To easily identify the specific classifications of topical ocular medications, the American Academy of Ophthalmology (AAO), with input from pharmaceutical companies and the Food and Drug Administration (FDA), developed a universal color-coding system to distinguish among all topical ophthalmic medications. The color-coded system identifies every pharmaceutical class with its own unique cap and label color scheme (Table 33.2). With the introduction and implementation of the voluntary color-coding system, the AAO expects to “decrease the amount of serious adverse events resulting from patients (and medical personnel) difficulty in distinguishing between various ocular medications.”4 The threefold partnership of voluntary cooperation among the FDA, the pharmaceutical industry, and the AAO has proven to be very effective in and advantageous to the primary interest of patient safety since its inception.
Table 33.2
Ophthalmic Medication Color-Coding System
| Class | Color |
| Adrenergic agonists | Purple |
| Adrenergic agonist combinations | Light green |
| Antiinfectives/antimicrobials/antivirals/antifungals | Tan |
| Antiinflammatory/nonsteroidal | Gray |
| Antiinflammatory/steroidal | Pink |
Antiinflammatory/ immunomodulators | Olive green |
| Beta-blockers | Yellow |
| Beta-blocker combinations | Dark blue |
| Carbonic anhydrase inhibitors | Orange |
| Cytotoxic | Black |
| Miotics | Dark green |
| Mydriatics and cycloplegics | Red |
| Prostaglandin analogs | Turquoise |
Adapted from American Academy of Ophthalmology: Color codes for topical ocular medications (website). www.aao.org/about/policies/color-codes-topical-ocular-medications. Accessed May 27, 2016.
Preoperative Phase
Patients undergoing eye surgery will understandably have more apprehension and will need more constant verbal communication and reassurance. The perianesthesia nurse should use this time to review any preoperative education and postoperative instructions with the patient and any caregivers present. Expectations about the operative procedure’s outcome should also be explored. It is important that the patient and caregiver have realistic expectations before going into surgery. As suggested by Hata et al., the more information and education that can be given to a patient and caregiver about the anticipated perioperative and postoperative course, the less amount of anxiety the patient will have and the less antianxiety medications that will be required.5 All preoperative laboratory work, medical tests, and clearance letters should be reviewed to ensure that all paperwork is in order and placed on the chart. The nurse should also verify each patient’s name, the operative eye, and procedure to be performed. Planned preoperative medications should be discussed. Depending on the type of ophthalmic procedure to be performed, ophthalmic medications may be administered in the preoperative holding area. A significant reduction of systemic absorption can be achieved by occluding the nasolacrimal duct by pressing on the inner canthus of the eye or closure of the eyelids for a few minutes immediately after the administration of ophthalmic medications. This will reduce the chances of undesirable systemic side effects.1
Anesthetic Options
The determination of the type of anesthetic to be used is between the surgeon, the anesthesia provider, and, most important, the patient. Factors that influence this decision are the type and length of the procedure to be performed, the physical status of the patient, and the ability of the patient to remain still. Local anesthesia can appear less stressful and more beneficial to some patients, but the thought of being awake while having eye surgery is terrifying to others. For those patients, general anesthesia is safer and more acceptable. Children and other uncooperative adults also benefit from general anesthesia. Lack of patient cooperation and head or body movements could result in very poor outcomes.
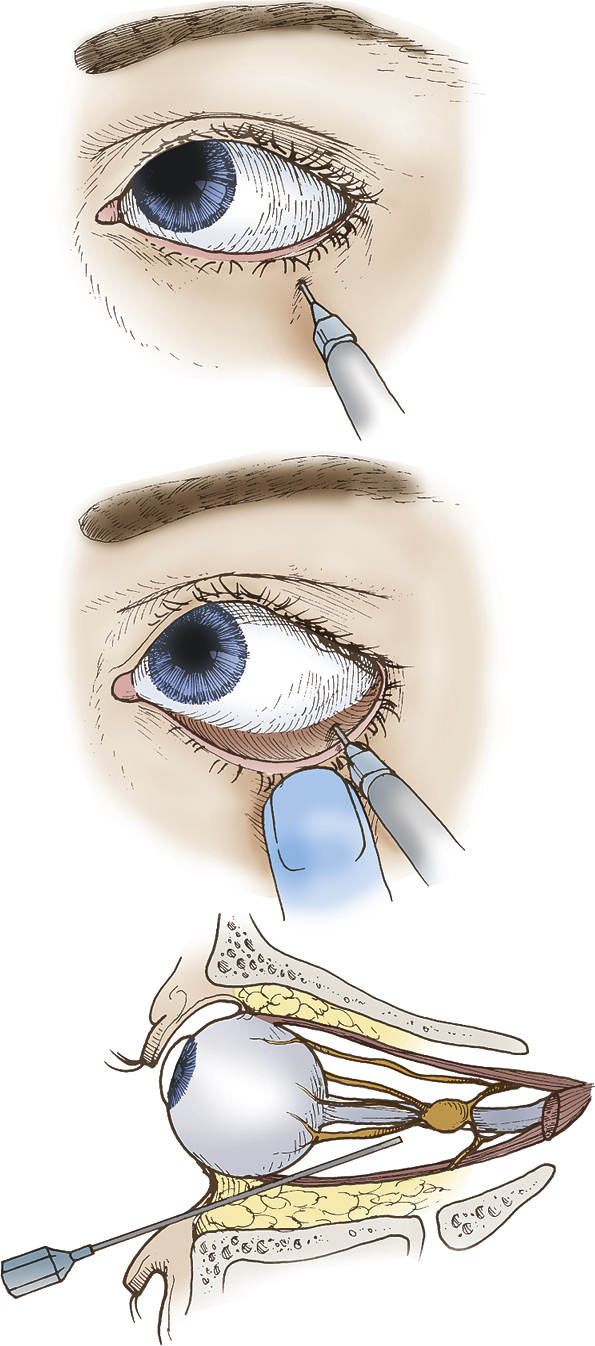
Local anesthesia can range from the topical instillation of 0.5% tetracaine anesthetic drops to an injection of a local anesthetic. A patient with a relatively quick surgeon performing a simple anterior chamber cataract removal, intraocular lens implantation, or glaucoma procedure could have a topical anesthetic provided the patient is cooperative. Intracorneal anesthesia is also used for cataract surgery. The surgeon injects a local anesthetic directly into the anterior chamber of the cornea where anesthesia is needed. The most common nongeneral anesthetic techniques are the modern approaches to the peribulbar and retrobulbar blocks (Fig. 33.1). These blocks are performed by the surgeon or the anesthesia provider after sufficient sedation has been given. A 25- to 31-gauge retrobulbar (blunt-tipped) needle is used to inject 3 to 5 mL of local anesthetic either into the peribulbar or retrobulbar space. Lidocaine 2% and bupivacaine 0.75% are the most common local anesthetics used. Epinephrine (1:300,000 or 1:400,000) may be premixed into the local anesthetic to cause vasoconstriction of the blood vessels, thus reducing bleeding and decreasing the absorption rate of the local anesthetic. It is important that the perianesthesia nurse be aware of these techniques and potential side effects because assistance may be needed with the application of a local anesthetic. An eye that has had a successful retrobulbar block will not move during head turning. Complications are rare but can include orbital complications such as conjunctival or retrobulbar hemorrhage; globe perforation or penetration; optic nerve injury; and systemic complications such as oculocardiac reflex (OCR), instantaneous convulsions, and/or respiratory arrest. Other local blocks used alone or in conjunction with the peribulbar or retrobulbar blocks are the sub-Tenon block and the facial nerve block. It is imperative that the patient be closely monitored for any signs or symptoms of any complications while they are in the preoperative area after receiving any type of local anesthetic.6
Perioperative Phase
Numerous ophthalmic procedures are routinely performed, with most procedures performed on an outpatient basis (Box 33.1). A few exceptions include true ophthalmic emergencies in which therapy should be started within minutes. These true emergencies include chemical burns of the cornea, central retinal artery occlusion, traumatic eyeball contusion injury, and/or traumatic enucleation. Other urgent eye conditions in which treatment should be initiated within one to several hours include open-globe injuries, endophthalmitis, acute narrow-angle glaucoma, acute retinal detachment (Fig. 33.2), corneal foreign body, and lid lacerations. These emergencies require surgical treatment within one to several hours. However, these procedures do not always necessitate an overnight admission to the hospital. If the patient is stable and able to meet discharge criteria, most physicians will discharge the patient and schedule an appointment the next morning in the office. Semiurgent situations would include ocular tumors, blow-out fractures of the orbit, acute-onset cataract (Fig. 33.3), and chronic retinal detachment. Treatment for these types of situations is usually started within days of the initial injury but can be rescheduled for several weeks post incident. Another reason for an overnight hospital admission would be for a prolonged procedure on a pediatric patient or a patient with an extensive medical history.2