Cardiac Output Measurement: Do You Really Understand the Underlying Principles?
Valerie Sera DDS, MD
Matthew Caldwell MD
Fegler introduced the thermodilution method for measuring blood flow in 1954. The introduction of the flow-directed pulmonary artery catheter (PAC) in the 1970s permitted clinicians to measure intracardiac pressures directly. Hemodynamic data gathered from PAC use are widely used to diagnose and to help guide medical therapy in critically ill patients in the operating room, cardiac catheterization laboratory, and intensive care unit. Such data can be helpful in differentiating between cardiogenic and noncardiogenic shock and in guiding decision-making about fluid, vasoactive, and inotropic drug therapy over time. For the patient to benefit from PAC use, the clinician must thoroughly understand the interpretation and use of hemodynamic data and must be well aware of the limitations of data obtained from PAC use. Although pulmonary artery catheterization has not been proven to improve outcome, expert opinion continues to support its judicious use after evaluation of the potential risks and benefits for each patient (Pulmonary Artery Catheter Consensus Conference 1997).
HOW PAC TECHNOLOGY WORKS
The PAC is 100 cm long, with proximal and distal ports that enable the measurement of intravascular and intracardiac pressures and the sampling of blood as well as the infusion of vasoactive and inotropic drugs and fluids. At the very tip of the PAC lies the thermistor. The thermistor, when appropriately positioned in the pulmonary artery, continuously measures the temperature of the blood passing by the tip of the PAC in the pulmonary artery. Relatively cold (iced or room-temperature) fluid is injected into the right atrium via the proximal port of the PAC and decreases the temperature of the blood passing distally by the thermistor into the pulmonary circulation. A thermodilution curve is generated by plotting the decline in the pulmonary artery temperature against time in seconds. The area under the curve is integrated and then incorporated into the Stewart-Hamilton equation to yield the cardiac output (CO):
CO = [V × (Tb − Ti) × K1 × K2]/[∫ ΔTb(t)dt]
where V = volume of injectate, Tb = temperature of blood, Ti = temperature of injectate, K1 = density factor, K2 = computation constant, and ∫ΔTb(t)dt = integral of blood temperature over time. The computation constant is specific to the brand of catheter, and it incorporates specific variations in catheter dead space, approximate injection temperature, injection rate, heat exchange, and unit conversion. The greater the cardiac output the smaller the temperature change over time. Matching the constant with the correct volume (5 or 10 cc) and temperature (iced or room temperature) of injectate to be used is imperative. Dissection of this equation exposes a number of data points that, if inaccurately obtained, will result in a miscalculated CO, which may lead to an inaccurate diagnosis and a misguided therapy.
PLACEMENT AND RISK
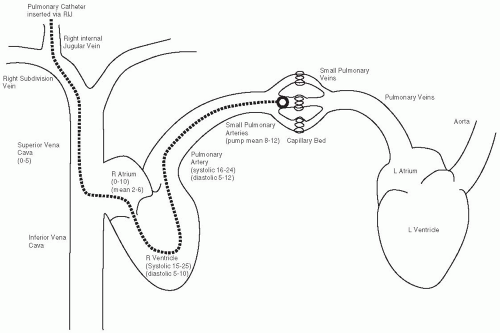
Assessing the overall risks and benefits of placing a PAC is important. Placing a PAC not only permits calculation of CO but also permits direct measurement of pulmonary-artery systolic, diastolic, and mean pressures and right heart filling pressures as well as indirect measurement of left ventricular filling pressures. Figure 93.1 depicts the correct path of the PAC through the right heart. An extra port in the PAC permits direct infusion of vasoactive and inotropic drugs into the central venous circulation.
Placing the large bore catheter that allows the introduction of the PAC into the central venous circulation poses risks for infection, pneumothorax, hemothorax, and bleeding at the puncture site or from disconnection of a line. Placing the PAC itself increases the risk for arrhythmia while the PAC floats through the right atrium and ventricle to the pulmonary artery. The most devastating complication associated with PAC use is pulmonary artery rupture. Although pulmonary artery rupture with hemorrhage is infrequent, with an incidence of 0.2%, it is associated with a mortality rate of up to 50%. The right pulmonary artery is involved in 93% of such cases, which usually affect the right lower or middle lobe branches.
ERRORS OF MANAGEMENT
Keep in mind that the thermodilution method measures pulmonary blood flow. Under normal circumstances, pulmonary blood flow equals systemic blood flow. The presence of intracardiac shunts, tricuspid regurgitation (TR), and cardiac arrhythmias, and rapid infusion of intravascular fluid can affect the accuracy of thermodilution CO measurements. The presence of a left-to-right shunt will yield a falsely high CO, because the pulmonary blood flow exceeds the systemic blood flow by an amount equal to the shunt from left to right. The presence of significant TR makes the CO calculations unreliable; it invalidates the thermodilution method, because a portion of the cold indicator continues to stay in the right atrium and right ventricle, therefore not producing a significant change in blood temperature. The
presence of cardiac dysrhythmias alters the beat-to-beat cardiac ejection, thereby yielding an inaccurate CO.
presence of cardiac dysrhythmias alters the beat-to-beat cardiac ejection, thereby yielding an inaccurate CO.
The accuracy of the CO calculation depends highly on operator consistency. Averaging at least three measurements made by the same operator yields the most reliable results, eliminating interoperator inconsistency and improving the precision of the CO calculation. The number of measurements averaged for each determination greatly affects the standard error of the mean (SEM), which is the basis for predicting reproducibility. There is a 2% to 5% variance in SEM when three measurements are averaged to calculate a single CO, and there is a 3% to 9% variance in SEM when only one measurement is used. When comparing CO over time and using three measurements per CO determination, a difference of 15% or more is needed to indicate that the results are actually different. If only one measurement per CO determination is used, then a difference of 26% or more is needed to indicate that the results are actually different. Therefore, at least three measurements should be done by the same operator and the average should be used to calculate CO.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree