FIG. 42.1 Sites of implantation of ectopic pregnancies. Order of frequency of occurrence is ampulla, isthmus, interstitium, fimbria, tubo-ovarian ligament, ovary, abdominal cavity, and cervix (external os). (From Lowdermilk DL, Perry SE, Cashion K, et al.: Maternity and women’s health care, ed 11, St. Louis, MO, 2016, Elsevier.)
If laparoscopy is performed, the ovary is not resected or removed unless the ovary is involved with the ectopic pregnancy. If implantation occurs in the cervix or cesarean scar, a hysterectomy may be indicated to control hemorrhage.24 A call for conservative treatment without a hysterectomy is growing backed by multiple case studies and commentaries in the literature.24 If abdominal implantation has occurred, the fetus is removed and the placenta often is left within the cavity to be reabsorbed. Methotrexate may also be recommended.25,26
Laparoscopy (or laparotomy) is performed with general anesthesia. Postanesthesia care is standard care as for any postlaparoscopy procedure including assessment of vaginal drainage.17 The perianesthesia nurse should be especially observant for signs of intraabdominal hemorrhage and shock because these are not uncommon complications of ectopic pregnancy, especially one that has ruptured before surgery. All patients with an ectopic pregnancy should be typed and screened unless the patient is already hemodynamically unstable. In case of hemorrhage, packed red blood cells are generally used for transfusions (good for 3 days).24 Women who are Rh negative must receive alloimmunization to prevent sensitization.27 As mentioned previously, many ectopic pregnancies are successfully treated without surgery and only with medications.25,26 Nurses caring for these patients should remember that the patient may perceive this as a pregnancy loss and need appropriate supportive comfort care. The greatest factor in perinatal grief is not the length of gestation but the woman’s perception of the pregnancy.28
Cervical Cerclage
The McDonald or Shirodkar procedure is used to treat cervical insufficiency (the cervix dilates and thins out too early) and is fairly successful in reducing preterm birth in singleton pregnancies. The suture is usually placed between the fourteenth and eighteenth weeks of gestation. These procedures may be accomplished with general, spinal, or regional anesthesia.4,29–31
On admission to the PACU, hospital guidelines are followed on patient admission to the PACU and care of the patient (see Chapters 27 and 28).17,32 Pain should be minimal and easily controlled with a simple analgesic such as acetaminophen. Any gross vaginal bleeding or abdominal cramping should be reported to the surgeon because this procedure may indicate labor and expulsion of the uterine contents. The obstetrician may also order indomethacin, a prostaglandin synthetase inhibitor, to reduce uterine contractions, with a dosage of 25 or 50 mg administered orally.33 If labor begins, the suture must be removed immediately, as there is risk that the cerclage suture will tear, resulting in significant cervical bleeding.
Dilation and Curettage
Dilation of the cervix and curettage of the uterus (D&C) is used for the termination of early pregnancy (i.e., first trimester) or in treatment of incomplete spontaneous abortion as well as diagnostic purposes. A general anesthetic can be used, but the trend has been toward the use of paracervical block and IV moderate sedation. Nursing care in the PACU is essentially the same as after D&C by conventional means, with attention to the amount of cramping, discomfort, and vaginal bleeding, which should be minimal. Complications from this procedure include incomplete evacuation and hemorrhage, which may be treated with misoprostol, methylergonovine, or oxytocin.34 Uterine perforation can occur and must be treated surgically. The woman who is Rh negative should receive treatment to prevent sensitization.27
Gynecologic Surgery
Gynecologic surgery has changed a great deal in recent years for several reasons. The first reason is that more young females are requiring gynecologic surgery for treatment of pelvic pain and less frequently for congenital anomalies. More young females are being seen for incapacitating pelvic pain that may be caused by endometriosis in particular to the extent that surgical intervention is required. Parents, school nurses, teachers, coaches, pediatricians, and other health care providers need to be aware of this. Generally, pelvic pain is associated with the menstrual cycle.1
In general, women may have incapacitating pelvic pain requiring surgery.35–38 This is usually due to severe menstrual cramps and/or bleeding oftentimes associated with endometriosis, fibroids, ovarian cysts, adhesions, and/or infection. Another common reason for gynecologic surgery is pelvic floor prolapse. Patients with prolonged or heavy menstrual periods may be more chronically anemic. Large amounts of blood may have accumulated within the pelvic organs at the time of surgery. Although the procedure may be elective, many gynecologic operations are associated with significant blood loss, depending on the approach taken. This can be affected by a larger uterus with multiple fibroids. A well-trained laparoscopic surgeon and team will hopefully increase efficiency intraoperatively, reduce blood loss, limit complications, and decrease postoperative morbidity.
In the case of a premenopausal woman undergoing a hysterectomy where the uterus is large and/or a myomectomy, the uterine vessels may be significantly larger than usual. Regardless of the approach (laparoscopy with or without the robot, vaginal, or laparotomy), all vessels and pedicles must be identified and coagulated or ligated effectively. In addition, because of the proximity of the female organs to the urinary tract, great care must be taken during surgery to identify the ureters and bladder. Also, the bowel must be safely out of the way to prevent injury. Proper postoperative observation and follow-up of all systems must be done. If there is any question regarding the urinary tract during surgery, a cystoscopy should be done near the conclusion of the surgery.39,40
More and more gynecologic surgery is being done with a minimally invasive approach.41 These procedures are often done laparoscopically, and the robot may or may not be used. The perianesthesia nurse needs to know how to care for the patient regardless of the approach taken.17,42,43 In addition to overall assessment and general care of these patients, the perianesthesia nurse should direct specific attention toward the patient’s cardiovascular status, renal function, and fluid balance.17
Laparoscopy
Operative laparoscopy commonly is performed as outpatient surgery (23-hour overnight stay) for treatment of benign gynecologic problems and may involve advanced operative laparoscopic procedures for more significant problems that involve the pelvic organs. A small incision (approximately 1 cm) is made at the subumbilical site for insertion of the primary trocar (typically 5, 10, or 12 mm in diameter), which houses the laparoscope with attached video camera for visualization of the pelvis (Fig. 42.2). The entry into the pelvic cavity can be done various ways; one of which includes open laparoscopy, particularly for patients who have had multiple previous surgeries to protect against injuring the bowel.41 When a patient has had multiple previous surgeries, the bowel is more likely to be adhered to the abdominal wall. After pneumoperitoneum is established, the surgeon can visualize the organs within the peritoneum. The video camera enables the surgeon, first assistant, scrub technician, and entire team to view the procedure on the video monitor (Fig. 42.3). A high-definition video camera attached to the laparoscope provides visualization of the pelvis. Continued advances in digital technology increase the resolution and lighting dramatically. Visualization of the abdomen and pelvis continues to improve (Fig. 42.4). The surgeon generally uses a laparoscope that is 5, 10, or 12 mm in diameter. Ancillary instruments are typically 5 to 12 mm in diameter. An angled laparoscope may be used for difficult cases when there is a large uterus to improve visualization. If the robot is used, it is connected after the trocars have been placed. The robot offers three-dimensional visualization that some find appealing. The surgeon sits at a console and is able to maneuver the instrumentation from that location while the surgical assistant is at the patient’s side and using instrumentation such as suction and irrigation. In addition, a surgical technologist is typically present between the patient’s legs (similar to laparoscopy without the robot) to manipulate the uterus with a uterine manipulator. If an emergency arises with bleeding that cannot be controlled, the robot is quickly disengaged so that a laparotomy can quickly be initiated. Newer robots may have two consoles so that the surgeon may have a student surgeon (resident or fellow) at the secondary console to work and receive instruction.44–46
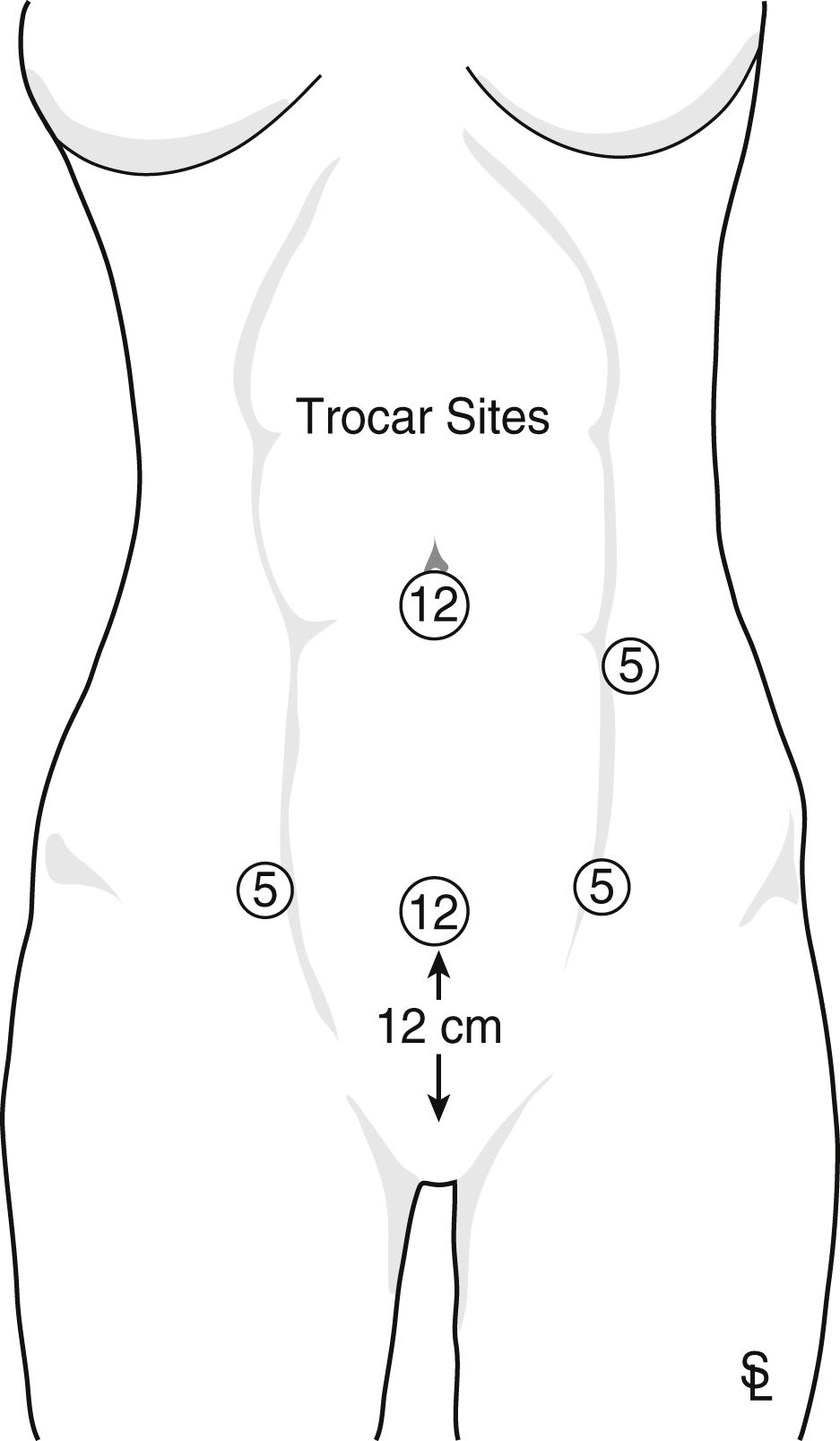
FIG. 42.2 Placement of trocars during advanced operative laparoscopy. Trocar in upper left quadrant is optional and only recommended in cases in which primary trocar is not sufficient because of severe adhesions. Laparoscope needs to be placed off to one side for taking down adhesions.
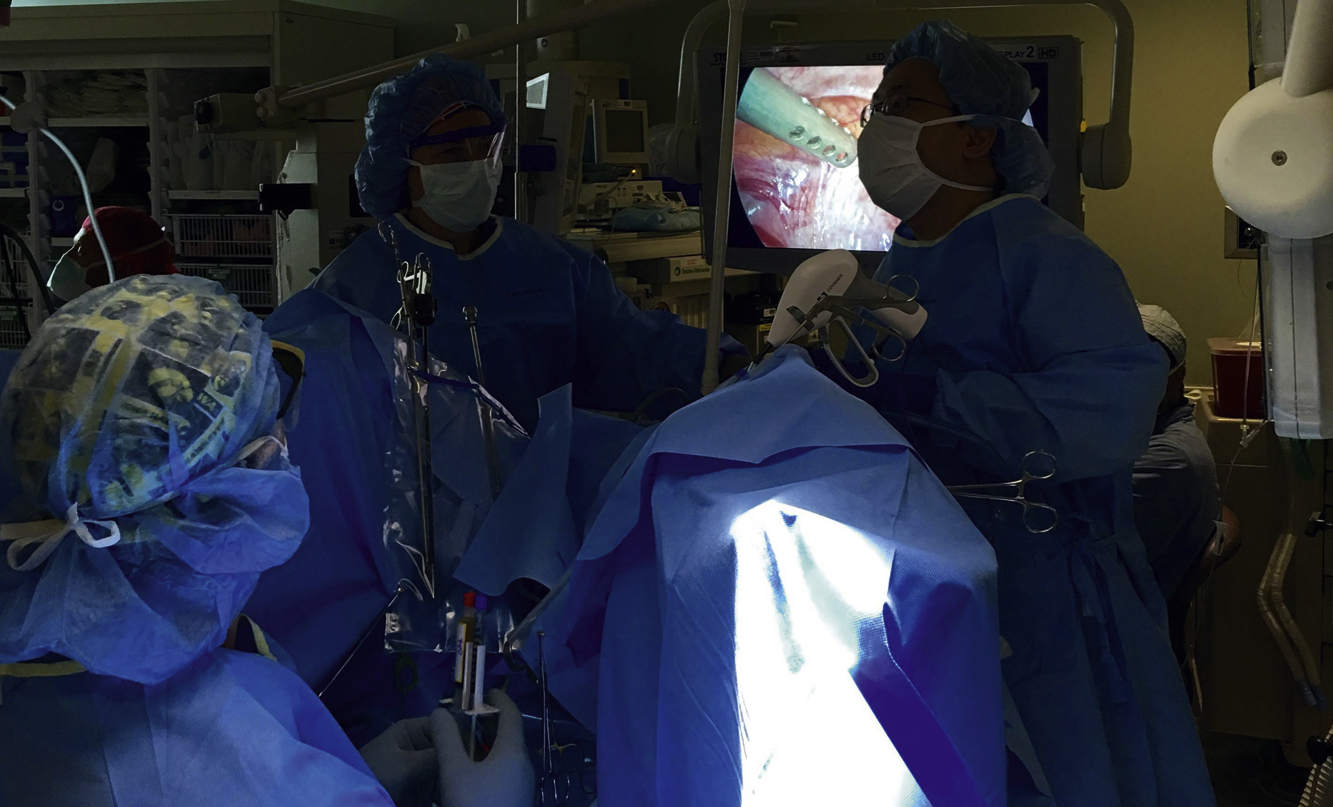
FIG. 42.3 The entire team plays a key role during surgery as seen in this photo (surgeon, surgical assistant, surgical tech, circulating nurses, laser technician, and anesthesia).

FIG. 42.4 Updated technology plays an important role during operative laparoscopy as seen in this photo (HD camera and LED monitors, digital displays, high-flow insufflator, high-intensity light source, and various types of energy sources).
The surgeon examines the ovaries, fallopian tubes, pelvic side walls, uterosacral ligaments, bowel, appendix, peritoneum, anterior and posterior cul-de-sacs, and uterus after placement of the second and third incisions suprapubically in the right and left lower quadrants of the abdomen to house the ancillary instrumentation. If additional instrumentation is needed, a fourth incision may be made along the midsuprapubic area or on one side or the other. During operative laparoscopy, the surgeon will evaluate the abdomen and pelvis. The procedure may be as simple as thorough washings (as in the case of an infection), biopsies, or a tubal sterilization.
More advanced laparoscopic procedures may include aspiration or excision of an ovarian cyst, lysis of adhesions, excision of endometriosis, myomectomy, hysterectomy, salpingectomy, salpingo-oophorectomy, oophorectomy, tubal reanastomosis, removal of an ovarian remnant, ovarian cystectomy, ureterolysis, or pelvic floor support (paravaginal repair and/or Burch procedure, sacral colpopexy, rectocele, cystocele or enterocele repairs, or urethral sling).41,47,48
In endometriosis of the bowel, a general or colorectal surgeon may be called in to do a laparoscopic bowel resection. These surgeries may occur in patients with severe endometriosis who have impedance of their bowel function. These patients have been properly consented before surgery and do a complete bowel preparation preoperatively. The colorectal surgeon who is part of the endometriosis team is on standby for that type of procedure. The same thing is possible with endometriosis of the bladder. In this case, a urologist is called in to resect the endometriosis. Once again, patients are thoroughly informed and consented with regard to these possibilities for thorough excision of their endometriosis.
The PACU should be aware of any special needs postoperatively for patients undergoing thorough excision of their endometriosis. In the case of a bowel resection, the incisions might be different. The postoperative diet is important as well as auscultation of bowel sounds and documentation of any significant amount of blood or mucus that might be present rectally. In a patient who undergoes cystotomy, a urinary catheter will remain in place longer, and blood-tinged urine is likely. Some patients with pelvic pain have interstitial cystitis and are more prone to having blood in their urine. The urinary catheter must be properly secured so that no tugging of the catheter occurs and it is not inadvertently removed. The catheter should be cleaned and/or changed based on postoperative guidelines.43 Depending on the extensiveness of the repair, it is likely that the catheter will be left in place for 7 to 21 days based on the recommendation of the urologist. These patients may be placed on additional antibiotics and other medications. If a bowel resection is done, patients are hospitalized for at least 3 to 4 days. The PACU nurse will need to pay close attention to any changes in postoperative orders that might be different from routine. Examples of this will include listening to bowel sounds, a more limited diet postoperatively, and additional medications and anticoagulant medications for patients who are in the hospital for more than 24 hours. The diet is very limited initially: ice chips, followed by clear liquids, clear fluids, and then a soft diet in accordance with the surgeon’s postoperative orders.17
With minimally invasive repairs as a whole, these patients generally do not require a colostomy or a suprapubic urinary catheter. The circulating nurse should communicate thoroughly pertinent information in the report to the perianesthesia nurse caring for the patient in the PACU. The surgeon should be notified if there is a significant amount of bleeding from any orifice.17,42,43

FIG. 42.5 The 5-mm ancillary sites are sutured subcutaneously followed by using a liquid adhesive and Steri-Strips to approximate the edges of the skin incision.
Closure of the skin wound involves a few absorbable-type sutures. It is important to close the fascia at the subumbilical site as well as any other incision sites that are 7 mm or larger to prevent the development of a hernia. The 5-mm ancillary sites are sutured subcutaneously followed by using a liquid adhesive and Steri-Strips to approximate the edges of the skin incision (Fig. 42.5). Patients may have more discomfort postoperatively from larger incisions where the fascia has been closed. In addition, if there is any question about the amount of oozing, a pressure dressing can be placed, and the perianesthesia nurse can reinforce it with a 1-pound sandbag in the PACU. Dressings may include an eye pad or a 2-inch pad at the subumbilical site with clear adhesive type bandages over the other sites to allow the patients to shower (Fig. 42.6). If patients have an allergy to adhesive, then paper tape or Steri-Strips can be used depending on the patient history of sensitivities.
Initial pain in the PACU is generally successfully controlled with antiinflammatory agents or mild opioids. Some patients are very anxious and require additional reassurance in the PACU that can also help to decrease their pain. Patients’ complaints should always be taken seriously. Severe pain may indicate a more severe condition, and the surgeon should be notified immediately. Patients often experience shortness of breath and/or chest pain the first couple of days postoperatively as a result of the gas used during laparoscopy to create pneumoperitoneum, which makes it more difficult for a patient to take a deep breath. Patients’ vital signs must be monitored regularly, and the perianesthesia nurse can never assume these issues are because of gas pain.17 A firm abdomen could indicate abdominal bleeding that is not normal. Severe pain, nausea, vomiting, or an elevated temperature could indicate a bowel perforation. Generally these types of occurrences show up in the first 24 hours, but it is important to note they may not occur for 7 to 14 days postoperatively. Vaginal bleeding may occur post hysterectomy a week or more after surgery. All postoperative instructions must be reinforced in writing and reviewed with the patient and the person caring for the patient when she goes home before discharge. If any of these conditions occur or anything is out of the ordinary, the surgeon should be notified immediately. Again, instructions should always be written and given to the patient preoperatively and reviewed before discharge.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







