Key Clinical Questions
Introduction
Abnormalities of calcium metabolism are common in hospital practice. Hypercalcemia has a prevalence of 0.1% in the general population and 1% among hospitalized patients. In the inpatient setting, hypercalcemia often portends serious illness, especially malignancy. Hypocalcemia is also common in the hospital, especially in patients with chronic renal failure or sepsis. Hypocalcemia may also be a manifestation of vitamin D deficiency, which has a prevalence of up to 80% on specialized geriatric inpatient units.
Calcium Metabolism
Precise regulation of calcium homeostasis is essential because calcium is critically involved in many physiological activities. It is the major mineral of bone. It also plays major roles in neuronal transmission, muscle contraction, and blood coagulation. Calcium is also required for the functioning of many enzymes, endocrine secretory processes, and biochemical signaling pathways.
A typical laboratory range for serum total calcium concentration is between 8.4 and 10.2 mg/dL. Approximately half of this total amount is bound to albumin, with the remainder in free (ionized) form. The normal free calcium concentration range is 4.5 to 5.3 mg/dL. A small fraction (10%) of circulating calcium is complexed with anions, such as citrate and phosphate.
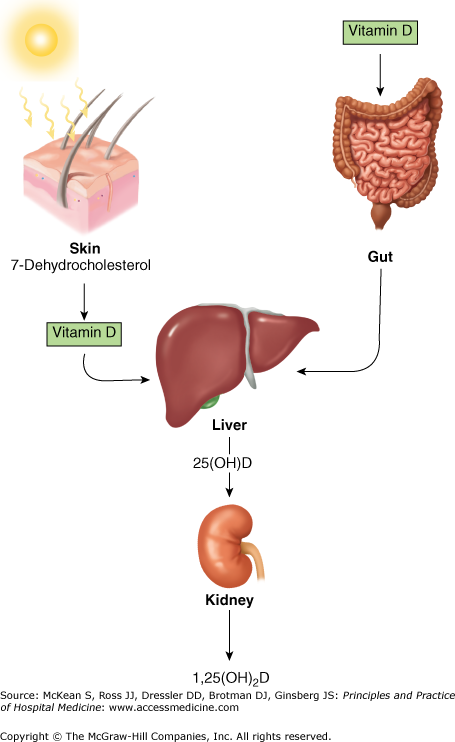
The three organ systems that together regulate serum calcium are the gastrointestinal tract, kidneys, and skeleton. The two principal regulatory hormones are parathyroid hormone (PTH) and 1,25-dihydroxyvitamin D3. PTH is a peptide hormone that is secreted from the parathyroid glands in its active full-length configuration, known as PTH(1-84). Its half-life in plasma is very short, on the order of 3 to 5 minutes. The major regulator of PTH secretion is the free calcium concentration in extracellular fluid. Elevated levels of free or ionized calcium promptly block secretion of PTH, while reduced serum calcium levels promptly increase secretion of PTH. 1,25-dihydroxyvitamin D3 is produced by a sequence of activation steps (Figure 247-1). It starts with the generation of cholecalciferol (vitamin D3) through exposure of skin to ultraviolet light of a specified wavelength (90–315 nm). Cholecalciferol or its plant analogue, ergocalciferol (vitamin D2) can also be obtained by dietary sources or in nutritional supplements. Cholecalciferol or ergocalciferol is converted in the liver to a hydroxylated form, 25-hydroxyvitamin D3 or 25-hydroxyvitamin D2. The hydroxylated forms of vitamin D are further activated to their final products by a second hydroxylation step in the kidney leading to 1,25-dihydroxyvitamin D2 or D3. Both dihydroxylated forms of vitamin D are active in human subjects, although there is controversy over whether vitamin D3 is more potent than vitamin D2. PTH maintains serum calcium concentrations by conserving calcium that has been filtered at the kidney glomerulus and by mobilizing calcium from bone. 1,25-dihydroxyvitamin D maintains serum calcium by facilitating absorption of calcium from the gastrointestinal tract and, like PTH, mobilizing calcium from bone. Under normal conditions, the amount of calcium absorbed in the gut (approximately 150–200 mg/d) is matched by the amount of calcium eliminated by the kidney. At the dynamic skeletal interface, as much as 500 mg of calcium is turned over daily. This process is in a steady state, with net calcium neither gained nor lost. Thus, under normal circumstances, there are no significant fluctuations in body calcium stores, nor is there any major change in circulating serum calcium concentrations.
Figure 247-1
Vitamin D synthesis and activation. Vitamin D is synthesized in the skin in response to ultraviolet radiation and is also absorbed from the diet. It is then transported to the liver, where it undergoes 25-hydroxylation. This metabolite is the major circulating form of vitamin D. The final step in hormone activation, 1-hydroxylation, occurs in the kidney. (Reproduced, with permission, from Fauci AS, Braunwald E, Kasper DL, et al. Harrison’s Principles of Internal Medicine. 17th ed. New York: McGraw-Hill; 2008, Fig. 346-4).
Changes in free or ionized calcium concentration are registered virtually instantly by parathyroid cells via the calcium-sensing receptor (CaSR). The receptor is located on the parathyroid cell surface, where its extracellular domain senses binding of calcium ions. The Ca2+-CaSR complex uses a G-protein coupled pathway to transmit the signal to the interior of the cell. Subsequent fluctuations in intracellular calcium stores regulate PTH gene transcription. If the circulating calcium concentration rises, the Ca2+-CaSR complex leads to a rise in intracellular calcium, inhibiting both PTH secretion and synthesis. If the serum calcium concentration falls, the Ca2+-CaSR complex sends a reduced signal to the cell, leading to an increase in PTH secretion and synthesis.
1,25-dihydroxyvitamin D decreases PTH production, although not as powerfully as does the ionized calcium signal. There is a stronger interaction between levels of 25-hydroxyvitamin D and PTH. Their relationship is an inverse one, with PTH levels rising when 25-hydroxyvitamin D levels fall below approximately 25–30 ng/mL. In turn, increased PTH stimulates the 1-alpha hydroxylase enzyme in the kidney that is responsible for the conversion of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D (Figure 247-2). When PTH levels are elevated (ie, primary hyperparathyroidism), 1,25-dihydroxyvitamin D levels increase. When PTH levels are low (ie, hypoparathyroidism), 1,25-dihydroxyvitamin D levels are typically low. The three organ systems (bone, gastrointestinal tract, and kidneys) and the two calcium-regulating hormones (PTH and 1,25-dihydroxyvitamin D) work together to maintain normal calcium homeostasis. When they are not perturbed by disease or by the aging process, they are an exquisitely sensitive and effective servomechanism.
Figure 247-2
Schematic representation of the hormonal control loop for vitamin D metabolism and function. A reduction in the serum calcium below 2.2 mmol/L (8.8 mg/dL) increases secretion of parathyroid hormone (PTH), mobilizing additional calcium from bone. PTH promotes the synthesis of 1,25(OH)2D in the kidney, which, in turn, stimulates the mobilization of calcium from bone and intestine, and regulates the synthesis of PTH by negative feedback. (Reproduced, with permission, from Fauci AS, Braunwald E, Kasper DL, et al. Harrison’s Principles of Internal Medicine. 17th ed. New York: McGraw-Hill; 2008, Fig. 346-5).
Laboratory Measurement of Blood Calcium
The measurement of serum calcium may be helpful when a disorder of calcium metabolism is suspected. However, there are many disorders of calcium metabolism, such as osteoporosis or Paget disease of bone, in which the serum calcium concentration is typically normal. Serum measurements may be performed by spectrophotometry or by atomic absorption spectrophotometry, with the latter yielding more accurate measurements. Spuriously high readings may occur if the tourniquet is in place too long before blood is drawn and hemoconcentration occurs. Under these circumstances, the measured serum calcium value can rise by as much as 0.4 mg/dL. On the other hand, the sample can read falsely low if the blood sample is obtained from a central, high-flow site via a central venous catheter. For most clinical situations, the total serum calcium is measured. This may need to be corrected for the circulating albumin concentration. For every 1 g/dL reduction in the serum albumin, the total calcium is adjusted upward by 0.8 mg/dL. This may be calculated as follows:
In theory, free or ionized serum calcium is a more accurate physiological measurement than the adjusted total serum calcium concentration, but the sampling technique (the blood has to be free-flowing and not impeded by a tourniquet) and strict anaerobic collection conditions are problematic. Moreover, the measuring instrument has to be in regular use and properly calibrated. Samples have to be measured immediately. These technical issues somewhat limit the clinical utility of the ionized calcium measurement.
Hypercalcemia
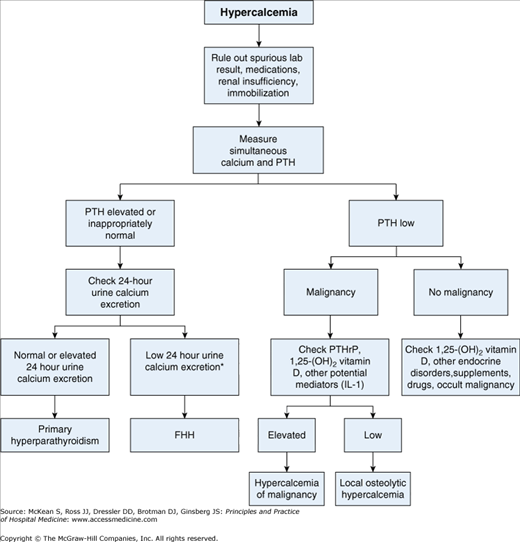
Signs and symptoms of hypercalcemia may be absent or subtle, except when calcium is significantly elevated or has increased rapidly. The diagnostic workup of hypercalcemia is usually straightforward (Figure 247-3) because two causes, primary hyperparathyroidism and malignancy-associated hypercalcemia, account for approximately 90% of cases. In addition, most individuals with primary hyperparathyroidism are asymptomatic and discovered on routine biochemical screening tests, while most individuals with malignancy-associated hypercalcemia have a known advanced malignancy at the time that hypercalcemia occurs. If the malignancy is not known, it is generally quickly apparent. When neither of these two etiologies is readily apparent, identification of the other potential etiologies requires a comprehensive history, physical examination, laboratory tests, and, occasionally, diagnostic imaging studies.
Many individuals with mild hypercalcemia (serum calcium level < 11 mg/dL) are asymptomatic, although some may report mild fatigue, vague changes in cognitive function, depression, or constipation. Symptomatic manifestations of hypercalcemia become more apparent when the serum calcium concentration is between 12 to 14 mg/dL. These symptoms include anorexia, nausea, weakness, and depressed mental status. As hypercalcemia may induce polyuria and nephrogenic diabetes insipidus, dehydration can occur should the compensatory polydipsia not be able to match urinary water losses. When serum calcium levels rise above 14 mg/dL, profound dehydration, renal dysfunction, and central nervous system changes, such as progressive lethargy, disorientation, and coma, may develop.
In addition to the absolute magnitude of the serum calcium elevation, the rate of increase in serum calcium also influences symptoms. Individuals who are chronically hypercalcemic may have relatively few symptoms, even with serum calcium values up to 15 to 16 mg/dL. In contrast, those whose calcium level has risen abruptly may have symptoms at much more modest calcium levels. Elderly or debilitated patients are more likely to be affected by hypercalcemia than younger individuals.
The medical record may contain clues to etiology. Prescription medications (Table 247-1), foods, and vitamin and nutritional supplements should be reviewed. A careful family history might uncover a familial endocrine condition. A history of family members with endocrine tumors of the pituitary or pancreas suggests multiple endocrine neoplasia type 1 syndrome (MEN-1). A family history of pheochromocytoma or medullary thyroid cancer is consistent with MEN-2 syndrome. Patients with sarcoidosis may have a history of unexplained fever, lymphadenopathy, skin rashes, or pulmonary symptoms. Bone pain suggests myeloma or other malignancies, although it may also be a nonspecific finding of hypercalcemia.
| PTH mediated |
|
| PTH-independent |
|
The physical examination is directed at identifying signs or symptoms of hypercalcemia. Evidence for dehydration such as orthostasis or dry mucous membranes may be present, although hypercalcemia has to be quite marked and prolonged for these physical findings to be appreciated. The physical examination is often normal in patients with hypercalcemia, especially if calcium levels are only modestly elevated. Rarely, severe and prolonged hypercalcemia may produce a visible horizontal deposit of calcium salts on the cornea, a finding called band keratopathy.
Effort should be made to identify signs of common causes of hypercalcemia, such as malignancy and primary hyperparathyroidism. The physical examination in primary hyperparathyroidism, like most hypercalcemic states, is usually not noteworthy. A mass is virtually never found in the neck, because enlarged parathyroid glands are still too small to be felt. However, when the serum calcium is markedly elevated, a neck mass may signify a parathyroid carcinoma. Symptomatic kidney stones might be accompanied by costovertebral tenderness. Enlarged lymph nodes suggest sarcoid, lymphoma, or metastatic carcinoma.
The first step in evaluating hypercalcemia is adjustment for serum albumin. If the corrected serum calcium is elevated, it should be repeated. Renal function should also be assessed, because hypercalcemia may develop or worsen in the setting of acute renal failure. If hypercalcemia is confirmed, the next step is measurement of serum PTH. The PTH level is the most important test for distinguishing between the two most common causes of hypercalcemia, primary hyperparathyroidism and malignancy-associated hypercalcemia (Table 247-1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree