as death and disfigurement or waking during the procedure. They need to be reassured as they may not initiate this type of conversation for fear of appearing weak or foolish.2
Pain issues need to be discussed in the preoperative area. It is important to assure families and patients that the entire team has the goal of treating pain and providing comfort. Discussing the treatment options or medications that have been useful in the past as well as medications that might not have worked maybe helpful. Parents can relay the words their child might use to tell them they are in pain (e.g., boo-boo, owie, ouchie).
This is a good time to educate patients about pain scales and what will be asked of them after the procedure. Younger children can look at a “FACES” scale and talk about what each face looks like to them. The anesthesia team may discuss various regional blocks or patient-controlled analgesia (PCA). Families and patients may need additional education and instruction about anesthesia or how to use the PCA. Parents need to know that some younger children become very anxious and/or agitated if a block is used and they cannot feel their affected extremity.
Overall, it is most important to assure the patient and the patient’s parent or guardian that pain will be treated promptly, but also that treatment may not eliminate all pain. Parents should be educated to become partners in providing comfort and reassurance to their children and to assist in evaluation of pain as well as provision of coping and distracting techniques. Having a parent ask, “Are you in pain?” every 5 to 10 minutes does not help with establishing a comfort goal. They may also need some redirection and refocus so they can understand how they can best help.2
There are some instances where an intravenous catheter may be placed before going to the OR. There may be a need for antibiotic administration before the surgery. Some older school-age children and teenagers may request to have a total intravenous medication induction and are willing to have an IV placed preoperatively. The most common practice for the pediatric population is to refrain from placing the intravenous catheter until the child is in the OR and has fallen asleep with an inhalation anesthetic gas.10
Many pediatric institutions offer choices for helping an anxious child back into the OR and through induction. These are institution- and anesthesia provider–specific practices. After evaluation and team discussion, some parents may be allowed to accompany their child to the OR for inhalation induction of the child. This process helps with the child’s potential separation anxiety, but only if the parents are relaxed and can be helpful with distraction. Children take cues from their parents and any outward worry or concern will affect the child’s state of anxiety.
Parents need to be educated about what it might look like as their child “falls asleep.” Induction of anesthesia will appear different from normal sleep as their child goes through stage II. Parental presence during induction may not be right for every parent. Parents must be reassured that it is acceptable for them not to participate in induction.
Some practitioners may choose to give an anxiolytic medication such as midazolam after evaluating the cooperation of the child and discussion with the parents. Midazolam can be administered without an IV present via oral, rectal, or intranasal routes. The intranasal route has a faster uptake and effect; coordinated timing with oral or rectal administration may be needed. Midazolam is generally given about 10 to 20 minutes before going to the OR. Once the child has received midazolam, it is important to confine him or her to the bed, stretcher, or parent’s lap to prevent any possibility of fall injuries. Some institutions may opt to place these children on a pulse oximeter after administration.
The most popular inhalation anesthetic agents used for pediatric anesthesia are sevoflurane, halothane, isoflurane, and desflurane. Sevoflurane is the most common induction inhalation agent in the pediatric population because it is least irritating to the airway and has a rapid onset of effect and offset at the end of the case.10 Halothane is no longer available for use in the United States but may be used in some other countries throughout the world. Sevoflurane may be superior to halothane for mask induction of general anesthesia because of (1) a quicker induction of anesthesia, (2) less incidence of cardiac arrhythmias, (3) more rapid psychomotor recovery postoperatively, and (4) less nausea and vomiting.23 An anticholinergic drug such as glycopyrrolate or atropine may be given by the anesthesia team before induction to protect against bradycardia, which can occur with the induction of general anesthesia.9,19,24 The induction of general anesthesia is usually initiated with sevoflurane and, when the child reaches the maintenance phase of general anesthesia, the anesthesia provider may switch to either isoflurane or desflurane. To help prevent emergence delirium, an analgesic and possibly propofol may be administered before emergence from general anesthesia and transfer to the PACU. See the Evidence-Based Practice box for information regarding anesthetic agents in the pediatric population.