27
Cardiac emergencies
Related anatomy and physiology
First-degree heart block (Fig. 27.22)
Second-degree heart block (Fig. 27.23)
Third-degree (complete) heart block (Fig. 27.24)
Introduction
Cardiovascular disease accounts for approximately 40 % of all deaths under the age of 75 years in Europe (Resuscitation Council (UK) 2011). One-third of all people suffering from myocardial infarction (MI) will die prior to reaching hospital, with a high proportion of these dying within one hour from the onset of symptoms (Resuscitation Council (UK) 2011) and approximately 15 % of those admitted will die within the first 30 days (British Heart Foundation 2010). Ischaemic heart disease is the leading cause of death in the world (Fuhrmann et al. 2008) and 50 % of men and 64 % of women who die suddenly of chronic heart disease do so without having had or recognizing any early warning signs (Williams 2009). More than 1.4 million people suffer from angina and 300 000 have MIs every year (Department of Health 2000) with up to 28 000 new cases of angina reported in the UK each year (British Heart Foundation 2010). Thus, Emergency Departments (EDs) will see a high proportion of patients suffering from a cardiovascular disorder.
Related anatomy and physiology
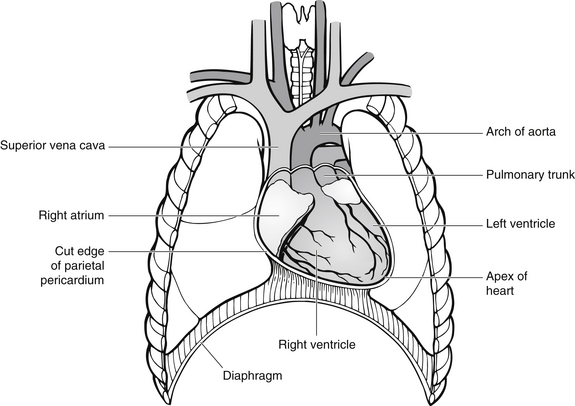
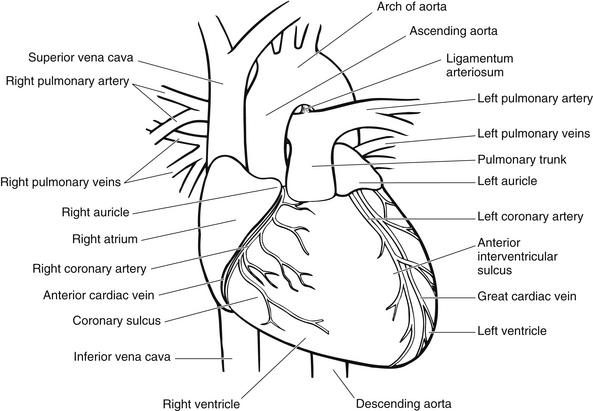
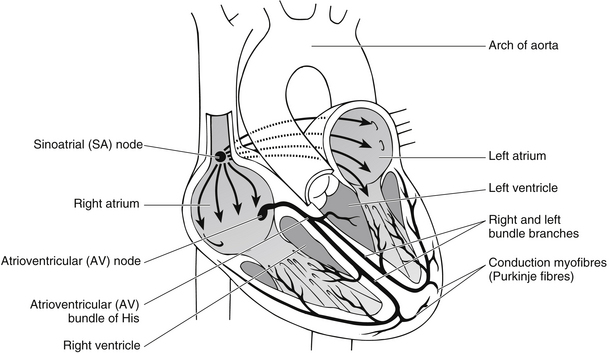
The heart can be described as a muscular pump containing four chambers, situated at an oblique angle in the mediastinal cavity (Tortora & Grabowski 2000) (Figs 27.1 and 27.2).
As the heart beats it expels blood into two closed circuits. The first circuit is fed from the left side of the heart. This supplies oxygenated blood from the lungs to the systemic circulation. The second circuit is the pulmonary circuit. This enables the right side of the heart to receive deoxygenated blood which is then pumped back to the lungs via the pulmonary artery (Marieb 2000).
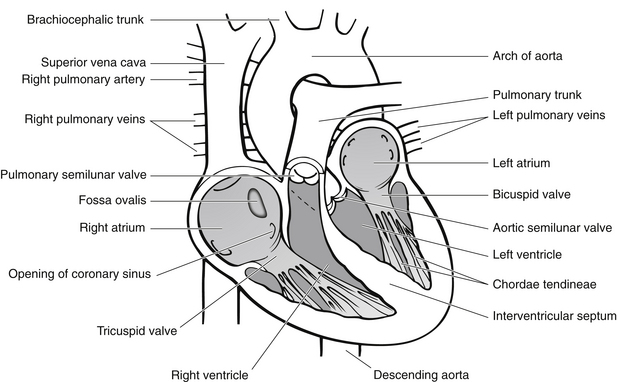
The heart is composed of a triple layer, which enables the protection of the inner components (Tortora & Grabowski 2000):
• the pericardium – the outer layer is composed of thick fibrous tissue that surrounds and protects the heart
• the myocardium – this is the muscular layer that forms the basis of the pumping action of the heart. It is present within both the atria and the ventricles, with the ventricles having the greater ratio of muscle
• the endocardium – this is composed of a thin layer of endothelial and connective tissue covering the inside of the heart, including the valves, which enables a smooth flow of blood through the heart, with little resistance.
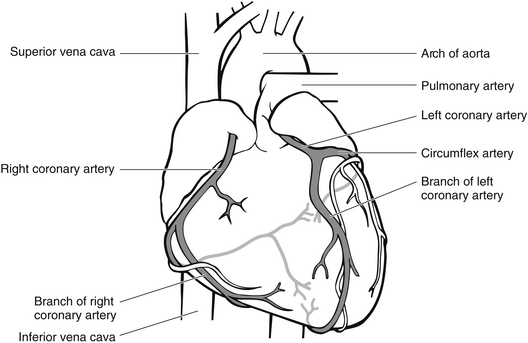
Coronary circulation
To maintain oxygenation and the supply of nutrients, the heart derives its own blood supply via the coronary arteries (Fig. 27.4). The left and right coronary arteries originate from the aorta. As suggested, they branch into a network of arteries supplying both the right and left sides of the heart.
The cardiac cycle
The cardiac cycle is divided into three main phases (Tortora & Grabowski 2000):
For simplification only the left side of the heart will be explained.
Ventricular relaxation
This follows ventricular contraction (systole). The ventricles relax, resulting in pressure within the left ventricle falling below that of the aorta, and thus the aortic valve closes. As Tortora & Grabowski (2000) indicate, all valves within the heart are now closed. At the same time, blood is passively flowing into the left atrium via the pulmonary system. As pressure and volume within the left atrium increase, the mitral valve opens and the second phase of the cardiac cycle is now entered.
Ventricular filling
Tortora & Grabowski (2000) identified that the ventricular filling phase of the cardiac cycle is divided into three stages. The first stage is referred to as rapid ventricular filling and involves passive filling of the left ventricle from the left atrium. The second stage of ventricular filling is known as diastasis and refers to slow ventricular filling. At the end of diastasis, the pressures in the left atrium and the left ventricle are now equal. The third stage of ventricular filling is due to the contraction of the atrium, with blood being forced into the left ventricle.
Assessment
The presenting history when a patient attends the ED with a cardiac event remains one of the most crucial aspects in aiding diagnosis. The history provides subjective information about the presenting complaint, symptoms, past medical history and any other relevant information (Castle 2009). During initial assessment, the patient’s need for immediate care must be paramount. Hence, the use of the ABC principle should be initiated automatically (Box 27.1).
The remainder of the assessment should include:
• assessment of patient’s appearance – this should include pallor, posture and any non-verbal signs
• pain assessment – location, type, site and severity of pain, including any measures taken to relieve the pain
• baseline observations – these should include blood pressure, pulse, temperature, respiration and oxygen saturation. Often temperature is forgotten, but the incidence of a mild pyrexia is a common response to muscle damage (Alexander et al. 2000)
• Electrocardiograph (ECG) – note any arrhythmia and use of cardiac monitor. (Note that it may be necessary to perform repeat ECGs on a patient whose condition changes, experiences further chest pain, or whom may have an evolving cardiac event.)
Clinical investigations
Clinical investigations to support assessment should include blood analysis (Box 27.2) and chest X-ray to determine heart size and detect oedema (Jowett & Thompson 2007). These blood tests, specifically the troponin/cardiac enzymes, may be repeated at defined times; normally between 6 and 12 hours past the initial onset of chest pain (Baliga & Eagle 2008).
Basic ECG interpretation
It is important for ED nurses to accurately record and interpret an ECG of a patient presenting with a cardiac condition. An inherent and rhythmical electrical activity is the reason for the heart’s continuous beating (Tortora & Grabowski 2000). The cardiac cells (myocardial cells) located within the myocardium undergo chemical changes, which in turn trigger electrical impulses (action potentials) and result in myocardial contraction.
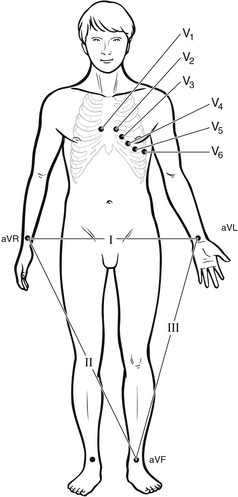
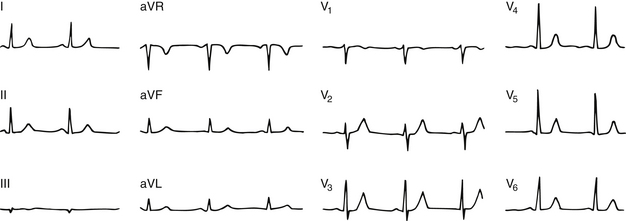
The normal heartbeat is known as sinus rhythm. In essence, this means that the impulses have been generated by the normal heart conductive system (Fig. 27.5). These electrical impulses can be recorded via an ECG. To obtain a 12-lead ECG, electrodes are placed across the chest and each limb (Fig. 27.6).
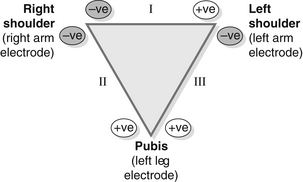
Having positioned the ECG electrodes, it is important to understand the representation being made by each electrode. The heart’s electrical impulses start at the SA node and depolarize down the conductive system as far as the apex of the heart. This directional flow is known as the cardiac vector. The four limb leads attached as shown in Figure 27.7 form what is known as the Einthoven triangle. The fourth lead not shown within the triangle acts as an earth and helps to standardize recordings. Leads I, II and III are known as bipolar leads, because each lead represents the electrical activity between two poles:
• lead I represents electrical activity from the right arm to the left arm
• lead II represents electrical activity from the right arm to the left leg
• lead III represents electrical activity from the left arm to the left leg.
The abbreviations for the unipolar leads are as follows:
• V – vector (force of direction of impulse)
• R, L, F – the direction being viewed, i.e., right, left or foot.
Thus, AVR looks at the right atrium (although in practice this is of little consequence), AVL looks at the lateral aspect of the heart, and AVF looks at the inferior aspect (Box 27.3). The chest leads are a much more simplified version for looking at the frontal plane of the heart. These are unipolar leads that pick up electrical activity from the point at which they are placed (Box 27.3):
• V1 is placed over the 4th intercostal space to the right of the sternum
• V2 is placed over the 4th intercostal space to the left of the sternum
• V1 and V2 thus view the anterior surfaces of the right and part of the left ventricles
• V3 is placed on the chest midway between V2 and V4; hence it is useful to apply V4 before V3. V3 looks at the septum
• V4 is placed on the fifth intercostal space, midway along the clavicular line, and views the septum and the anterior wall of the left ventricle
• V5 is placed along the same line as V4, but anteriorly to the midaxillary line
• V6 is again placed along the same line as V4 and V5, but rests on the midaxillary line
• V5 and V6 view predominately the lateral wall of the left ventricles.
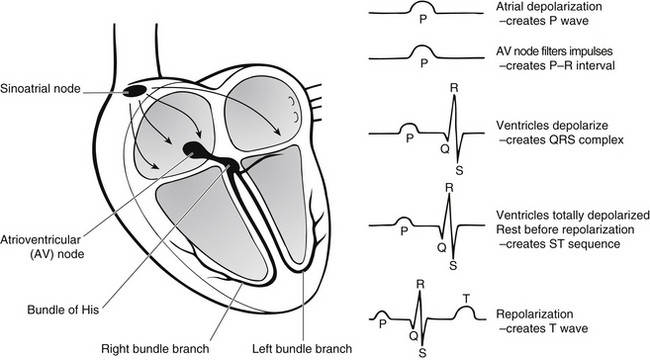
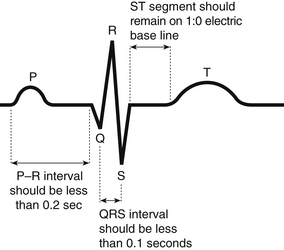
Components of a normal ECG
The ECG complex is made up of a sequence of electrical events occurring in the heart. The activity starts with impulses being transmitted from the sinoatrial node across the atria. As the atria depolarize, the P wave is created. The AV node filters and holds atrial impulses to allow significant ventricular filling time prior to contraction. This is represented as a straight line (isoelectric line) on the ECG and is called the P–R interval. As depolarization occurs through the bundle branches, and a wave of depolarization spreads across, the QRS complex is created on the ECG. This is followed by a short resting period, depicted again as an isoelectric line called the ST segment, before the T wave is created by ventricular repolarization (Fig. 27.8).
When this is all put together, a single heartbeat is represented in the ECG trace as shown in Figure 27.9.
Basic rhythm recognition
To make an accurate analysis of cardiac activity it is necessary to obtain a 12-lead ECG trace as opposed to a rhythm strip. The rhythm strip only shows one view of the heart that is dependent on the electrode positioning. As a result, myocardial damage or stress can easily be missed.
Once the 12-lead ECG has been obtained (Fig. 27.10), it is necessary to work through each lead methodically, looking at each waveform to ensure that any changes/abnormalities are recognized. To interpret an ECG, the ED nurse should start by looking at the rhythm strip to determine whether a basic rhythm is present. If a rhythm exists, complexes will be repetitive and components of those complexes will form the same pattern. It is also necessary to determine whether this pattern is occurring at regular intervals or not. Once an underlying rhythm is established, the rate of the rhythm should be determined (Evans 2007).
ECG tracings are standardized so that heart rate can be calculated from the tracing. Most ECG machines are set to pass paper through at 25 mm/s. As graph paper is standardized, one small square represents 0.04 s (1 mm of paper), one large square represents 0.2 s (5 mm of paper) and five large squares represent 1 s (25 mm of paper). Therefore, if there is one QRS complex per five large squares, the heart rate would be approximately 60 beats/min. Once an approximate rate is established, the nurse should look at the make-up of the repetitive complexes, checking whether the P waves are followed by the right length of interval and the QRS complex is followed by a T wave (Box 27.4).
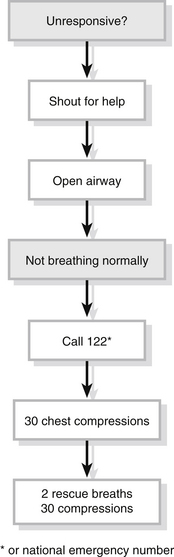
Cardiac arrest
Cardiorespiratory arrest can be defined as the sudden or acute cessation of the heartbeat and subsequently cardiac function, resulting in loss of effective circulation and respiration and therefore, incompatible with life (Evans 2007). There are numerous causes of cardiorespiratory arrest but there are only four cardiac rhythms an arrested patient will be in, they are:
Systemic management
In EDs, cardiac arrests in most instances are anticipated. Therefore, the ED nurse is responsible for (Alexander et al. 2000):
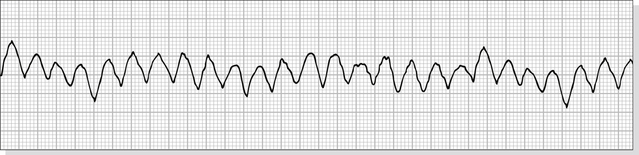
Ventricular fibrillation and pulseless ventricular tachycardia
The most common cause of cardiac arrest is usually VF or VT, which has an 80 % mortality rate for patients outside the hospital environment (Nolan et al. 2010) although women have a higher survival rate (Teodorescu et al. 2012). In VF, the cardiac cycle is disrupted and the cardiac cells behave chaotically, depolarizing in a disoriented and disorderly fashion or fibrillation (Fig. 27.12). As a result, cardiac output is compromised to the extent that blood circulation stops. This results in hypoxia, loss of consciousness within 10–20 seconds and absence of respiration. The physiology of VT is discussed later in this chapter. Simply put, the ventricular contractions occur at such a rate that ventricular filling time is inadequate and cardiac output is compromised. In severe cases, circulation ceases as in VF.
Immediate management
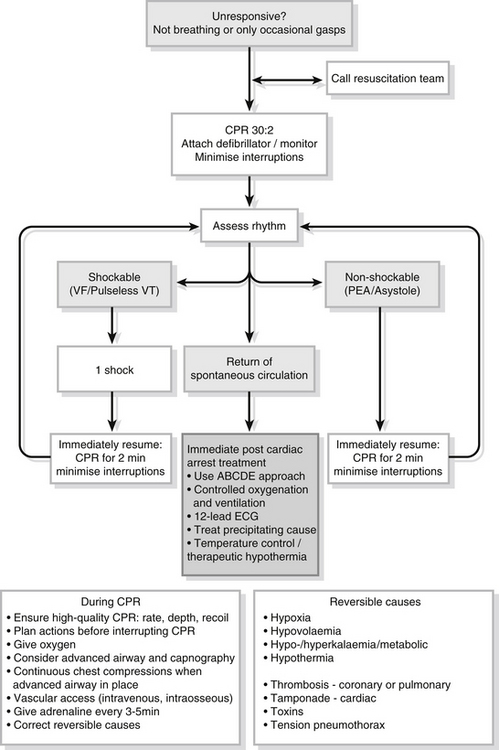
Cardiac arrest management has been standardized by the development of advanced life support (ALS) protocols (International Liaison Committee on Resuscitation 2005a, Resuscitation Council (UK) 2011). If the VF arrest is witnessed and monitored, a precordial thump may be of benefit in an attempt to ‘shock’ the heart and restore normal electrical activity; however it has a very low success rate for cardioversion of a shockable rhythm and is only likely to succeed if given within the first few seconds of the onset of a shockable rhythm (Haman et al. 2009, Pellis et al. 2009). It should never lead to a delay in getting a patient on to a defibrillator or being shocked (Resuscitation Council (UK) 2011). Potential complications of the precordial thump include rhythm deteriorations, such as rate acceleration of VT and asystole (Krijne 1984). A precordial thump is most likely to be successful in converting VT into sinus rhythm. Successful treatment of VT by precordial thump is much less likely (Resuscitation Council (UK) 2011). Having reviewed the evidence, the International Liaison Committee on Resuscitation (2005b) recommends one immediate thump may be considered after a monitored cardiac arrest if an electrical defibrillator is not immediately available.
The optimum first-line treatment for VF and pulseless VT is early defibrillation. The aim of defibrillation is to depolarize the myocardium simultaneously, to allow normal cardiac cell function to resume (Colquhoun et al. 1999). A key factor in reducing mortality lies with the speed of defibrillation, which should be given, safely, without delay (International Liaison Committee on Resuscitation 2005b). For this reason, ED nurses should be appropriately skilled in performing defibrillation as they are likely to be the first personnel in attendance. The resuscitation training officer for the ED should provide or ensure this training is given and updated yearly.
Defibrillation
Defibrillators used to require someone holding onto paddles and placing them on the chest; these have now all but been withdrawn, replaced by hands-free pad systems. Most EDs will have hands-free defibrillator systems. The pads or paddles of the defibrillator are positioned to enclose as much myocardium as possible (Fig. 27.13). A conductive medium, such as jelly pads, should always be used if older-style paddle defibrillators are used, both to enhance contact and to reduce skin damage. However, the widely used hands-free systems in most EDs have this gel component included already in the pads provided. Good contact with the chest is vital to maximize conduction and prevent ‘arcing’ of electrical current. If using the paddles, then they should be placed firmly over the jelly pads and perpendicular pressure should be applied (approximately 8 kg). If using the hands-free pads then the pads should be firmly pressed against the skin without kinks or folds and care should be taken to ensure nothing has become stuck between the pad and the patient. One pad/paddle should be placed to the right of the sternum, below the right clavicle in the mid-clavicular line, and the other vertically in the mid-axillary line, approximately level with the V6 electrode position or the female breast. This position should be clear of any breast tissue (Resuscitation Council (UK) 2011).
As even short interruptions to perform rhythm analysis causes significant interruptions in CPR and thus survival, the Resuscitation Council (UK) (2011) now recommends a single-shock strategy. The rationale is that with the first wave of biphasic waveforms exceeding 90 %, failure to terminate VF/VT successfully implies the need for a period of CPR to improve myocardial oxygenation, rather than a further shock. The Resuscitation Council (UK) (2011) notes that even if defibrillation is successful in restoring a perfusing rhythm, it is very rare for a pulse to be palpable immediately afterwards, and the delay in trying to palpate a pulse will further compromise the myocardium if a perfusing rhythm has not been restored (van Alem 2003). The SOS-Kanto study group (2007) found in witnessed out-of-hospital cardiac arrest, cardiac-only resuscitation improved survival rate.
The safety of the resuscitation team is paramount and it is the responsibility of the person administering DC shocks to ensure that other team members are clear of the patient. This should be ascertained verbally and visually before proceeding with defibrillation. ALS courses provide a standardized approach to training for all team members and should be a priority for ED nurses. These courses and updates are usually attained through a hospital’s resuscitation training department. The defibrillation regime should follow the algorithm shown in Figure 27.14.
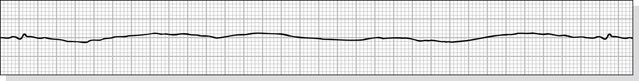
Asystole
This is total cessation of circulation, brought about by the lack of cardiac pacemaker activity, either natural or artificial (Colquhoun et al. 1999). Asystole accounts for 25 % of all cardiac arrests within the hospital environment (Jowett & Thompson 2007). The treatment is continued cardiac compression with ventilation. Adrenaline (epinephrine) and atropine are used to stimulate cardiac activity, but the prognosis for a successful resuscitation remains poor, with the overall survival rate being about 20–22 % of the survival rate compared with VF/VT rhythms (Resuscitation Council (UK) 2011) (Fig. 27.15).
Pulseless electrical activity (PEA)
This presents as a full QRS complex on the heart trace, but with the absence of any palpable pulse, hence the lack of systemic circulation. The causes are divided into the categories primary and secondary (Box 27.5).
For the resuscitation attempt to be of any success, the cause must be isolated and the appropriate treatment initiated, namely the non-VF/VT side of the algorithm shown in Figure 27.14.
Drug therapy
Pharmacological intervention may be used during cardiac arrest to (Jowett & Thompson 2007, Resuscitation Council (UK) 2011):
Adrenaline
Adrenaline (epinephrine) is the first drug used in cardiac arrest. Its therapeutic action is to improve coronary and cerebral perfusion. To date, substantial clinical evidence that adrenaline improves survival or neurological recovery in humans is absent (International Liaison Committee on Resuscitation 2005a), but some clinical findings have ensured that it has been continually used in arrests for the last 40 years (Resuscitation Council (UK) 2011). Adrenaline is an alpha- and beta-agonist and acts upon receptor sites to increase circulation to vital sites (Opie 2000). Its action in cardiac arrest is to cause vasoconstriction, increasing cerebral and coronary perfusion. Arrich et al. (2012) found, however, that an increasing cumulative dose of adrenaline during resuscitation of patients with asystole and pulseless electric activity is an independent risk factor for unfavourable functional outcome and in-hospital mortality.
Atropine
Atropine used to be recommended in the first-line treatment of arrests. However, the Resuscitation Council (UK) Resuscitation Guidelines (2010) no longer recommend its use for this purpose.
Ethical considerations
Whether the resuscitation is successful or not, thought and consideration for family or relatives must be a priority. Clear lines of communication must exist between medical and nursing staff and any family/friends. If the need to break bad news arises, ideally the doctor and the ED nurse should perform this, with one or the other actually breaking the news. More often than not these simple communication skills are forgotten (Box 27.6). A detailed discussion of this subject is given in Chapter 14.