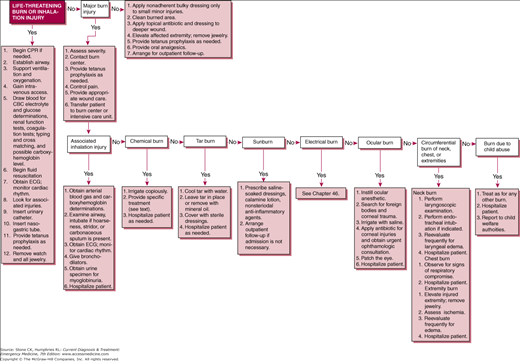
Immediate Management of Life-Threatening Problems
When any patient enters the Emergency Department, the first steps to care involve evaluation of the ABC’s—especially in burn patients. Severe burns to the lower face and neck may be associated with upper airway and laryngeal edema that cause airway obstruction. Inhalation of superheated air or steam in a confined space may also cause significant upper airway edema. Full-thickness chest wall burns, especially if they are circumferential, may limit chest wall movement and cause respiratory failure, requiring escharotomy on an emergency basis. Consider early endotracheal intubation in all patients with such injuries and in patients with stridor, hoarseness, or hypoxia.
Airway obstruction may progress rapidly in these patients. When the burn size exceeds 60% total body surface area, early endotracheal intubation should be considered as these patients often deteriorate rapidly. If facial or airway involvement is noted, intubation is advisable. If endotracheal intubation is not successful, cricothyrotomy or tracheostomy may be necessary.
Give oxygen by nasal cannula or face mask. If smoke inhalation may have occurred, give 100% oxygen by tight-fitting reservoir face mask or endotracheal tube. Monitor oxygen saturation by pulse oximetry, but be aware that pulse oximetry readings will be falsely elevated in patients with elevated carboxyhemoglobin levels. Simply subtract the measured carboxyhemoglobin level from the pulse oximetry value to determine the true oxygen saturation. Noninvasive co-oximetry is emerging as a useful tool to monitor the carboxyhemoglobin level in the ED.
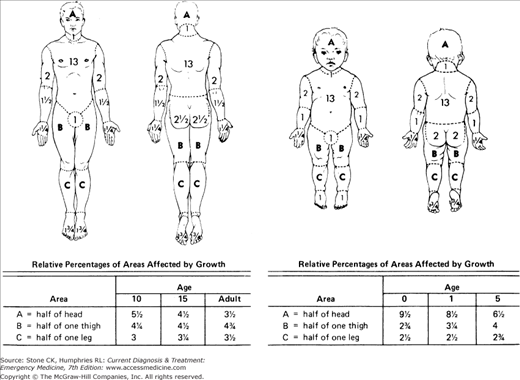
Patients with deep burns covering more than 15% of body surface area require intravenous fluid resuscitation. Insert one or two large-bore (≥16-gauge) peripheral intravenous catheters, preferably inserted through unaffected skin, or a central venous catheter if peripheral lines cannot be established. Calculation of the percent of body surface burned can be performed using an age-adjusted burn chart displayed in Figure 45–2. Additionally, the “Rule of Nines” can be used to estimate total burned body surface area, with each of the following representing 9%: head, anterior chest, anterior abdomen, each arm, anterior of each leg, and posterior of each leg. The back and buttocks represent 18%, while the groin and each palm represent 1%. Adjustment of the rule of nines for children changes 9% to 5%, with the head encompassing 20% of the total.
Burns are associated with the loss of large volumes of intravascular fluid, electrolytes, and protein through capillaries with increased permeability. Loss begins soon after injury and is maximal during the first 6–8 hours. Currently there is no universal consensus regarding fluid resuscitation and several formulas may be used as guidelines (Table 45–1). Studies comparing colloid to crystalloid solutions for resuscitation have not shown an increased benefit with colloids. Most burn centers today use only crystalloid for the first 18–24 hours, utilizing either the Parkland or modified Brook formula. These formulas should be individualized for each patient on the basis of the patient’s response to therapy, as well as the accepting physician’s preference if the patient is to be transferred to a burn center. Additional variables including body temperature, blood alcohol level, and inhalational injury may also affect the volume of fluid resuscitation required. In general, infusion rates should be adjusted to maintain urine output at 0.5–1.0 mL/kg/h for adults and 1.0 mL/kg/h for children under 10 kg.
| Formula | Day 1a |
|---|---|
| Crystalloid | |
| Parkland (Baxter) | 4 mL crystalloid × TBSA% × weight in kg |
| Modified Brooke | Using Lactated Ringers:
|
In the case of extensive burns over a significant body surface area, noninvasive blood pressure monitoring may be impossible due to interference of tissue edema with cuff readings. For these patients, a radial or femoral arterial catheter should be placed to accurately monitor blood pressure during resuscitation.
Arterial blood gas analysis is helpful if respiratory involvement is present. In addition, for assistance in overall patient management and resuscitation, submit blood for carboxyhemoglobin level, complete blood count, and electrolytes and urine for myoglobin. Obtain chest X-ray and electrocardiogram (ECG) and consider obtaining cardiac enzymes in the patient with suspected carbon monoxide poisoning.
Burn patients frequently have other injuries in addition to the burn. Patients who have been burned in motor vehicle accidents or explosions should be evaluated as described in Chapter 12. Consider cervical spine and other traumatic injuries in patients who may have jumped or fallen from a burning building or been burned in a motor vehicle crash.
An indwelling urinary catheter is the most important monitoring device in burn patients to monitor urinary output and to obtain urine for urinalysis (including myoglobin determination if the patient has sustained an electrical burn). Patients with full-thickness burns of the penile glans or shaft may require suprapubic cystostomy.
Patients with deep burns covering more than 20% of their body surface will develop an ileus. Inserting a nasogastric tube will decrease the risk of emesis and possible aspiration.
1This chapter is a revision of the chapter by David A. Fritz, MD, FACEP, from 6th edition.
Further Evaluation of the Burn Patient
Once initial resuscitation efforts have begun, additional information is often required to determine the disposition of the burn patient. Ask the patient, witnesses, and family about the mechanism of injury (eg, explosion, spilled liquid, house fire) and about the possible presence of combustibles known to be toxic. Find out whether the patient was burned in an open or enclosed space; the latter increases the risk of inhalation injury and should prompt consideration of early intubation. Also ask about underlying medical problems, tetanus immunization status, and medication allergies.
An accurate estimate of the severity of injury is crucial in determining the need for hospital admission or referral to a burn center and in guiding initial fluid resuscitation and establishing a prognosis. In general, patients with minor burns may be managed as outpatients, patients with moderate uncomplicated burns should be hospitalized, and patients with major burns should be transferred to a burn center. Even in the absence of major burn criteria, if the hospital does not have facilities or expertise in caring for burn patients, victims with moderate or major burns should be referred to a burn center. The following factors are used to determine burn severity.
Accurate measurement of the burned area, expressed as a percentage of body surface area, should be performed in all burn patients. Burn size may be quickly estimated by using an age-adjusted surface area chart (see Figure 45–2) or by using the “rule of nines” as mentioned earlier in this chapter. The size of scattered small burns can be estimated by comparing them with the size of the patient’s hand, which constitutes about 1.25% of body surface area. The extent of all burns should be recorded on a drawing (front and back views) on the patient’s chart.
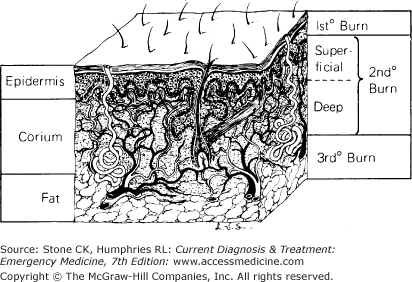
Burns are typically described as first, second, third, or fourth degree. A more useful description, based on the wound’s ability to heal, is partial thickness (heals spontaneously) and full thickness (requires skin grafting). Deep partial-thickness burns usually require grafting to expedite healing and decrease contractures and hypertrophic scar. Figure 45–3 shows the level of skin involved with each type of burn. Table 45–2 outlines the physical findings usually associated with each type of burn. The depth of burn should be recorded accurately on a drawing (front and back views) on the patient’s chart.
| Depth of Burn | Color and Appearance | Skin Texture | Capillary Refill | Pain/Pinprick | Healing | |
|---|---|---|---|---|---|---|
| 1st degree | Superficial epidermis | Red | Normal | Yes | Yes | 5–10 days; no scar |
| 2nd degree | Superficial partial thickness | Red; may be blistered | Edematous | Yes | Yes | 10–21 days; no or minimal scar |
| Deep partial thickness | Pink to white | Thick | Possibly | Possibly | 25–60 days; dense scar | |
| 3rd degree | Full thickness | White, black, or brown | Leathery | No | No | No spontaneous healing |
| 4th degree | Involves underlying subcutaneous tissue, tendon, or bone | Variable | Variable | No | No | No spontaneous healing |
Several principles must be kept in mind when considering burn depth. First, because it is difficult to distinguish deep partial-thickness burns from full-thickness burns, these burns should be assumed to be full-thickness injuries and should be treated accordingly. Second, burn wounds change over 48–72 hours, and what may appear to be superficial injury on initial examination may progress to a deeper-level injury, especially if the patient has poor perfusion or the wound becomes desiccated or infected.
Burns in the following areas are considered major injuries:
Deep burns of the hands or feet cause scarring and may produce permanent disability.
Partial- or full-thickness facial burns may cause severe scarring, with profound physical and emotional impact. They are also often associated with inhalation injury and compromised airway.
Burns of the eyes may cause corneal scarring and eyelid dysfunction that may ultimately lead to blindness. Note: Patients with possible eye burns should be examined as quickly as possible, preferably in the emergency department, because massive periorbital edema often develops and hinders later examination. Further discussion of eye injury is detailed later in this chapter.
Deep burns of the ears predispose to development of pressure deformity and infection. Examine the tympanic membrane in patients with external ear injuries caused by hot liquids or chemicals. Burns associated with electrical injury, including lightning strikes, also require examination of the tympanic membrane. A high incidence of rupture occurs with this mechanism of injury.
Burns of the perineum are difficult to manage on an outpatient basis and are more susceptible to infection than are other types of burns.
Any deep circumferential burn is a potential major injury. Circumferential deep burns of the neck may cause lymphatic and venous obstruction that leads to laryngeal edema and airway obstruction. Circumferential burns of the extremities may restrict blood flow, causing an increase in tissue pressure and ischemia. Circumferential chest wall injuries may impede chest wall movement and lead to respiratory failure.
Inhalation injury signifies a major burn. Signs and symptoms suggestive of inhalational injury include burns sustained in a confined space, singed nasal nares, soot around the nares, carbonaceous sputum, hoarseness, stridor, respiratory distress, and a carboxyhemoglobin level >10%. Diagnosis and management of inhalation injuries are discussed below.
Damage from electrical injury may be extensive, even though the outward signs of injury are minimal. Cardiac arrhythmias and renal failure from myoglobinuria are possible complications. Electrical currents as little as 100 milliamps can cause ventricular fibrillation. All electrical injuries should be considered major injuries.
The mortality rate from burn injury is increased in very young or very old patients; these are also the age groups in which burns most commonly occur. Burns in a child younger than 5 years or in an adult older than 55 years are more likely to be serious than are burns in other age groups.
Burns may occur in patients with other injuries, such as fractures or internal injuries due to vehicular accidents, falls, or explosions. The associated injuries often place the patient at increased risk of serious complications or death, even though the burns themselves are small.
Major pre-existing medical problems in a burn patient are associated with an increased rate of serious complications and death. Any pre-existing condition that prevents normal healing puts a patient with even minor burns at risk for complication. Patients with a history of myocardial infarction, angina, significant pulmonary disease, diabetes mellitus, or renal failure are considered poor-risk patients even if their burns are not serious. Burned patients with a history of alcohol or other drug abuse are also at higher risk for complications following burn injury.