CARDIAC TAMPONADE
CASE SCENARIO
A 22-year-old man is brought to the emergency department (ED) after an altercation in which he was stabbed in the left chest. On arrival he is diaphoretic, his heart rate is 140 and blood pressure is 80/60. Examination reveals only a puncture wound at the sixth intercostal space, just left of the sternum. Lung sounds are present bilaterally but diminished on the left.
EPIDEMIOLOGY
Cardiac injury is uncommon and has a high mortality rate, making it an infrequent but highly lethal injury encountered by the trauma surgeon. Most victims of penetrating cardiac injury (94%) die before reaching the hospital; 50% of those who survive to the hospital will die as well.1 In certain circumstances, for example, after low-velocity injuries, tamponade may prevent lethal exsanguination and improve survival. Among patients presenting to a hospital in South Africa with cardiac stab wounds, those with tamponade had a mortality rate of only 8% versus 34% among those who did not.2 In contrast, patients presenting with cardiac injuries from gunshot wounds and blunt trauma have high mortality, without any observed survival benefit when presenting with tamponade.3,4
PATHOPHYSIOLOGY
The pericardium functions to isolate the heart from the rest of the mediastinum. It is a fibrous, relatively inelastic structure surrounding the heart and proximal great vessels, and extends from the central tendon of the diaphragm to the great vessels, and from the sternum to the esophagus. The pericardium forms a sac with an outer parietal layer reflecting upon itself to form the epicardial layer of the heart. Within this sac is roughly 30 to 50 mL of serous fluid that serves to lubricate the heart. Bilateral phrenic nerves run along the lateral aspects of the pericardium anterior to the root of the lungs and innervate the diaphragm.
Tamponade physiology arises secondary to the poor distensibility of the pericardium. As the pericardium fills with fluid, it reaches a point of inextensibility.4 The amount of fluid within the pericardium is less important than the speed of its accumulation. The pericardium can gradually stretch to accommodate a chronic effusion of 1 L or more without symptoms; however, tamponade can result from the acute accumulation of as little as 60 to 100 mL of blood.5
Tamponade is a dysfunction of diastolic filling. The inelastic pericardium limits the total intrapericardial volume, and as pericardial fluid volume increases, intracardiac chamber volume must decrease.4 Initially, cardiac output is maintained with compensatory tachycardia, higher filling pressures, and enhanced contractility; however, this will decompensate rapidly with increasing effusions or loss of these mechanisms.6 Tamponade is the endpoint of a continuum of worsening cardiac filling, as higher diastolic pressures are required to overcome the pericardial pressure. Hypotension from low cardiac output follows tachycardia, and ultimately cardiac arrest ensues when intrapericardial and intracardiac pressures equilibrate.7
CLINICAL PRESENTATION
Acute trauma presentations seldom afford clinicians time to investigate the subtleties of pulsus paradoxus and electrical alternans, but tamponade can present in a delayed fashion from missed injuries or even following resuscitation.8 Therefore, surgeons must be able to diagnose tamponade both in the acute setting and when it develops more gradually.
Tamponade is one of the few survivable causes of traumatic prehospital arrest. Between 2003 and 2009, the Western Trauma Association compiled data on all patients surviving ED thoracotomy in 18 participating trauma centers in an effort to characterize the limits of heroic resuscitative efforts.9 Among the 56 surviving patients, 41% presented with tamponade. The results were even more favorable for patients suffering stab wounds, with 57% of survivors presenting with tamponade.
Certain mechanisms of injury are more likely to present with tamponade. Among penetrating injuries, knife wounds are more likely to present in tamponade than gunshot wounds. Tamponade should be suspected with all penetrating injuries to the “cardiac box,” the area between the mid-clavicular lines from the clavicles to the costal margin. Furthermore, the trajectory of bullets cannot be predicted, and seemingly remote gunshot wounds may result in cardiac injury. Blunt trauma is least likely to present with tamponade, although when it occurs the right ventricle usually incurs injury, followed by the left ventricle. The left atrium is the chamber least likely to be injured.7
Despite a number of explicit physiologic changes notable in tamponade, patients present with nonspecific symptoms, including hypotension, agitation, and signs of shock.7 Distended neck veins from increased filling pressures are often present, but are difficult to distinguish in a trauma scenario. Also, jugular venous distension requires time for venous pressure to increase, and so may be absent in acute tamponade, particularly in cases of concurrent hemorrhagic shock.4 Hypotension with compensatory tachycardia as stroke volume decreases is common and worsens with increasing tamponade. The classic presentation of all three components of Beck’s triad—distended neck veins, muffled heart sounds, and hypotension—is rare.
Pulsus paradoxus, the inspiratory fall in systolic pressure of at least 10 mm Hg, may be useful in the diagnosis of tamponade. On inspiration, intrathoracic pressure decreases, resulting in right ventricular filling. However, given the limited intrapericardial volume, the full right ventricle pushes the interventricular septum into the left ventricle. The negative intrathoracic pressure also leads to decreased pulmonary venous return to the left ventricle. These factors combine to restrict left ventricular preload during inspiration.4 However, it is important to note the limitations of using pulsus paradoxus in the diagnosis of tamponade. Pulsus paradoxus will be absent in positive pressure ventilation. Pulsus paradoxus will also be absent in aortic regurgitation, atrial septal defects, left ventricular hypertrophy, and severe hypotension. Conversely, pulsus paradoxus can be seen in the absence of tamponade in the setting of exaggerated inspiratory effort such as chronic obstructive pulmonary disease (COPD), pneumothorax, pulmonary embolus, or stridor.6
Electrocardiogram (ECG) findings of tamponade include tachycardia, low voltage, and electrical alternans.4 Electrical alternans describes the phenomenon whereby every other QRS is of a smaller voltage or reversed polarity. This occurs due to a “swinging” of the heart within the pericardial fluid. While quite specific to tamponade, electrical alternans may also occur with a large effusion in the absence of tamponade.
DIFFERENTIAL DIAGNOSIS
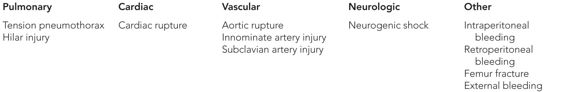
See Table 23–1.
WORKUP AND CHOICE OF IMAGING
The workup of pericardial tamponade depends on the hemodynamic stability of the patient. In the setting of severe hemodynamic instability or cardiac arrest, the patient likely requires immediate diagnostic and therapeutic maneuvers in lieu of imaging. However, tamponade can be diagnosed in the absence of imaging based on history and physical examination findings.
The hemodynamically abnormal patient highlights the importance of rapid imaging in the trauma bay. Ultrasound offers portability, speed, and ease of use, and focused echocardiography has largely supplanted pericardiocentesis and pericardial window as diagnostic tools. For these reasons, the focused assessment with sonography for trauma, or FAST examination, has become critical in evaluating blunt trauma patients in shock. Rozcyki et al. have shown that subxiphoid ultrasound is both highly sensitive and specific for detecting pericardial effusions in patients with penetrating thoracic trauma.10 Importantly, accuracy is maintained regardless of whether an echocardiographer or surgeon performs the scan. There are some limitations to detection, however, as surgeons in this study were unable to obtain adequate windows in 3.5% of patients. Patient factors such as body habitus, presence of pneumothorax, tachycardia, and tachypnea can limit the detection of effusions and tamponade.11 A large hemothorax can obscure the subcostal view as well, but may improve after chest tube insertion.12 Additionally, while ultrasound is generally specific, false positives can occur from incidental effusions. In a study where patients at risk for cardiac injury had pericardial windows performed, a number of false negatives were identified.12
Further transthoracic imaging may be beneficial when the subxiphoid view of the FAST is equivocal or unobtainable. Formal echocardiography provides a more detailed examination for detection of effusions and signs of tamponade physiology.11 There is increasing evidence that limited bedside echocardiography performed by surgeons and surgical intensivists is sufficient in the detection of gross cardiac abnormalities. Transesophageal echocardiography (TEE) is usually not feasible in the immediate evaluation of suspected tamponade, but can provide further detail in some patients. TEE has been shown to be helpful in the preoperative evaluation of an effusion in a stable patient to determine the need for cardiac bypass.13 TEE is also a useful intraoperative adjunct in the event of unexplained hypotension during a non-thoracic trauma procedure such as a laparotomy or pelvic fixation.
Plain x-ray and computed tomography (CT) are complementary to echocardiography. Chest x-ray has limited utility, but may demonstrate injuries associated with effusions and tamponade. CT scan is sensitive for detecting effusions and can show signs of tamponade physiology, and its utility can be further improved with echocardiogram (ECG)-gated CT scan. However, unstable patients with possible tamponade should not undergo CT scan, as time spent in the scanner can create life-threatening delays in treatment.
IMAGING FINDINGS
 Plain Film
Plain Film
Chest x-ray is a staple in the evaluation of the trauma patient. While not ordered for the specific purpose of detecting pericardial effusions, signs of effusion may be evident on chest film. The cardiac silhouette may be widened; however, a normal silhouette does not rule out effusion. In fact, pericardial effusions of 200 to 500 mL are necessary for the cardiac silhouette to appear enlarged on chest film. Other signs suggestive of effusion are a dilated azygous vein and increased pulmonary venous markings.4 Importantly, chest x-ray can show other injuries such as fractures, pneumothorax, and hemothorax, which may assist with the utility of echo or management of the unstable patient (Table 23–2 and Figure 23–1).