Burns and Smoke Inhalation
Roger W. Yurt
James J. Gallagher
Joy D. Howell
Bruce M. Greenwald
KEY POINTS
 Initial evaluation of the patient includes determination of depth of injury and extent of surface area involved. These are trauma patients and may have other injuries in addition to the burn.
Initial evaluation of the patient includes determination of depth of injury and extent of surface area involved. These are trauma patients and may have other injuries in addition to the burn. Fluid resuscitation in the first 24 hours is based on a formula to calculate the amount of lactated Ringer solution to infuse. The formula is only a guide; adjustments are made on the basis of vital signs and urine output.
Fluid resuscitation in the first 24 hours is based on a formula to calculate the amount of lactated Ringer solution to infuse. The formula is only a guide; adjustments are made on the basis of vital signs and urine output. Silver sulfadiazine is the topical agent most commonly used for burn wounds. Early excision of the wound is now standard of care in the burn-injured patient.
Silver sulfadiazine is the topical agent most commonly used for burn wounds. Early excision of the wound is now standard of care in the burn-injured patient. Hypermetabolism is very prominent in the burninjured child. Proteins and calories must be provided to address these needs, beginning on the day of injury. Hypermetabolism persists for 9-12 months postinjury.
Hypermetabolism is very prominent in the burninjured child. Proteins and calories must be provided to address these needs, beginning on the day of injury. Hypermetabolism persists for 9-12 months postinjury.The derangements of physiology that occur after major burn injury in a child are among the most challenging problems in modern medical care. The loss of skin integrity exposes the child to the exterior environment of bacterial, fungal, and viral pathogens. At the same time, the wounds provide a portal for loss of fluid and body heat. Beyond these local changes are the systemic responses that further stress the homeostatic mechanisms that usually maintain a stable internal environment for the patient. This chapter addresses the evaluation and care of the child with a major burn, electrical injury, and/or smoke inhalation injury. Information will also be provided regarding lesser wounds, as it is not uncommon for patients to present with multisystem injury in addition to their burns.
EVALUATION OF THE PATIENT
The distraction created by the appearance of large areas of blistering, tissue loss, and disfigurement associated with a burn injury can lead to a fixation on that injury and a lack of  recognition that burn-injured patients are trauma patients. In that regard, initial evaluation should be the same as for any patient who has sustained injury. Thus, the ABCs of ensuring adequacy of an airway, that the patient is ventilating, and that circulation is intact must be addressed. A rapid overall evaluation of the patient is performed as resuscitation is initiated. The specific details of evaluating a child with burn injury will be addressed here. The aspects of evaluation of additional traumatic injury are addressed in Chapter 30.
recognition that burn-injured patients are trauma patients. In that regard, initial evaluation should be the same as for any patient who has sustained injury. Thus, the ABCs of ensuring adequacy of an airway, that the patient is ventilating, and that circulation is intact must be addressed. A rapid overall evaluation of the patient is performed as resuscitation is initiated. The specific details of evaluating a child with burn injury will be addressed here. The aspects of evaluation of additional traumatic injury are addressed in Chapter 30.
 recognition that burn-injured patients are trauma patients. In that regard, initial evaluation should be the same as for any patient who has sustained injury. Thus, the ABCs of ensuring adequacy of an airway, that the patient is ventilating, and that circulation is intact must be addressed. A rapid overall evaluation of the patient is performed as resuscitation is initiated. The specific details of evaluating a child with burn injury will be addressed here. The aspects of evaluation of additional traumatic injury are addressed in Chapter 30.
recognition that burn-injured patients are trauma patients. In that regard, initial evaluation should be the same as for any patient who has sustained injury. Thus, the ABCs of ensuring adequacy of an airway, that the patient is ventilating, and that circulation is intact must be addressed. A rapid overall evaluation of the patient is performed as resuscitation is initiated. The specific details of evaluating a child with burn injury will be addressed here. The aspects of evaluation of additional traumatic injury are addressed in Chapter 30.Extent of Burn Injury
The extent of tissue injury caused by a burn is quantified by the surface area (SA) and the depth of injury. Determination of the extent of injury provides a basis for estimation of fluid requirements for resuscitation and for determining an overall care plan. In addition, in that a positive correlation exists between extent of injury and mortality, this determination provides information on prognosis. For estimation of the extent of SA involved, a Lund & Browder chart or Berkow’s formula should be used. The “rule of nines” cannot be used in children <15 years of age. The distribution of SA by age is shown in the chart in Table 32.1.
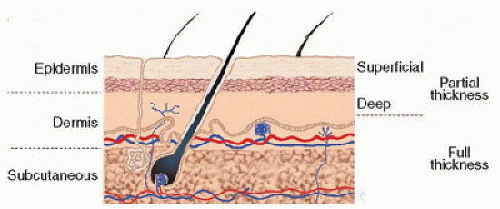
Evaluation of depth of injury is readily determined at the extremes of depth, such that partial-thickness injury is easy to differentiate from full-thickness injury. A first-degree burn is characterized as erythematous, painful, and dry, while a thirddegree burn, also known as a full-thickness burn, is leathery, dry, and insensate. Burn injuries at an intermediate depth of partial thickness are more difficult to assess. They are divided into superficial and deep partial-thickness wounds. Whether superficial or deep, these wounds appear very similar on physical examination. They are erythematous, moist, and sensate. Evaluation of these wounds is complicated by the fact that
they evolve over time, are frequently not homogeneous with regard to depth, and dynamically change over the first days after injury. Previous attempts to use advanced instrumentation, such as laser Doppler and infrared sensing devices, did not demonstrate proven value in routine evaluation of this depth of injury. However, a more recent report suggests that laser Doppler imaging may be useful in estimating depth of injury in children (1). The importance of differentiating depth of injury relates to the fact that a superficial partial-thickness burn will reepithelialize in 2 weeks, whereas a deep partialthickness wound heals by epithelialization and contraction. To avoid scarring, the deeper wound must be treated by skin grafting. Except for small-SA wounds, full-thickness wounds should either should be excised and closed primarily or grafted with the patient’s skin. A cross section of skin with indication of the various depths of injury is depicted in Figure 32.1.
they evolve over time, are frequently not homogeneous with regard to depth, and dynamically change over the first days after injury. Previous attempts to use advanced instrumentation, such as laser Doppler and infrared sensing devices, did not demonstrate proven value in routine evaluation of this depth of injury. However, a more recent report suggests that laser Doppler imaging may be useful in estimating depth of injury in children (1). The importance of differentiating depth of injury relates to the fact that a superficial partial-thickness burn will reepithelialize in 2 weeks, whereas a deep partialthickness wound heals by epithelialization and contraction. To avoid scarring, the deeper wound must be treated by skin grafting. Except for small-SA wounds, full-thickness wounds should either should be excised and closed primarily or grafted with the patient’s skin. A cross section of skin with indication of the various depths of injury is depicted in Figure 32.1.
TABLE 32.1 DISTRIBUTION OF BODY SURFACE AREA BY AGE AS PERCENTAGE OF TOTAL BODY SURFACE AREA | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Types of Injury
The depth of the injury in burns that are caused by scalding, flame, or contact with a hot object is directly related to the temperature, duration of exposure, and thickness of the tissue. Three zones of injury have been identified in burn-injured skin. The outer zone of coagulative necrosis includes necrotic tissue that is irreversibly damaged by heat or chemical. Below that is the zone of stasis in which some viable tissue remains. This dynamic region is subject to further necrosis if it is not protected from further physical damage. Care must be taken to avoid aggressive methods of debridement and harsh cleansing agents. In addition, delivery of nutrient blood flow and oxygen is important in this region, and compromised cardiac output due to inadequate resuscitation can increase the depth of injury. The zone adjacent to the zone of stasis is the zone of hyperemia, and is characterized by increased blood flow and local inflammatory response to the injury.
Chemical burns cause denaturation of protein and disruption of cellular integrity. The degree of injury is dependent on the time of exposure, the strength of the agent, and the solubility of the agent in tissue. Alkaline agents tend to penetrate deeper into tissues than do acids, with an exception being hydrofluoric acid, which penetrates lipid membranes readily.
Electrical injury accounts for 2%-3% of the burns in children that require evaluation in an emergency department (2). Electricity is the flow of electrons, the force (or gradient) behind the flow is the voltage, the volume of the flow is the current measured in amperes, and the resistance to that flow is measured in ohms. Electrical injury can occur from direct contact or by an arc such as a lightning strike. Direct contact often causes damage at the entry and exit sites and along the path of the current. Arcs associated with high voltage can be extremely hot and cause deep thermal burns at the entrance site as well as current injury along the path. Domestic electricity in North America ranges 120/240 V. Low voltage is defined as <500-1000 V and is usually associated with less morbidity (less tissue injury from burns or blunt trauma) if there is no cardiac or respiratory arrest. Electricity occurs in two forms, alternating current (AC) where the current flows back and forth, and direct current (DC) where flow is in one direction. AC is in common use in North America and standardly runs at 60 cycles per second or 60 Hz (3). Battery power and lightning are examples of DC current. AC is more dangerous at a given voltage because of its ability to produce a tetanic muscular contraction that can prevent the victim from letting go and prolong the contact with electricity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree