Cardiac Emergencies
Luba Komar
Introduction
Congenital cardiac diseases often present in the newborn period and may require emergency management (see Chapter 11)
Other cardiac emergencies include arrhythmias, myocarditis, and pericarditis
Chest pain is uncommonly due to cardiac disease in children (< 5%)
Dysrhythmias
Tachyarrhythmias: heart rate faster than accepted normal range
Heart Rates in Normal Ranges
Age
Normal Range (bpm)
Mean (bpm)
0-3 mos.
90-180
140
3-6 mos.
80-160
130
6 mos to 1 yr
80-140
115
1-3 yrs
75-130
105
6 yrs
70-110
95
10 yrs
60-90
80
Narrow vs wide complex
Mechanisms: reentry, automaticity, or triggers
Narrow Complex Tachyarrhythmia
Most common tachyarrhythmia
Sinus Tachycardia
Most common tachycardia in children
Electrocardiographic Features
Causes of Sinus Tachycardia
Fever, hypovolemia (dehydration, blood loss), pain, sepsis, stress, poisoning, anemia, hyperthyroidism
Treatment of Sinus Tachycardia
Treat underlying cause—antipyretic, fluids, pain medication, etc.
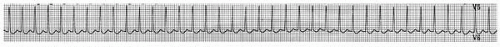
Supraventricular Tachycardia (SVT)
Rapid, regular rhythm
Often sudden onset
Most often caused by reentry mechanism that involves an accessory pathway
Usually well tolerated in most infants and children
May lead to congestive heart failure and cardiovascular collapse
Electrocardiographic Features
Heart rate > 220 in 60% of infants
Heart rate > 180 in children
P waves may be difficult to identify, P wave axis is abnormal
No beat to beat variability
Causes of Supraventicular Tachycardia
Wolff-Parkinson-White (22%)
Congenital heart disease (23%): corrected TGA, Ebstein’s anomaly, mitral valve prolapse, asplenia-polysplenia syndromes, post Mustard, Fontan, or ASD repair
Hyperthyroidism
Myocarditis
Drugs: sympathomimetics, caffeine, digitalis toxicity
Treatment of Hemodynamically Stable SVT
Resuscitation room, cardiac and saturation monitors
Initial 12-lead ECG, and continuous 12-lead ECG during cardiac conversion
Vagal maneuvers (62% successful, less successful in infants and younger children):
Ice (diving reflex): ice/water mixture in bag applied over forehead and eyes only for 15-20 seconds
Gag, carotid sinus massage, abdominal pressure, or Valsalva: ask older child to blow through straw, rectal stimulus (do not apply pressure to eyeballs)
IV access
Adenosine: 0.05-0.25 mg/kg IV/IO quick push, increase by 0.05 mg/kg q 2 min or 6 mg max first dose
Cardiology consultation to consider other medications including phenylephrine, neostigmine, verapamil, propranolol, esmolol, procainamide, digoxin
Esophageal overdrive pacing
ECG post conversion
Treatment of Hemodynamically Unstable SVT
ABCs
Synchronized cardioversion 0.25-1 J/kg, then 0.5-2 J/kg, max 10 J/kg
Note: cardioversion may not be successful in presence of hypoxia or acid-base imbalance
Cardioversion
Successful cardioversion or defibrillation requires passage of sufficient electric current through the heart
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree