FIG. 43.1 A, In stereotactic procedures, patients lie face down on a special table. The woman’s breast protrudes through a hole in the table’s surface, where it is lightly compressed and immobilized while a computer produces detailed images of the abnormality. B, When the biopsy area has been located and mapped, the Mammotome probe is inserted through a ¼-inch incision in the breast, where it gently vacuums, cuts, and removes breast tissue samples. C, The incision is then closed with a small adhesive bandage. (From Rothrock J: Alexander’s care of the patient in surgery, ed 14, St. Louis, MO, 2011, Elsevier.)
The surgical site should be inspected for excessive drainage, which occurs only rarely. The patient can resume fluid and food intake as soon as the cough and gag reflexes have fully returned and nausea has subsided. Pain should be minimal, if any, and easily controlled with minor analgesics, compression dressings, and ice.
Surgical Choices for the Treatment of Cancer
The goals for surgical interventions for breast cancer include diminished potential for local recurrence, reduction of therapeutic surgeries, and minimization of morbidity and mortality.4 Most women need some type of surgery to treat the breast tumor and remove as much of the cancer as possible. Surgical treatment choice depends on the stage of the disease, the size and site of the mass, and the patient’s individual choice. Advances in early diagnosis and modifications in surgical techniques have increased the numbers of surgical choices in the treatment of breast cancer (Fig. 43.2). Surgical treatment may range from breast-conserving techniques (lumpectomy) to modified radical mastectomy that involves the breast and the axillary nodes.
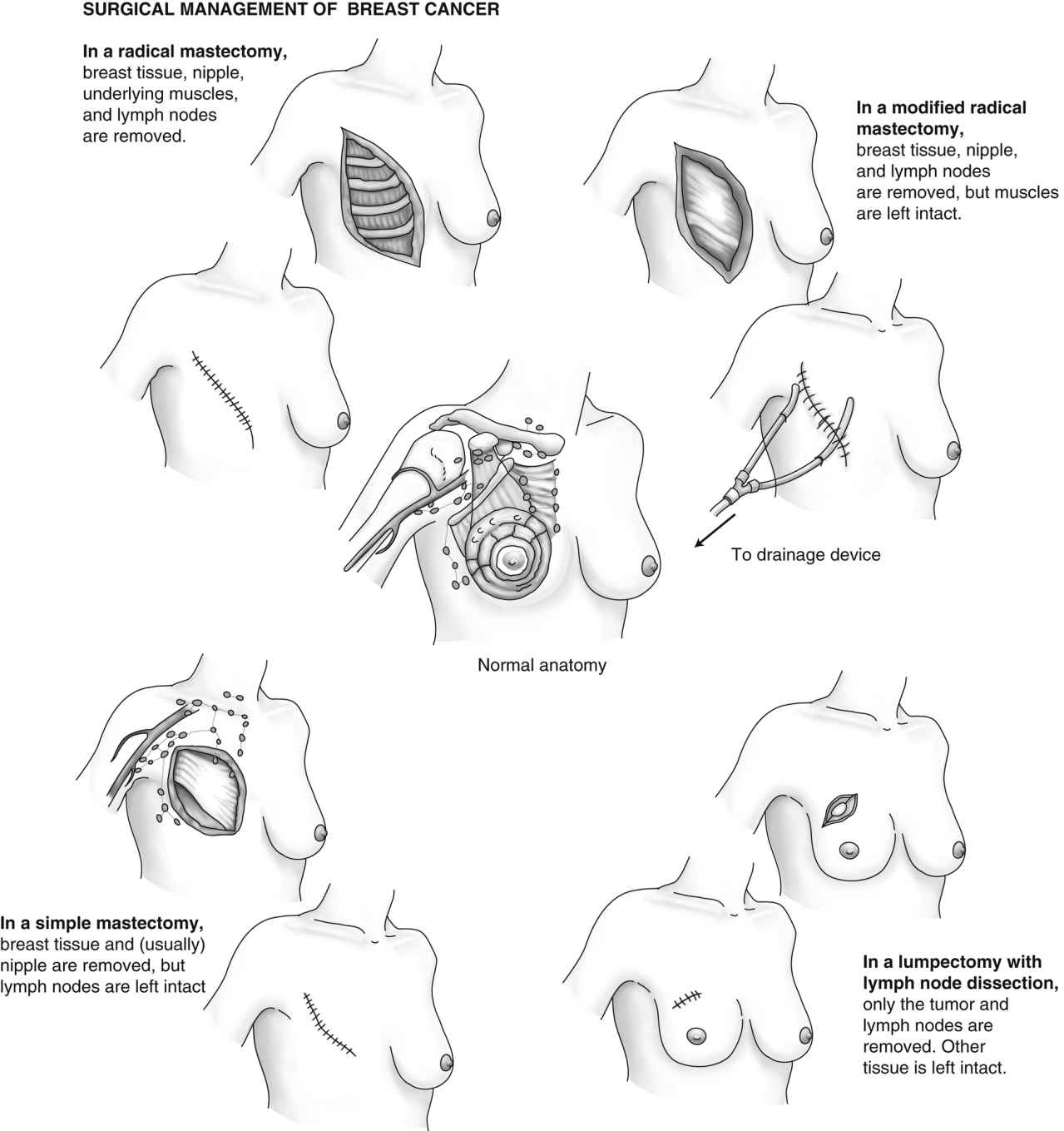
FIG. 43.2 Surgical choices for treatment of breast cancer. (Redrawn from Ignatavicius DD, Workman ML: Medical-surgical nursing: critical thinking for collaborative care, ed 7, Philadelphia, PA, 2013, Elsevier.)
Lumpectomy
Lumpectomy, also called breast-conserving therapy (BCT), is the surgical treatment of choice when the breast tumor is well defined and less than 5 cm in diameter. Lumpectomy is usually performed with general anesthesia. Only the breast tumor and a margin of 1 to 1.5 mm of surrounding normal tissue are removed. Surgery may also be done to determine whether the cancer has spread to the lymph nodes. Lumpectomy with subsequent radiation therapy is frequently the treatment of choice for small tumors. In some patients, a catheter-balloon device commonly referred to as a MammoSite device may be placed at the time of surgery in the lumpectomy site. This device provides a means of delivering brachytherapy (placement of radioactive sources near the site of the tumor) as a means of BCT.
Sentinel Lymph Node Biopsy
A sentinel lymph node biopsy may be done to visually examine the lymph nodes without having to remove them first. Sentinel node biopsy was developed to reduce the morbidity associated with surgical staging of the axilla in patients with no palpable axillary nodes. A radioactive blue dye is injected near the tumor and is carried by the lymph system to the first (sentinel) node to receive lymph from the tumor. This lymph node is most likely to contain cancer cells if the cancer has spread. The sentinel node is not located in the same site in every patient. When this node is found, it is removed and examined. If it is free of cancer, further surgery may not be needed. If there is evidence of positive nodes, then axillary node dissection and adjunct therapy may be required. The axillary node dissection is done through a separate incision and involves a sample of 10 to 15 lymph nodes lateral and inferior to the pectoralis minor muscles for pathology. Removal and examination of the nodes allows for staging of the cancer and helps the patient and provider to choose adjuvant therapy and treatment options. A possible side effect from the removal of the lymph nodes is lymphedema or swelling of the arm (seen in 1 to 3 of 10 women; Box 43.1).
Patient complications from sentinel lymph node biopsy may include allergic reactions to the dye. Use of the dye in patients with known sensitivity is contraindicated, and perianesthesia nurses should be alert for any signs of anaphylaxis.
When the patient is admitted to the PACU, all the initial assessment measures should be performed. The blood pressure cuff should be placed on the arm opposite the operative side. The arm on the operative side should be elevated on a pillow because the removal of lymph nodes increases the risk of lymphedema. The operative-side arm should be assessed frequently for circulatory adequacy with monitoring of color, temperature, capillary refill, and the presence and strength of the radial pulse. Venipunctures and injections should not be performed on the operative-side arm. Sentinel node biopsy is usually an outpatient procedure that allows rapid return to full mobility and permits return to work weeks sooner than after axillary dissection. Dressings should be small, and bleeding or drainage should be minimal. A suction device may be connected to drains placed at the incision site but with a sentinel node biopsy are seldom required.
Nursing personnel should be aware that although this procedure allows the patient to keep the breast, it does not eliminate fear of the cancer diagnosis or concerns about whether the procedure was successful; therefore, the nurse must provide factual reassurance and support.
Mastectomy
Partial (Segmental) Mastectomy
The partial mastectomy involves the removal of more of the breast tissue than in the lumpectomy and is usually followed by radiation therapy. Some surgeons refer now to lumpectomy or partial mastectomy as a wide local excision.
Simple Mastectomy
The simple mastectomy is the removal of the entire breast but not the lymph nodes under the arm. Both breasts may be removed if the patient is at an increased risk for breast cancer. Most patients go home the next day.
Modified Radical Mastectomy
The modified radical mastectomy includes removal of the breast as well as the axillary, pectoral, and superior apical nodes. The underlying pectoral muscles are not removed. The modified radical mastectomy is performed with hopes of decreasing the chance of the malignancy spreading.
Radical Mastectomy
The radical mastectomy is rarely performed in the United States because the modified radical mastectomy has been found to be just as effective for the patient and less disfiguring with fewer side effects. The radical mastectomy involves the extensive removal of the entire breast, lymph nodes, and chest wall muscles under the breast. Refined techniques for diagnosis and surgery, radiation therapy, and chemotherapy have made it unnecessary in most instances.
Mastectomy is performed with general anesthesia. The patient is admitted to the Phase I PACU with the head of the bed elevated 30 to 45 degrees. Admission assessments are performed per PACU protocol. Dressings may be bulky and should be checked frequently for excessive serosanguineous drainage and for constriction. Patients should be observed closely for signs of postoperative hematoma below the skin flaps. Attention to the drains and the maintenance of free drainage within the vacuum system prevent this potential complication. Drains are usually placed under the skin flaps to remove excess blood and serum that ordinarily collect under the wound site, thus causing edema, infection, and sloughing of the skin graft (Fig. 43.3).5 The drains may be connected to a closed suction device. Generally, additional vacuum is needed the first 8 postoperative hours, and the drain is connected to vacuum pressure of 20 to 30 mm Hg. These drains should be monitored for excessive bleeding, which must be reported to the surgeon. Dressings are necessarily snug but should not impair respiration or circulation to the upper extremity. The arm on the operative side should be supported and elevated on a pillow; it must be checked frequently for cyanosis or pallor, and the pulse must be palpated for intensity. If signs of respiratory distress or impaired circulation arise, the surgeon should be notified to rearrange the dressing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







